Page Synopsis: We neither know what causes CFS nor how to treat it (though hopefully this site has ameliorated that situation!), therefore the cause (and hence the cure(s) are likely hiding on this page (or perhaps in one of the 10,000 links at the bottom of the page). By allowing the titles or actual pages spark your investigative imagination, perhaps you will notice something that others haven't, (leading to lines of inquiry towards discoveries which offer relief to millions of not so patient patients)
Skill Level 2
Relevance:2 Technical Level:3
page 75 FURTHER RESEARCH LINKS
page 74
page 76
There's a patent for a CFS drug 'Treatment of chronic fatigue syndrome and fibromyalgia syndrome https://patents.google.com/patent/WO2002043737A1/en Chronic fatigue syndrome (CFS) and fibromyalgia syndrome (FMS) can be treated by the administration of Δ5-androstene-3β-ol-7,17 dione and metabolizable precursors thereof.
Classifications
A61K31/5685 Compounds containing cyclopenta[a]hydrophenanthrene ring systems; Derivatives thereof, e.g. steroids not substituted in position 17 beta by a carbon atom, e.g. estrane, estradiol substituted in positions 10 and 13 by a chain having at least one carbon atom, e.g. androstanes, e.g. testosterone having an oxo group in position 17, e.g. androsterone
![]()
From an interview with Maija Haavisto in describing potential treatments which have helped her or her website forum users
"Various probiotics, Glutathione, N-Acetyl Cysteine, methylation cycle treatments, MAF 314, IV saline solution, Gamma Globulin injections/IV, Lidocaine IV, Valtrex, Valcyte, Ergoloid, Levofolinic Acid, Nifedipine, Galantamine, Ampligen, Bromocriptine and Selegiline"
Investigate topics including
- fluoride sensitivity
- Cyclosporine
- dentaltests
- hypopituitary
- Iodine Protocol
- PQQ
Things that have had dramatic beneficial effects on at least one person on my forum, besides the LDN, include e.g. L-carnitine, D-ribose, methylfolate, wild vegetables, gluten-free diet, ozone therapy, oral saline, beta blockers, sumatriptan (for all symptoms), tramadol (similarly), modafinil, hydrocortisone, amitriptyline, fluoxetine, clonazepam, prednisone, testosterone, IVIG, nimodipine, antibiotics, Epicor, benfotiamine, astragalus, berberine, cat’s claw and inosine. Bromelain is great for post-exertional muscle soreness. As with meds, there are supplements that may carry a lot of promise, but hardly anyone uses them.
NMDA antagonists, GH deficiency, I’m also taking most other pituitary and related hormones except for testosterone – glucocorticoids, mineralocorticoids, estrogen, progesterone, DHEA, desmopressin, T3 and T4. I might start oxytocin, too
My Finnish doctor uses supplemental oxygen, which several of my friends have tried and feel it is very helpful. Ozone therapy may have use in some cases. A friend benefited a lot from neurofeedback. Acupuncture may help some. My Dutch doctor uses intermittent hypoxia
It has turned out that I’m helped a lot by progesterone. It’s quite a surprise, as I was hoping to
improve on estrogen, but didn’t really expect anything fromprogesterone – it’s just “something that has to be taken if you take estrogen” (which doesn’t seem to do anything). But progesterone helps my hypoglycemia and makes my breathing easier and physical stamina better. Sadly, it’s supposed to be taken cyclically. I’m on a break after 11 days and my blood sugar just won’t stay up at all
For sleep I use a combination of melatonin, baclofen and Sophora flavescens. B12 and methylfolate help that too. But the most important thing for my sleep is adequate hormones. For example, low cortisol used to mean not sleeping more than one hour a night
I know of another person with ME/CFS who did very well on progesterone (but not on estrogen). She found out about progesterone by visiting forums for another disease group. How did you find out about progesterone?
I went to a Belgian clinic after I asked my Dutch CFS/ME doctor if he could prescribe me growth hormone and he said he wouldn’t, but the clinic probably would. Which they did – they use it quite often. I was already taking various hormones, but based on my symptoms, lab tests and a physical exam they added estrogen, progesterone, the GH (and changed some of my existing hormone prescriptions
They said estrogen deficiency is one of my main problems and behind my severe hair loss (I had figured out I was deficient in estrogen, but didn’t connect it to the hair loss – time will tell whether they’re right), but they didn’t really mention anything about progesterone.
I don’t really view myself as taking it for CFS/ME (but progesterone deficiency from hypopituitarism), but of course it’s hard to say for sure which symptom comes from which problem. But I doubt I’d have never specifically asked for progesterone.
I’ll have to ask if there’s any chance I could take progesterone all the time. After all with the mini pill women are taking only (synthetic) progestagens without any breaks
After you discovered LDN and nootropics such as nimodopine and piracetam your productivity increased greatly. You were able to put in 15 hour days but then you experienced a sudden acute stress that wiped your pituitary out and your ability to work – not to exercise – but to do the kind of mental work you were so good at before plummeted. Did you have any indication prior to that that your system was weakening or was your collapse an out-of-the blue type thing?
No, I was doing just fine. Though I’ve had minor instances of worsening hypopit, e.g. in March 2009 (I’ve been dependent on corticosteroids since), June 2012 and August 2012, where I’ve had some preliminary symptoms. For the first two there was no obvious serious stressor, the last one followed a trip to Berlin with temperatures reaching 37C.
In the first and last instance I had a sudden sensation of feeling inexplicably good for a few hours the day before the problem got worse. In the second instance I suddenly started feeling extremely thirsty, like I could drink an ocean. I wasn’t very surprised when my diabetes insipidus got permanently worse after that. (Normally diabetes insipidus does not make me thirsty
30-50 mgs of Testosterone Propionate injected every
other day (EOD) is an excellent option and my recommended
protocol for long term TRT administration.
left off pg 76
For full report please see 'Treatment Protocols' https://bra.in/2joB5q
Listing of therapies click hereListing of therapies, protocols, drugs and supplements (in order of average effectiveness as reported by takers of a 'curetogether' poll) http://curetogether.com/Chronic-Fatigue-Syndrome/treatments/ae/ Take frequent short rest breaks (559) Spend time in low-stimulation environment (198) Rest (572) Personal development (e.g. learn to say 'no', care less about opinion others, letting go of shoulds and musts, acceptance, become more relaxed and balanced) (450) Wheelchair (66) Ignore people who think ME/CFIDS is not real (363) Low-Dose Naltrexone (LDN) (89) Avoid biotoxins (82) Complete stillness & quiet (154) Diet changes (509) Avoid known allergens (149) Meditation (343) Gluten-free diet (250) Eliminate/ reduce sugar (399) Change job (212) Adequate rest (49) Avoid alcohol (442) Methylation treatments (74) Adequate sleep (49) Yeast treatments (125) T3 (58) "Recuperation" (55) Relaxation techniques (156) Avoid mold (168) Mindfulness (141) Eliminate/ reduce dairy (366) Perrin Technique (10) Inverting body position (with head down and feet up eg on a couch) (180) High Dosage VegEpa (EPA+EPO) (15) Do absolutely Nothing (168) B12 injections (205) Anti-yeast diet (65) Inner Spirit Therapy (12) Diaphragmatic breathing (221) Far Infrared Heat (Migun Bed) (58) Go to bed early and sleep longer (448) Marijuana (6) Massage (371) Thyroid hormone (59) Probiotics (402) Stay well-hydrated throughout the day (469) Oxytocin (20) Beta Blockers (for OI) (15) ketogenic diet (10) Betahistine (3) Physiotherapy (Connective Tissue Release) (6) Revitalizing Sleep Formula (14) Mobic (14) Energy Revitalization System vitamin powder (14) paleo/primal diet (22) Magnesium (oral) (374) Gupta Amygdala Retraining (49) Reiki (39) SHINE Protocol-Dr. Teitelbaum (23) Ayurveda (37) Orthomolecular Therapy (18) Chelation treatments (49) Lymphatic Massage (61) Sinus Surgery (6) Qigong (53) Co-codamol (27) Eat more vegetables and fruits (467) Liposomal Glutathione (31) vegetarian diet (19) horseback therapy (4) Lithium orotate (4) Atlas Profilax (4) Emotional Freedom Technique (EFT) (68) EECP (1) Adya Clarity Shots (1) bowel removal for cancer (1) MAF 878 (1) clarithromycin & hydroxychloroquine (1) Nicotinamide Riboside (1) carbidopa/levadopa (1) Clonazepam (Klonopin, Rivotril) (167) Stretching (414) Diflucan\--antifungals (33) Crystal Light Therapy (5) B vitamins (458) Cranio-Sacral Therapy (94) in-home treatment mobility exercises (2) ketotifen (2) fluefenazine/nortriiptiline clorhidrate (2) Proamatine (2) Earthing (18) Xanax (alprazolam) (92) Nexavir (9) Nystatin (22) Antivirals (84) carnitine (6) Theta Healing (6) Adrenal Stress End (16) Robaxin (3) Interferential TENS (13) Cordyceps (13) Sinus Treatments (Nasonex, etc) (66) Betaine-HCl (67) Transfer Factors (7) Malic Acid (153) Antihistamines (drowsy / first generation) (14) Stimulants (dextroamphetamine, amphetamine, Adderall, etc) (96) Horizant (1) alpha - gpc (1) Siffrol (1) Kavinace (1) Mirapex (1) Nimodipine (1) Aqua Flora for yeast (1) Azilect (1) desmopressin (1) Ampligen (8) Rebreathing carbon dioxide (8) Myer's Cocktail (43) Magnesium (topical) (76) Electrolyte beverage (eg. gatorade) (170) Guainfenesin (59) Rheumatrex, Trexall (methotrexate) (9) NAET for allergies (9) Acetyl-L-carnitine (166) Osteopathy (76) Pinecone Extract (ImmunExtra) (6) Vitamin D (424) Reverse Therapy for CFS (10) Baclofen (29) Ibuprofen (Advil, Motrin) (384) IVIg infusions (4) Zeolith (4) Famvir (4) Red Marine Algae (8) Theanine (16) Neurofeedback (28) Testosterone (94) Sublingual B12 (212) Root canal/cavitation removal (107) thyroid operation (1) MCT oil (1) ice baths (1) Phenocane (1) NAC (42) Hypnotherapy (26) Glucosamine/Chondroitin (84) Mushroom Extracts (AHCC, Shitaake) (18) Specific Carbohydrate Diet (SCD) (18) gardening/nature (35) Hyperbaric Oxygen (10) Cerefolin (folate, B12 & NAC) (53) Azathioprine (2) Cannabidiol (CBD) (2) Valcyte (2) UVA-URSI (11) Yoga (263) Helminthic Therapy (7) UltraClear products (12) Acupuncture (278) Xyrem/GHB (13) ALA (50) Armour Thyroid (4) Coenzyme Q10 (332) Omega 3 (fish oil) (393) Ultram (tramadol) (98) D-Ribose (103) Bioidentical estrogen (19) Petrovic Protocol (5) Omega 3,6,9 (352) Iron (54) Afipran (1) Sauna (1) GcMAF (6) Taurine (11) Lamictal (11) Ubiquinol (46) Ionized Water (56) Naproxen (Aleve) (146) DHEA (62) Chinese herbs (123) NK stim supplements (7) Oxymatrine (7) Isagenix (7) EPA-DHA (59) Acetaminophen / Paracetamol (Tylenol, Panadol) (344) Kinesiology (45) Licorice Root Extract (40) Savella (3) Vicodin (hydrocodone) (3) Chiropractic (234) L-Carnitine (203) Valtrex (14) Bioidentical Hormones, i.e. progesterone (36) Homeopathy (194) vegan diet (9) Non-sedating antihistamines (137) Fentanyl patch (15) Urine Therapy (4) Ritalin (43) 5-HTP (83) Iodine (58) Distract your attention away from the symptoms (417) Mickel Therapy (6) Immunovir (isoprinosine, inosine pranobex) (24) Ganciclovir (7) Moclobemide (1) Catapres (clonidine) (14) Skin brushing (71) Melatonin (319) Formula 3030 (2) Cool shower following exertion (93) Detox Foot Baths with mild electric current (36) Wheat Germ Extract supplements (Avemar) (3) NADH (112) DMG (25) GABA (Gamma Amino Butyric Acid) (33) Pregabalin (5) Sophora root (5) Antibiotics (217) Vitamin C (lypo spheric) (71) Psychotherapy (non CBT) (175) Pall Protocol (13) Fresh Vegetable Juices (88) Cortef (hydrocortisone / synthetic cortisol) (83) Green Smoothies (green vegetables and fruit) (68) MSM (53) Brainwave audio CD's (69) Aspirin (169) Cortisol (compounded) (16) Propranolol (beta-blocker) (8) Sodium Valproate (9) Doxycycline (43) Beta-interferon (1) Heparin (1) MAF 314 (1) Piracetam (1) Metanx (1) Hydrotherapy (1) Raw food diet (27) Bowen Technique (10) Lansoprazole (11) Soak feet in cold water (44) Cats Claw - Uncaria Tomentosa (55) Reishi mushrooms (26) Lightning Process (16) Rolfing (27) Whey Protein supplements: (Immunopro/ Immunocal) (38) bicycle with power options (8) Vitamin E (96) AllicinPlus (active garlic capsules (64) Flaxseed oil (44) Hot baths (10) Antiretrovirals (10) ativan (11) Inosine (30) Tai Chi (104) Calcium (63) Vitamin A (67) Florinef (fludrocortisone) (17) Lyrica (26) Hot showers (12) Gingko Biloba (88) Marshall protocol (12) Provigil (modafinil) (124) SAM-E (104) Olive Leaf Extract (46) Cognitive Behavioral Therapy (CBT) (205) Orthostatic conditioning/exercise (65) Doxylamine (Unisom) (41) Undenatured whey protein (80) Monolaurin (e.g., Lauricidin) (37) Celexa, Cipramil (citalopram) (114) Diphendydramine (Unisom, Benadryl) (161) Atenolol (beta blocker) (36) Rebounder (32) Trazodone (92) Cymbalta (duloxetine) (138) Neurontin (gabapentin) (149) Wellbutrin (bupropion) (149) Caffeine (378) Mild/ moderate exercise (577) Amitriptyline (Elavil) (113) Regular exercise program (208) Effexor (venlafaxine) (136) SSRIs total(Prozac, Effexor, Celexa) (224) Zoloft (sertraline) (148) Prozac (fluoxetine) (164) Paroxetine (Paxil, Seroxat) (118) Alcohol (229) Graded Exercise Therapy (GET) From: 'DRUG DATABASE' http://fmcfsme.com/drug_database.php(for CFS/ME but includes FM) AAcaiacetaminophenAcetyl-L-CarnitineActiq®alprazolamAmbien®amitriptylineamoxapineAnafranil®Anexsia®Anolor®Asian GinsengaspirinAtivan®atomoxetine BbaclofenBalacet®Bancap®bupropionBuspar®buspironeButrans Patch® CCapsaicin®carbamazepinecarisoprodolCarnitineCelebrex®celecoxibCelexa®chlordiazepoxidecitalopramclonazepamcodeineCoQ10cyclobenzaprineCymbalta® DDarvocet®Darvon®Daypro®Demerol®desloratadinedesvenlafaxineDesyrel®DHEA®diazepamdiclofenacDicloflex®Dilaudid®Dolophine®doxepinD-Riboseduloxetine EEffexor®Elavil®Eldepryl®Endep®Endocet®Eskalith®estazolameszopicloneetodolac FfentanylFentora®Feverfew®fexofenadineFioricet®Fiorinal®Flebogamma®Flexeril®fluoxetineflurazepamfluvoxamine GgabapentinGammar-P I.V.®ganciclovirGarlicGinkoguaifenesin Hhalazepam5-HTPhydrocodonehydromorphone IibuprofenimipramineImitrex®Imovane®isocarboxazid J KKadian®KavaketamineketoprofenKlonopin® LLexapro®Licorice RootLidocaine®Lidoderm®Lioresal®Lodine®lorazepamLorcet®Lortab®L-TheanineLunesta®Lyrica® MMagnesium MalatemelatoninmephobarbitalmetaxalonemethadoneMethadose®MethocarbamolmilnacipranMirapex®mirtazapineMobic®moclobemidemorphine NnabiloneNADHNalfon®naltrexonenaproxenNardil®nefazodoneNembutal®Neurontin®nialamideNiravam®Norco®Norflex®Norpramin®nortriptylineNucynta®OomeprazoleOrudis®oxazepamoxycodoneOxyContin® PparacetamolparoxetinePaxil®Percocet®Percodan®Pexeva®phenelzinepiroxicamPlaquenil®pregabalinPropacet®propoxypheneProvigil®Prozac® RreboxetineReglan®Remeron®Requip®Restoril®Rhodiola RosearisperidoneRobaxin®rofecoxibRozerem® SSAM-eSarafem®Savella®Serax®sertralineSerzone®Sinemet®Skelaxin®sodium oxybateSoma®Sonata®St. John's Wortsumatriptan Ttiapreferic acidtizanidineToradol®tramadolTrancot®Tranxene SD®tranylcyprominetrazodonetriazolamTylox® UUltracet®Ultram® VvalganciclovirValium®Valtrex®Vanadom®Vanatrip®Vicodin®Vitamin B-12Vivactil®Voltaren® WWellbutrin®Wygesic® XXanax®Xyrem® ZzaleplonZanaflex®Zoloft®zolpidemzopicloneZostrix®Zyban®Zyrtec®Prescription Treatments click hereFrom: 'Treatments for ME/CFS' https://livingwithchronicfatiguesyndrome.wordpress.com/2016/10/15/treatments-for-mecfsPrescription Treatments for ME/CFSAzithromycin https://livingwithchronicfatiguesyndrome.wordpress.com/2012/05/09/may-2012-a-treatment-update/ Azithromycin is an antibiotic that has antiviral and immunomodulatory properties. It may be effective against a broad range of bacteria, many of which have been linked to ME/CFS. A study found that 58 out of 99 ME/CFS patients had a decrease in symptoms while taking Azithromycin. Dr. De Meirleir and Dr. Nicholson are both advocates of this antibiotic and have used it on ME/CFS patients with some success. Azithromycin is generally fairly low in side effects although sometimes causing stomach upset. It is normally taken 3 times a day away from food at a dosage of 500mg on each occasion. Dr. Brewer’s Protocol https://livingwithchronicfatiguesyndrome.wordpress.com/2015/09/15/dr-brewers-protocol/ This protocol involves patients taking either a nasal version of Amphotericin B or a compounded Nystatin that has to be atomised. Patients should also take a chelating PX. A pilot study by Dr. Brewer found that 56 out of 151 ME/CFS patients could not tolerate the Amphotericin B. 88 out of the remaining 94 patients 93.6% had a reduction in symptoms. Approximately a third of these 88 CFS patients reached remission. Since this pilot study, Dr. Brewer has used a compounded and atomised Nystatin due to it being safer than the nasal Amphotericin B. The theory behind Dr. Brewer’s Protocol involves treating the sinus reservoirs of mycotoxins that may be causing ME/CFS symptoms. Since replacing Amphotericin B with Nystatin, Dr. Brewer’s Protocol has become safer for patients, with followers of the protocol rarely reporting nasal side effects. Patients experiencing die-off symptoms range from 30-40% according to Dr. Brewer. The appropriate dosages of the compounded and atomised Nystatin and the chelating PX are provided by the compounding pharmacy. Clonazepam https://livingwithchronicfatiguesyndrome.wordpress.com/2012/09/13/september-2012-a-treatment-update/ This treatment is one of the most polarising ME/CFS treatments in existence. Clonazepam may benefit patients due to reducing the overstimulation of the brain and central nervous system. It also has potential effects as a sleep aid, neuroprotector and energy enhancer. Several ME/CFS specialists are advocates of Clonazepam under the right circumstances, such as Dr. Cheney. There are also many online reports of patients benefiting from Clonazepam. The dark-side of Clonazepam involves countless ME/CFS patients’ online anecdotes stating that this drug has been the worst treatment they have ever tried as it has caused long term side effects. A dosage around the 0.5mg- 1mg range is normally used on ME/CFS patients for sleep which is a lower amount than for other conditions. An even tinier dose is recommended by Dr. Cheney if the drug is used during the day with the motive of increasing the patient’s energy. Clonazepam shouldn’t be stopped suddenly and patients should gradually reduce the dose before ceasing treatment. The common side effects of Clonazepam include drowsiness and confusion. Some ME/CFS patients have reported other side effects such as a general worsening of their condition. As Clonazepam usage can be habit forming, patients often feel like they need to increase the dose to maintain efficacy which can be a dangerous process. Dexedrine https://livingwithchronicfatiguesyndrome.wordpress.com/2012/05/09/may-2012-a-treatment-update/ Dexedrine may benefit ME/CFS patients due to alleviating cognitive impairment, reducing fatigue and increasing energy. A small study found 9 out of 10 ME/CFS patients had reduced fatigue after taking Dexedrine in comparison to 4 out of 10 patients in the placebo group. Dr. Teitelbaum is a supporter of this treatment, believing that it increases energy and blood pressure. Dr. Goldstein has written that 1/3^rd of ME/CFS patients will improve as a result of taking stimulants and he has recommended amphetamine salts. One of the risks of Dexedrine is that prolonged usage may lead to addiction. Dr. Goldstein has warned that if specific neurotransmitters are low in an ME/CFS patient, stimulants may increase ME/CFS symptoms. Dr. Rowe has recommended that ME/CFS patients begin with a 5mg dosage in the morning and if no improvement is noted, the dosage be increased to 10-15mg. Some patients may find that 5mg is too high for them to tolerate. DHEA https://livingwithchronicfatiguesyndrome.wordpress.com/2009/08/25/prescription-medications-that-i-have-taken-for-cfs/ DHEA is a hormone produced by the adrenal glands. A study found that the majority of the Japanese ME/CFS subjects had DHEA deficiency. Several studies have found the use of oral DHEA and intravenous vitamin C to be useful in treating ME/CFS. Another study found normal DHEA levels in ME/CFS patients but low blood levels of a hormone that causes the adrenal glands to release DHEA. Dr. Cheney has found that DHEA is more effective in less severe cases of ME/CFS and that sometime symptoms may worsen if severely ill patients take this treatment. Dr. Myhill recommends Pregnenolone as an alternative to DHEA. Some doctors have experienced success in prescribing lower doses of DHEA such as doses less than 10mg. Another ME/CFS specialist recommends 50mg every second day. Palpitations, hair loss, acne and an upset stomach are some possible side effects. Fludrocortisone https://livingwithchronicfatiguesyndrome.wordpress.com/2010/07/27/fludrocortisone-for-cfs/ Fludrocortisone is a synthetically produced hormone. It may benefit ME/CFS patients with; hypotension, POTS, orthostatic intolerance or adrenal insufficiency. Its mechanism of action in ME/CFS patients could be due to; increasing blood volume, raising blood pressure and helping blood reach the bodies extremities. Three studies have been performed on ME/CFS patients taking Fludrocortisone with the ME/CFS patients’ level of improvement no better than the placebo group. According to Dr. Bell, Fludrocortisone is more likely to work on younger patients who are still somewhat active. Dr. Bell tries this treatment on almost all of his patients and says that it works well in approximately 25% of cases. If the drug doesn’t increase the ME/CFS patients’ activity levels by at least 50%, he stops the drug. Dr. Cheney believes that liquorice can have the same effect on patients as Fludrocortisone. Many ME/CFS specialist recommend that Fludrocortisone dosages start at a very low amount such as a quarter of a 0.1mg tablet. Dr Rowe begins patients on a quarter of a tablet and if no side effects are noted, gradually increased this amount every 4-7 days to maximum of 2 tablets 0.2mg. Potassium and plenty of water should be used concurrently with this treatment. High blood pressure and depression are two possible side effects. Gabapentin Neurontin https://livingwithchronicfatiguesyndrome.wordpress.com/2016/04/13/gabapentin-neurontin-for-me/ Gabapentin is a anticonvulsant drug that may benefit ME/CFS patients due to reducing pain, increasing energy and improving sleep. Its mechanism of action may be its ability as a calcium channel blocker to reduce the excretion of certain neurotransmitters that cause pain and stimulate the brain. Anecdotally, a number of ME/CFS patients have gained extra energy as a result of taking Gabapentin however in some of these cases the extra energy has worn off. Dr. Goldstein lists Gabapentin amongst his five most favoured treatments for ME/CFS. Dr. Teitelbaum uses Gabapentin for its sleep effects and Dr. Enlander uses it for stopping the ‘abnormal impulses’ in ME/CFS patients’ brains. Three studies have found Gabapentin to be beneficial to Fibromyalgia patients in the areas of sleep enhancement and pain reduction. Gabapentin is considered to be fairly safe with a Cochrane review finding that serious adverse effects were no more common in the Gabapentin group than the placebo group. Dizziness, somnolence, peripheral oedema and gait disturbance are the most common side effects. Dosages should begin at low levels and only be increased if tolerated. ME/CFS specialists tend to start patients at 100mg-800mg and if no side effects occur, the dose is gradually increased up to 2400mg-5000mg. These doses are the total daily dosages and should be split up into three dosages across the day. Heparin https://livingwithchronicfatiguesyndrome.wordpress.com/2016/08/23/heparin-for-me/ Heparin is an anti-coagulant drug that may benefit ME/CFS patients who have hypercoagulation. A Heparin-ME/CFS study found all 9 patients gaining improvement with 5 noting significant improvement. Another paper refers to 60 ME/CFS/Fibromyalgia patients taking Heparin with an average improvement of 85%. Dr. Teitelbaum writes that Heparin helps about 50% of ME/CFS patients who haven’t benefited from any other treatment. It is imperative that ME/CFS patients have coagulation testing performed to determine Heparin suitability before commencing treatment. Depending on what type of Heparin is used and what delivery method is chosen, the possible side effects of Heparin vary. If unfractionated Heparin is injected subcutaneously, regular blood tests to monitor treatment are a necessity. Heparin-induced thrombocytopenia is a potential side effect with this treatment although with Low Molecular Weight Heparin this is less likely to occur. A DEXA bone density test and liver and kidney function tests may be required before starting Heparin treatment. Sublingual Heparin and Low Molecular Weight Heparin are considered safer than unfractionated Heparin. Dr. Teitelbaum recommends those patients taking unfractionated Heparin start with 5000 unit injections twice a day and if blood tests are normal, the dose be gradually increased to a maximum of 8000 units twice a day. Isoprinosine Immunovir https://livingwithchronicfatiguesyndrome.wordpress.com/2012/11/19/november-2012-a-treatment-update-clonazepam-and-imunovir/ Isoprinosine may benefit ME/CFS patients due to its effects as an antiviral as well as its various immunomodulatory properties. A study found that 6 out of 10 ME/CFS patients benefited by taking Isoprinosine. In those patients who improved, their CD4+, T-cells and natural killer cells dramatically increased. Dr. Sharp believes Isoprinosine is one of the most helpful, safest and cost effective drugs for ME/CFS patients. Isoprinosone may increase uric acid levels and therefore shouldn’t be used by those with gout. ME/CFS specialists generally pulse the dosage of Isoprinosine so patients don’t develop a tolerance to the drug. Low Dose Naltrexone LDN https://livingwithchronicfatiguesyndrome.wordpress.com/2010/02/26/low-dose-naltrexone-for-cfs/ When used at low doses, Naltrexone causes the body to create more opioids which in turn may; relax the microglial cells, block pain, create endorphins and modulate the immune system. A small, pilot study on Fibromyalgia patients found that subjects experienced on average a 30% decrease in pain and fatigue while taking LDN. A second placebo controlled study on Fibromyalgia patients resulted in 32% of those taking LDN experiencing a significant reduction in pain as well as either a significant reduction in sleep problems or significant reduction in fatigue. Dr. Bihari reports that approximately 50% of ME/CFS patients are helped by LDN. Stories litter the internet of ME/CFS patients benefiting from this treatment. LDN is considered one of the safest treatments for ME/CFS with few patients experiencing side effects. The most common side effect is sleep disturbance. The dosage used is normally in the 1.5mg-4.5mg range. LDN is generally taken at night before falling asleep. Magnesium Injections https://livingwithchronicfatiguesyndrome.wordpress.com/2011/03/09/my-2011-treatments-a-progress-report/ A study found low red blood cell magnesium levels in ME/CFS patients. After intramuscular magnesium sulphate injections, 12 out of the 15 ME/CFS patients improved compared to 3 out 17 patients receiving the placebo improving. A study determined that despite normal magnesium blood levels, Fibromyalgia patients had low intracellular levels of magnesium. Dr. Myhill has found approximately 70% of her ME/CFS patients improving after receiving magnesium injections. Magnesium injections can cause temporary pain at the injection sight. High doses may cause diarrhea. Intramuscular injections are generally given once or twice a week. Melatonin https://livingwithchronicfatiguesyndrome.wordpress.com/2011/03/09/my-2011-treatments-a-progress-report/ Melatonin is a hormone whose primary role as an ME/CFS treatment is to aid sleep. One study found that it improved ME/CFS patients’ ability to function and that it enhanced patients’ quality of life. Another study concluded that it reduced patients’ fatigue levels. Dr. Wright states that over 60% of his ME/CFS patients produce undetectable levels of Melatonin. As well as improving quality of sleep, this treatment may be beneficial due to its anti-inflammatory and antioxidant effects. The most common side effects of Melatonin are morning drowsiness and headaches. These side effects may dissipate if the dose is decreased. Melatonin is listed in this section under the ‘prescription treatments’ umbrella due to a prescription being required to gain it in Australia despite formulations with negligible amounts of Melatonin being available over the counter. Other countries may have differing laws regarding prescription requirements to gain Melatonin. Some doctors use doses as low as 0.5mg while most doctors recommend doses in the 3-9mg range. It is normally taken at night, before sleep. Myers’ Cocktail https://livingwithchronicfatiguesyndrome.wordpress.com/2011/03/09/my-2011-treatments-a-progress-report/ The Myers’ Cocktail is an intravenously administered mixture of supplements including; magnesium, calcium, vitamin C, B vitamins and sometimes further ingredients. A study on Fibromyalgia patients receiving this treatment found that most of the subjects noted improvements however the placebo group that received a saline solution also improved. Intravenous saline solution is considered by some to be an effective treatment for ME/CFS/Fibromyalgia hence it is conceivable that both groups did improve. The authors noted that both groups experienced “strong symptomatic relief.” Dr. Teitelbaum is an advocate of Myers’ Cocktails and believes they can provide ME/CFS patients with more energy. Dr. Majid Ali had found that 15 grams of intravenous vitamin C an ingredient in Myers’ cocktails can fix the abnormal shapes of ME/CFS patients’ blood cells and hence improve blood flow. Some patients feel sleepy immediately after a Myers’ cocktail for a short period of time. If the patient feels excessive warmth, dizziness, nausea or a headache during the Myers’ cocktail IV, they should notify the physician. The dosages of the individual ingredients within a Myers’ cocktail vary and are at the physician’s discretion. Nexavir Kutapressin https://livingwithchronicfatiguesyndrome.wordpress.com/2010/10/25/nexavir-kutapressin-for-cfs/ Nexavir is a porcine liver extract that is administered via subcutaneous or intramuscular injection. Studies have found that Nexavir can inhibit EBV in vitro and HHV-6 replication in vitro by greater than 90%. A study of 270 ME/CFS subjects found that a staggering 96% of patients receiving more than 40 Kutapressin injections reached remission or near remission status. 71% of patients receiving 11-40 injections obtained remission or near remission levels. If an ME/CFS patient had high EBV-EA-IgG titres, they were more likely to improve in this study. A final Kutapressin study contained 130 ME/CFS patients with 85% noting significant improvements. 43% of patients reached remission while a further 42% of patients gained near remission status they had a few residual symptoms. Dr. De Meirleir had found 67% of his ME/CFS patients responding to Nexavir in comparison to 17% receiving the placebo improving. Dr. Cheney, Dr. Enlander, Dr. Teitelbaum and Dr. Lapp have all been advocates of Nexavir or an analogous version of Nexavir. Out of the 400 patients across both Kutapressin- ME/CFS studies, only 1 person experienced new symptoms and a deterioration of function following Kutapressin injections. Some physicians are reluctant to prescribe antivirals including Valtrex or Famvir due to side effects and therefore prescribe Nexavir as a safer alternative. Nexavir is contraindicated in those allergic to pork or liver products. It shouldn’t be used by those taking MAO inhibitors. The most common dosage is 2mls administered daily although some patients start with a lower dose. Nimodipine https://livingwithchronicfatiguesyndrome.wordpress.com/2012/11/26/nimodipine-for-me/ Nimodipine is a calcium channel blocker that is used to improve cognitive function or reduce pain in other illnesses. Dr. Goldstein found that Nimodipine improved ME/CFS patients’ cerebral blood flow monitored through SPECT scans and indeed this is the treatment’s primary usage in ME/CFS patients. Dr. Goldstein has labelled Nimodipine as one of the most useful treatments for both ME/CFS and Fibromyalgia. Dr. Mason Brown has found that Nimodipine helps 20% of ME/CFS patient quickly, another 20% over 6 months and the remaining patients to varying degrees. A report on Nimodipine usage in ME/CFS patients found that 9 out of 13 experienced enhanced mental clarity or improved general functioning. Possible side effects of Nimodipine include; hypotension, nausea, headache, bradycardia, skin rash and peripheral edema. Specialists generally recommend starting at a low dose some patients begin with as little as 1/16^th of a tablet. The maximum dose normally recommended for ME/CFS patients is 30-60mg taken 2-3 times a day. Oxytocin https://livingwithchronicfatiguesyndrome.wordpress.com/2010/07/05/oxytocin-for-cfs/ This treatment is a neurotransmitter hormone whose most effective delivery method is widely considered to be injection, followed by nasal spray and finally tablets. The ME/CFS patients most likely to respond to Oxytocin are those with cold extremities. Dr. Flechas states that many ME/CFS symptoms are similar to those that an Oxytocin deficiency would cause. Dr. Goldstein found approximately 20% of his patients benefiting from Oxytocin injections and in those patients who do benefit, the improvement is dramatic. As well as Dr. Goldstein, the ME/CFS specialists; Dr. Lapp, Dr. Flechas and Dr. Teitelbaum all use Oxytocin injections on their ME/CFS patients. Possible side effects of Oxytocin include; headache, weight gain, irregular heartbeat, nausea and dizziness. Intramuscular injections are sometimes given at 10 units and sublingual Oxytocin has been used by Dr. Cheney at 10 units up to a maximum of three times a day. Oxytocin should not be used by those who are pregnant. Pentoxifylline https://livingwithchronicfatiguesyndrome.wordpress.com/2011/09/05/pentoxifylline-for-me/ Pentoxifylline belongs to a class of drugs called xanthine derivatives and its most common usage is to improve cerebral and peripheral blood circulation. It may also benefit ME/CFS patients by reducing; the cytokine IL-2, lowering NF-Kappa B and downregulating the cytokine TNF-alpha. All three facets of the immune system are thought to be high in ME/CFS patients and potentially contributing to symptoms. Pentoxifylline also has antiviral and further immunomodulatory properties. Dr. Leslie Simpson has noted that Pentoxifylline is useful at reducing cognitive problems and dizziness in ME/CFS patients. Pentoxifylline should not be taken by those who cannot tolerate stimulants. It should also be avoided by those with a peptic ulcer or at risk of haemorrhaging. The drug hasn’t been well studied in ME/CFS patients but in other illnesses is considered safe and well tolerated at 1200mg per day. The standard dose of Pentoxifylline for various non ME/CFS illnesses is 400mg three times per day. Rifaximin Xifaxan https://livingwithchronicfatiguesyndrome.wordpress.com/2014/11/11/rifaximin-for-m-e/ Rifaximin is an antibiotic that may benefit ME/CFS patients due to eradicating small intestinal bacterial overgrowth SIBO. SIBO involves healthy bacteria in the large intestine being transferred to the small intestine thus causing gastrointestinal symptoms. Dr. Pimentel found 100% 42/42 of Fibromyalgia patients testing positive to SIBO compared to 20% of controls. The degree of pain experienced by Fibromyalgia patients in this study correlated strongly with the amount of hydrogen seen on the lactulose breath test. Rifaximin may also help ME/CFS patients as it balances gut flora. In vitro, 90% of the 536 strains of anaerobic bacteria tested were inhibited in vitro. Anecdotally, a reasonable number of ME/CFS patients have improved whilst on Rifaximin although many patients have had their symptoms return upon stopping the drug. Interestingly, some ME/CFS patients with no gastrointestinal symptoms improve. Dr. De Meirleir, Dr. Teitelbaum, Dr. Peterson and Dr. Myhill all use Rifaximin on their ME/CFS patients with some only using it after positive test results. Rifaximin is generally well tolerated and only 0.4% of subjects in a traveller’s diarrhea study had to discontinue treatment due to side effects. The most common side effects are gastrointestinal. Long term usage of Rifaximin increases the chances of building resistance to the drug. Some specialists recommend a slightly lower dose of 550mg taken 2 times per day for 8 days. Other specialists recommend doses up to 550mg be taken 3 times per day for 14 days. It is recommended that probiotics are taken after Rifaximin usage. Sleep Aids https://livingwithchronicfatiguesyndrome.wordpress.com/2015/09/20/the-best-sleep-aids-for-m-e/ In the attached link I examine the various prescription sleep drugs that the ME/CFS specialists recommend. Dr. Cheney, Dr. Teitelbaum, Dr. Klimas, Dr. Lapp, Dr. Myhill and Dr. Enlander all have certain sleep inducing and sleep enhancing drugs that they try on their patients in a specific order. Vitamin B12 Injections https://livingwithchronicfatiguesyndrome.wordpress.com/2011/01/08/10-of-the-most-effective-treatments-for-cfs/ Despite often having normal B12 as determined by a blood test, ME/CFS patients commonly have low B12 levels in their brain. High levels of B12 being injected can ensure that sufficient B12 crosses the blood-brain barrier. B12 may also benefit ME patients by acting as a scavenger of nitric oxide, a compound that may contribute to ME/CFS symptoms. A poll found that 50%-80% of Dr. Lapp and Dr. Cheney’s ME/CFS patients improved to some degree after taking B12 injections. A study found that ME/CFS patients were much more likely to respond to B12 injections if they had more frequent injections, a higher dose of B12, tried the treatment for longer and were taking oral folic acid. The study also found that the concentrated 5mg/ml methylcobalamin form of B12 tended to be more effective than the hydroxocobalamin form 1mg/ml. Some specialists prefer the cyanocobalamin form of B12 as it is more stable. If an ME/CFS patient doesn’t respond to B12 injections, they may respond to oral folic or folinic acid. B12 is also available over-the-counter in a sublingual form however this isn’t necessarily as effective as the injectable versions. ME/CFS specialists inevitably opt for injectable B12 over other forms. Dr. De Meirleir, Dr. Lapp, Dr. Teitelbaum and Dr. Cheney are amongst a number of ME/CFS specialists to use this treatment. When taking high doses of B12, a vitamin B complex is recommended to be taken concurrently. Although considered to be a fairly safe treatment, B12 may cause a temporary weakness in some patients. Dosage, type of B12, frequency of injection and method of injection vary depending on the physician’s preference. Over-the-Counter Treatments for ME/CFS Non PrescriptionArtesunate https://livingwithchronicfatiguesyndrome.wordpress.com/2009/08/25/antiviral-and-immunomodulator-cfs-treatment-i-am-trying/ Artesunate is a derivation of the herb artemisia and commonly used in the non-ME/CFS realm for its anti-malarial properties. It may benefit ME/CFS patients due to its potential anti-herpesvirus and anti-CMV effects. Using Artesunate, Dr. Cheney has doubled his number of ME/CFS cures and 75% of patients have shown some level of improvement using this treatment. Part of Dr. Cheney’s protocol involves the Artesunate being used concurrently with the herb wormwood. Some ME/CFS patients taking Artesunate have reported dizziness or tiredness. Dr. Cheney recommends the brand Hepasunate be taken on three days of the week. As opposed to swallowing the capsule, he encourages patients to place half the contents of the capsule under their tongue for a period of a minute followed by swishing it around their mouth and spitting the remnants out. Benfotiamine and Allithiamine https://livingwithchronicfatiguesyndrome.wordpress.com/2016/01/11/astaxanthin-b1-variants-elimination-diet-ip-6-naphazoline-and-ranitidine/ These are alternate versions of high dose thiamine that may be better absorbed. Anecdotally, many patients have improved as a result of these treatments. Studies have shown that a thiamine deficiency can causes similar symptoms to ME/CFS and these symptoms can be resolved especially fatigue after treatment with high doses of thiamine. See ‘Thiamine- High Dose’ for more information about thiamine and ME/CFS. Theoretically, these treatments should be avoided by those who have cancer. Few side effects have been reported by those taking Benfotiamine and Allithiamine. It is difficult to determine a standard quantity for these ‘high dose’ treatments as patients have tried a wide range of doses. Anecdotally, ME/CFS patients online have commonly taken either 50-200mg of Allithiamine or 300-600mg of Benfotiamine. Biotin https://livingwithchronicfatiguesyndrome.wordpress.com/2014/01/29/my-me-treatments-a-january-2014-update/ Biotin deficiency has many shared features with ME/CFS. Several anecdotal accounts are online that mention Biotin greatly benefiting ME/CFS patients. High dose Biotin is currently being studied, with some promising results, as a treatment in progressive multiple sclerosis. Biotin is normally a fairly safe treatment with few side effects noted. The dosages used by ME/CFS patients have often been in the 300mcg-1000mcg range. A neurologist from Massachusetts recommended that an ME/CFS patient take; 100mg of B1 twice a day, 100mg of B2 and the high dosage of 5000mcg of Biotin for treating post-exertional malaise. This treatment benefited the patient. Butyrate https://livingwithchronicfatiguesyndrome.wordpress.com/2014/08/05/my-me-treatments-an-august-2014-update/ Butyrate may improve ME/CFS patients’ gut symptoms by creating T-cells in the digestive system. It may reduce cognitive symptoms, lower inflammation and enhance the immune system. Studies have shown that butyrate may be beneficial in treating ulcerative colitis and Crohn’s disease symptoms. Butyrate is low in side effects and 1-2 capsules are usually taken with each meal. Coenzyme Q10 Coenzyme Q10 is a treatment that when taken with L-Carnitine, has superior effects. These treatments both enhance mitochondrial function and hence may benefit ME/CFS patients. The active version of Coenzyme Q10, Ubiquinol is often preferred. A study found a close association between levels of Coenzyme Q10 and severity of ME/CFS. Dr. Lapp has found that about half of his patients benefit from Coenzyme Q10 generally by around 10%-15%. A University of Iowa study rated Coenzyme Q10 as the leading treatment for ME/CFS with 69% of patients reporting it as beneficial. A study with 20 ME/CFS patients 80% of those deficient in Coenzyme Q10 found 90% had a reduction or complete disappearance of symptoms after 3 months of taking Coenzyme Q10. There is a theory that taking Coenzyme Q10 as two doses throughout the day can increase its efficacy. There also exists a sublingual version of Coenzyme Q10. Alongside the energy boost that Coenzyme Q10 may provide, it occasionally causes insomnia. Those with diabetes or other types of hypoglycemia should be wary of Coenzyme Q10 as it can reduce blood sugar levels. The daily dose that is used generally varies from 50mg to 300mg. Cordyceps Sinensis and Shiitake Mushroom https://livingwithchronicfatiguesyndrome.wordpress.com/2011/03/09/my-2011-treatments-a-progress-report/ Cordyceps Sinensis may enhance the immune system. A study on healthy subjects found ‘CordyMax’ increased aerobic capacity, reduced fatigue and lowered diastolic blood pressure. Another treatment that is similar to Cordyseps Sinensis is Shiitake mushroom which may increase interferon levels and have antiviral and immunomodulatory benefits. Anecdotally, numerous ME/CFS patients have reported more energy after taking versions of Shiitake mushroom supplements. A Japanese study that used injected ‘Lentinan’ taken from Shiitake mushroom on ME/CFS subjects found patients’ natural killer cell function increased. Recovery of the majority of patients studied took several months. Another study injected Lentinan into ME/CFS patients and found that 6 months of injections was required to normalise natural killer cell activity. Lentinan doesn’t get absorbed orally hence has to be given as an injection. Maitake and Reishi are another two of the many types of mushroom supplements used by ME/CFS patients. A study found that oral Maitake and oral Shiitake mushroom in combination significantly increased natural killer cell function in mice. Most people that take Cordyceps Sinensis experience no side effects however rarely diarrhea and nausea can occur transiently. In the aforementioned study, subjects took 333mg of Cordymax three times per day with meals. Shiitake mushroom supplements may cause gastrointestinal symptoms or a rash. Shiitake mushroom supplements are sometimes used at daily doses between 400mg-1500mg, with this total daily dose broken up into smaller doses taken several times a day. Curcumin https://livingwithchronicfatiguesyndrome.wordpress.com/2015/02/01/sulforaphane-nicotine-gum-curcumin-and-vns/ Curcumin is a derivation of turmeric. A study found that curcumin benefited mice with ‘CFS.’ Dr De Meirleir has recommended this treatment to some patients. It may reduce cognitive impairment, improve HPA axis dysfunction and have anti-inflammatory and antioxidant properties. A study found that when Curcumin is supplemented with either; olive oil, stearic acid or choline, the brain and blood absorption levels of Curcumin dramatically increase. Side effects from Curcumin usage are rare however if they do occur are generally of a gastrointestinal nature. Dosages used generally fall within the 500mg-1000mg range. Those with illnesses other than ME/CFS have ventured up to 8 grams of Curcumin a day. The absorption levels of the specific type of Curcumin used are relevant when determining a dosage. D-Ribose https://livingwithchronicfatiguesyndrome.wordpress.com/2011/01/08/10-of-the-most-effective-treatments-for-cfs/ This treatment may improve mitochondrial function and supply the body with energy. A pilot study found that 66% of ME/CFS patients significantly improved while taking D-Ribose. A follow up study involved 203 ME/CFS and Fibromyalgia patients that completed three weeks of treatment. The patients’ experienced: an average energy increase of 61%, a 37% improvement in well-being, a 30% increase in mental clarity, a 29% enhancement in sleep and a 16% reduction in pain. D-Ribose shouldn’t be used by those with gout as it may raise uric acid levels. Side effects can include nausea, headache and sleepiness. In the above D-Ribose studies, patients took 5 grams of D-Ribose, three times per day. It may be wise to start at a lower dose, to gauge any potential side effects. Energy Revitalization System https://livingwithchronicfatiguesyndrome.wordpress.com/2011/01/08/10-of-the-most-effective-treatments-for-cfs/ This formulation contains a broad range of nutrients including a B vitamin complex. It also contains various amino acids, choline, malic acid and biotin. It was developed by Dr. Teitelbaum and it is claimed that it can replace taking 30 tablets in the one formulation. A number of the ingredients probably aren’t of a high enough dosage to have a therapeutic effect on some patients although other parts of this formulation contain reasonable dosages. Many ME/CFS specialists recommend that patients take a multi-vitamin tablet including Dr. Cheney who labels a quality multi-vitamin as “essential.” Energy Revitalization System isn’t a multi-vitamin tablet but rather a powder containing eclectic ingredients targeted at improving patients’ energy. A small number of patients taking this treatment experience gastrointestinal symptoms. The typical dosage is one scoop 20.3 grams per day. Epicor https://livingwithchronicfatiguesyndrome.wordpress.com/2010/02/03/beta-glucan-and-coconut-oil/ Studies have shown that Epicor may improve natural killer cell function which is almost inevitably low in ME/CFS patients up to 4-fold. A similar substance, beta-glucan, may regulate other parts of the immune system too. A study that induced mice with ‘CFS’ found that beta-glucan significantly improved the symptoms of the mice. Epicor and beta-glucan are considered to be fairly safe supplements. The standard dosing of Epicor and beta-glucan ranges from 200mg to 3000mg. Essential fatty acids EFA Essential fatty acids include such substances as; flaxseed oil, evening primrose oil and fish oil. The first study to examine EFA usage in ME/CFS patients provided patients with both omega-3 and omega-6, resulting in 85% of the patients showing at least moderate improvement. A second study on ME/CFS patients taking EFA found 90% of patients experiencing a reduction in symptoms. Another study that provided patients with eicosapentaenoic acid EPA found that all four patients improved while the same patients didn’t respond to a placebo. Heartburn and gastrointestinal symptoms are some of the most common side effects of fish oil. The recommended dosing of EFA varies depending on what type of EFA product is being used. Fish oil is often used at 3000-4000 mg per day. Far Infrared Sauna https://livingwithchronicfatiguesyndrome.wordpress.com/2014/08/05/my-me-treatments-an-august-2014-update/ A study on 13 ME/CFS patients using a Far Infrared Sauna found two patients dramatically improve. The other 11 ME/CFS patients had a reduction in physical symptoms, lower levels of pain and reduced fatigue. Another study monitored the effects of Far Infrared Saunas on 10 ME/CFS patients. Average fatigue levels reduced on a 10 point scale from 6.7 to 4.8. It is recommended to hydrate after a Far Infrared Sauna session with electrolytes. Also, many people shower when a session is completed to remove the excess sweat from their body. The Far Infrared Sauna user should also be cognisant of the signs of heat stroke. ME/CFS patients that do trial this therapy should start off for only a short period of time in the Far Infrared Sauna before gradually increasing the time period if they don’t experience side effects. Some patients slowly build up to having a maximum 15-30 minute session per day. Fucoidan https://livingwithchronicfatiguesyndrome.wordpress.com/2010/09/14/fucoidan-for-cfs/ There is limited information online pertaining to ME/CFS patients taking Fucoidan. Despite this, over 850 studies on Pubmed detail many effects that may potentially benefit ME/CFS patients. These include; immune modulation, antiviral, anticoagulant and anti-inflammatory effects. A study found that Fucoidan reduced the amount of fatigue experienced by cancer patients. Fucoidan is widely considered to be a safe treatment. Some people have experienced transient diarrhea while taking this treatment. Anticoagulants shouldn’t be used while a patient in on Fucoidan. Studies have found that the efficacy of Fucoidan is largely dose dependant. An osteoarthritis study determined that 1000mg per day had a much better effect on subjects that 100mg per day. Fucoidan has been largely untried by the ME/CFS patient community hence appropriate doses are hard to establish. Germanium https://livingwithchronicfatiguesyndrome.wordpress.com/2011/10/10/my-2011-me-treatments-a-progress-report/ A 1988 paper reported that Dr. Greenberg found 25% of his ME/CFS patients showing “substantial clinical improvement” as a result of taking 300mg of Germanium a day. Dr. Maslin in the same paper found 150mg-300mg daily was sufficient to provide significant relief from ME/CFS symptoms in the majority of his patients and found 20% of patients to be non-responders. Dr. Anderson found half of his patients responding favourably to Germanium with doses for some patients needing to be as high as 1 gram. If patients are keen to take high doses of Germanium, they should have regular tests to monitor kidney function. It may be wise for ME/CFS patients to start Germanium at a low dosage and gradually build up to 300mg per day. As the above specialists’ reports indicate, some patients may need high doses, up to 1 gram a day to experience the effects of this treatment. The safer, medicinal form of Germanium is known as organic Germanium-132, the inorganic form is not recommended for supplemental use. Hawthorn https://livingwithchronicfatiguesyndrome.wordpress.com/2011/03/09/my-2011-treatments-a-progress-report/ Dr. Cheney has been an advocate of Hawthorn and did recommend its use in tandem with the prescription injectable, Nexavir. Hawthorn may improve the heart’s ability to pump blood around the body. Dr. Cheney trialled it on some of his patient and noted that it improved their cardiac output. In low doses, Hawthorn is non-toxic. Side effects are fairly uncommon but may include; nausea, headaches and palpitations. Doses used generally fall between 200mg-1000mg. Inosine https://livingwithchronicfatiguesyndrome.wordpress.com/2011/01/08/10-of-the-most-effective-treatments-for-cfs/ The supplement, Inosine, is the active ingredient in prescription medication ‘Isoprinosine.’ A study on the prescription version of this treatment found benefits in 6 out of 10 ME/CFS patients. Dr. De Meirleir believes the supplement Inosine is as effective as the prescription formulation. Inosine is antiviral and an immunomodulator. Dr. Sharp has labelled its prescription cousin as “One of the safest, most cost effective and helpful drugs at our ME/CFS doctors’ disposal.” Inosine is fairly low in side effects although some patients have experienced insomnia and headaches. Inosine can raise uric acid levels so shouldn’t be taken by those with gout. ME/CFS patients commonly take inosine at a dosage of 500mg three times a day but only on five days of the week. The treatment isn’t taken on 2 consecutive days each week such as the weekend. A pulsing dosing structure of this treatment is recommended so the patient doesn’t build up a tolerance to the Inosine. IP-6 Inositol Hexaphosphate https://livingwithchronicfatiguesyndrome.wordpress.com/2016/01/11/astaxanthin-b1-variants-elimination-diet-ip-6-naphazoline-and-ranitidine/ The main mechanism of this supplement is to increase natural killer cell activity which is inevitably low in ME/CFS patients. Dr. Conley reports that he has used IP-6 to increase natural killer cell function in dozens of cases of ME/CFS. He notes one patient who went from being unable to work to working a 32-40 hour a week job as a result of taking IP-6. A related treatment that some patients use is Inositol. Inositol may be useful against insomnia and depression. IP-6 is generally low in side effects with the most common being gastrointestinal. It is recommended that this supplement be taken on an empty stomach and twice a day. Some ME/CFS patients start with a lower dose of IP-6 such as 500mg and gradually increase this dosage to a total daily dose between 2-8 grams. The dose is taken at two separate occasions each day. L-Carnitine This amino acid could potentially benefit ME/CFS patients due to improving mitochondrial function. Acetyl-L-Carnitine may be better absorbed by the body than standard L-Carnitine. When taken in tandem with Coenzyme Q10, the positive effects may be magnified. A research centre found that out of 150 ME/CFS patients taking L-Carnitine, 69% noted an improvement in symptoms. A study found 12 out of 18 ME/CFS patients noting a statistically significant reduction in fatigue as a result of taking L-Carnitine. Another study found that 59% of ME/CFS patients taking Acetyl-L-Carnitine improved, 63% taking Propionyl-L-Carnitine improved but only 37% taking both treatments improved. The study noted that Acetyl-L-Carnitine mainly reduced mental fatigue while Propionyl-L-Carnitine was more likely to lower general fatigue. Studies have found ME/CFS patients low in cellular acylcarnitine levels. Deficiency of acylcarnitine can produce symptoms similar to ME/CFS. A study also found that as acylcarnitine levels improved in ME/CFS patients, symptoms improved. L-Carnitine should be avoided by those ME/CFS patients with low thyroid. If side effects do occur, they may be of a gastrointestinal nature. L-Carnitine should be taken with food and recommended dosages range from 1000mg to 2000mg per day. Patients often start off with a lower dose before increasing the dosage if no side effects occur. L-Serine https://livingwithchronicfatiguesyndrome.wordpress.com/2011/05/31/mecfs-treatments-a-progress-report/ L-Serine is an amino acid that former ME/CFS specialist Dr. Buttfield believes should help 60% of CFS patients significantly. Dr. Vallings found that 5/6 ME/CFS patients benefited from L-Serine supplementation. A study found that ME/CFS patients had “significantly reduced” levels of L-Serine in their urine when compared to healthy controls. The study continued on to note that those ME/CFS patients with low urinary L-Serine levels had mainly neurological symptoms and high levels of pain. L-Serine side effects are fairly rare but may consist of sleep disturbance or gastrointestinal symptoms. Dr. Buttfield’s protocol consisted of beginning patients on 500mg of L-Serine in the morning and increasing this dosage to 2 grams per day. Magnesium The majority of ME/CFS specialists incorporate either oral magnesium or magnesium injections into their treatment protocol. Dr. Cheney believes magnesium can benefit ME/CFS patients due to; enhancing energy, improving sleep and lowering muscle pain. He advocates oral magnesium glycinate due to its ability to cross the blood-brain barrier and also be absorbed into cells. Other ME/CFS specialists prefer magnesium citrate due to its possible higher levels of bodily absorption. Another facet of Dr. Cheney’s advocacy of magnesium glycinate is that this treatment is less likely to cause gastrointestinal symptoms. Other forms of magnesium are more likely to cause diarrhea. Magnesium should be taken with food and dosages should begin at low levels before increasing to the 200mg-400mg range. NADH This treatment is a form of coenzyme 1. A study found that 31% of ME/CFS patients improved while taking NADH in comparison to 8% of the control group improving. 18 out of 25 72% of ME/CFS patients enrolled in the longer follow up version of this study noted improvements. There is some evidence that it may take up to 6 months before certain ME/CFS patients respond to this treatment. Side effects tend to be rare but mild overstimulation is possible. NADH should be taken on an empty stomach, before breakfast. Recommended dosages range from 5mg up to 20mg per day. Naphazoline HCL https://livingwithchronicfatiguesyndrome.wordpress.com/2016/01/11/astaxanthin-b1-variants-elimination-diet-ip-6-naphazoline-and-ranitidine/ Dr. Goldstein, who was an ME/CFS specialist, always tried Naphazoline HCL 0.1% eye drops as an initial treatment when a patient stepped into his office. He claimed that 20% of patients benefited from this treatment and in those patient who benefited, the benefits were remarkable and immediate. He theorised that those patients in the cohort of having severe anxiety were the most likely to respond. In some countries such as Australia, Naphazoline HCL is available over-the-counter. The delivery process of this treatment involves placing a drop in each eye. Due to the nature of Naphazoline HCL, any benefits will be felt almost instantaneously. One of the most common side effects is local irritation. The occurrence of more serious side effects from this treatment is unlikely but may include; dizziness, headache or nausea. The dosage of the Naphazoline HCL eye drops used should be 0.1% and not 0.01%. NeuroProtek https://livingwithchronicfatiguesyndrome.wordpress.com/2011/10/10/my-2011-me-treatments-a-progress-report/ NeuroProtek contains a number of eclectic supplements; luteolin, quercetin and rutin in tandem with the antioxidant, olive kernel oil. Anecdotally, many ME/CFS patients have reported a reduction in cognitive impairment as a result of taking NeuroProtek. A drawback is that often the cognitive impairment returns when the patient ceases taking the treatment. Neuroprotek may be able to normalise mast cell function. Side effects of NeuroProtek are rare however caution is advised if the patient is concurrently taking drugs that are metabolised by the liver as NeuroProtek may alter the blood levels of these substances. The dosage of NeuroProtek is dependent on the patient’s weight, with a daily dose being 2 capsules taken per 20kg 44lbs of body weight. The maximum dose, regardless of body weight is 8 capsules per day. Capsules should be taken with food and the dosage spread out across the day. Nicotine Gum https://livingwithchronicfatiguesyndrome.wordpress.com/2015/02/01/sulforaphane-nicotine-gum-curcumin-and-vns/ Former ME/CFS specialist, Dr. Goldstein wrote fondly of Nicotine Gum as a treatment for ME/CFS. He noted that patients experienced an improvement in energy, cognition and mood as a result of this treatment although did caution that some patients may get worse. It potentially benefits ME/CFS patients due to inhibiting brain inflammation. Several patients have noted an improvement in cognition and increase in energy as a result of this treatment. Nicotine Gum can be detrimental to those with Crohn’s disease. Dr. Goldstein stipulates that occasional patients will have a worsening of ME/CFS symptoms as a result of taking this treatment. If a patient does improve on this treatment, benefit will be noted soon after taking the gum. One ME/CFS patient took a week before experience more energy. Nicotine may increase blood pressure which may be detrimental if an ME/CFS patient has high blood pressure. Longer term use of nicotine is also conducive to health problems such as addiction, periodontal problems and hair loss. If this treatment is trialled, a low starting dose is imperative. Oxymatrine https://livingwithchronicfatiguesyndrome.wordpress.com/2009/11/03/oxymatrine/ Equilibrant https://livingwithchronicfatiguesyndrome.wordpress.com/2014/01/29/my-me-treatments-a-january-2014-update/ Equilibrant is Dr Chia’s own formulation of Oxymatrine that also contains; Astragalus, Olive Leaf, Liquorice and Shiitake Mushroom. Oxymatrine, derived from the Sophora plant, is thought to be effective against enteroviruses. Dr. Chia has trialled Oxymatrine on 500 ME/CFS patients and has found approximately 52% of his patients improve as a result of taking this treatment. Common side effects of Oxymatrine can include headache, fatigue or an increase in ME/CFS symptoms. Oxymatrine should be avoided by those with autoimmune tendencies or seizure disorders. A low starting dose of Oxymatrine is essential for ME/CFS patients and the dosage should only be titrated upwards after a week. The maximum dosage of this treatment is in the realm of 200mg taken in the morning and 200mg taken in the afternoon. Dr. Chia’s Equilibrant doesn’t list the amount of Oxymatrine in the product however the recommended initial dosages of this product is 1 tablet per day for 1-2 weeks. This is followed by a gradual increase of dose, with patients taking up to a maximum of 6 tablets per day. Piracetam https://livingwithchronicfatiguesyndrome.wordpress.com/2011/04/04/piracetam-for-mecfs/ Piracetam is a supplement that specifically targets enhancing cognition. It may also benefit ME/CFS patients due to increasing blood circulation. A study that gave fatigued patients not necessarily those with ME/CFS Piracetam and Cinnarizine an antihistamine found that patients’ physical fatigue significantly reduced. There exist several similar products to Piracetam that may also benefit ME/CFS patients and these are classed as nootropics. In non-ME/CFS studies, Piracetam has rarely caused side effects. One study ascertained that 12% of subjects experienced sleep disturbances while taking this treatment. If a headache does occur while a patient is taking Piracetam, Choline may be a beneficial tandem treatment. Anecdotally some ME/CFS patients have stated that they can only tolerate a small dose of Piracetam- in the 100mg range. Other patients even find this dose too stimulating. Starting at the normally recommended dosage is not recommended for those with ME/CFS. The dosage of Piracetam used for other indications can be up to 20 grams per day. ME/CFS patients generally require much smaller dosages in the 0.8-4.8 gram range. This dosage is spread out across the day and taken at three different occasions at 8 hour intervals. Different countries have various classifications on Piracetam pertaining to its over-the-counter or prescription status. Post-Exertional Malaise Treatments https://livingwithchronicfatiguesyndrome.wordpress.com/2010/07/18/how-to-gain-relief-from-post-exertional-malaise/ This debilitating and central symptom of ME/CFS is often overlooked by doctors. There exists a range of treatment worth trying that I’ve written about in the attached link that benefit patients to varying degrees once in a ‘crashed’ state. These include; Hydralyte iceblocks, liquorice, D-Ribose, electrolyte solutions, leg elevation, massage, meditation, warm baths or cold baths. ProBoost https://livingwithchronicfatiguesyndrome.wordpress.com/2009/08/25/antiviral-and-immunomodulator-cfs-treatment-i-am-trying/ Also known as thymic protein A, a study found 16 out of 23 ME/CFS patients experienced a normalisation of immune function as a result of taking this treatment. There was a corresponding improvement in the clinical ME/CFS symptoms of patients in this study. Another study examined the use of thymic protein A in 6 ME/CFS patients with high EBV titre levels. Patients experienced an increase in energy and required less sleep to function. There exist several reports online of patients greatly benefiting from ProBoost. Many ME/CFS patients who feel run down or on the precipice of a virus take ProBoost. Side effects as a result of taking ProBoost are rare with occasional patients reporting mild, flu like symptoms when they start this treatment. The dosage used varies depending on whether the patient is taking it as a maintenance dosage- 1 packet a day or are fighting off an acute infection- 3 packets per day. Dr. Teitelbaum recommends that ME/CFS patients take one packet of ProBoost, 3 times a day. Propax with NT Factor https://livingwithchronicfatiguesyndrome.wordpress.com/2011/10/10/my-2011-me-treatments-a-progress-report/ This product contains a number of treatments all in the one formulation. Many of these lone treatments are individually used by ME/CFS patients including; quercetin, L-Glutathione, NAC, grape seed extract, various B supplement and NT factor. A study that was ominously run by the company that produces this product found that those with the symptom of severe fatigue not necessarily ME/CFS experienced a reduction in fatigue by on average 40%. Another study found Propax with NT Factor reduced the fatigue experienced by cancer patients. Propax with NT Factor is potentially a form of ‘lipid replacement therapy’. This entails repairing damage to a patient’s mitochondrial membranes. A study examined lipid replacement therapy’s efficacy on ‘moderately fatigued patients.’ As subjects mitochondrial function improved while taking lipid replacement therapy, their fatigue proportionally reduced. Propax with NT Factor is considered to be a safe product with gastrointestinal symptoms rare but possible. It is recommended that the packet be consumed 2-3 times a day. The tablets in the formulation can be taken with or without food and the soft gel capsule that contains omega-3, EPA and DHA should be taken with food. Ranitidine https://livingwithchronicfatiguesyndrome.wordpress.com/2016/01/11/astaxanthin-b1-variants-elimination-diet-ip-6-naphazoline-and-ranitidine/ Ranitidine is a treatment that former ME/CFS specialist Dr. Goldstein found benefited those with infectious mononucleosis. He then began using this treatment on ME/CFS patients with some success. If Ranitidine is not available over the counter in a country, often the alternative Cimetidine is. Dr. Goldstein has found that about 90% of mononucleosis cases respond to Cimetidine. When an ME/CFS patient does respond to one of these drugs, Dr. Goldstein notes that the recovery is remarkable. Approximately 20% of Dr. Goldstein’s ME/CFS patients respond to this type of drug. Stimulation and headaches are two of the most common side effects of Ranitidine treatment. Dr. Goldstein recommends that 150mg of Ranitidine be taken twice a day. The alternative, Cimetidine, should be taken at 300-400mg. Dr. Goldstein has written that it may take from one hour to one week before a patient notices whether this treatment is working for them. Selenium high dose https://livingwithchronicfatiguesyndrome.wordpress.com/2014/08/05/my-me-treatments-an-august-2014-update/ Numerous patients online have noted great benefit from this treatment. The symptoms that have generally improved in these patients are cognitive ability and energy. High dose Selenium may benefit ME/CFS patients due to its antiviral and strong antioxidant properties. Taking high dose Selenium for more than several months is not recommended as it may increase the chance of toxicity, although Selenium toxicity generally occurs at higher doses the 2400-3000mcg range. Overdosing on Selenium can cause numerous symptoms. The recommended dosage of the high dose Selenium protocol is between 400-800mcg a day. Some ME/CFS patients have noted side effects if they increase the dosage past 400mcg. The Selenium should be taken on an empty stomach to increase absorption. Yeast-free selenomethionine is thought to be the best form of Selenium to take although other forms may benefit certain patients more effectively. Sleep Aids https://livingwithchronicfatiguesyndrome.wordpress.com/2015/09/20/the-best-sleep-aids-for-m-e/ In this link I present various ME/CFS experts’ opinions on sleep aids including many over-the-counter formulations. Sulforaphane https://livingwithchronicfatiguesyndrome.wordpress.com/2015/02/01/sulforaphane-nicotine-gum-curcumin-and-vns/ This compound may benefit ME/CFS patients due to shifting the immune system from Th2 dominant to Th1 dominant. Sulforaphane is also an antioxidant, neuroprotective, defensive against oxidative stress and may improve mitochondrial function. It has been studied in autism and benefited those who took it through a mechanism the authors suspected may be due to inducing a “fever effect.” In the aforementioned autism study, those taking Sulforaphane experienced a tiny increase in their liver enzymes. There is quite some conjecture about the amount of Sulforaphane the body absorbs. This is partly due to the possible discrepancy between the specific forms of Sulforaphane ingested. It is therefore difficult to pinpoint a commonly used dosage. Thiamine high dose https://livingwithchronicfatiguesyndrome.wordpress.com/2013/08/05/an-me-update-august-2013/ Anecdotally, some ME/CFS patients have reported benefits from taking high doses of thiamine vitamin B1. A small study of Fibromyalgia patients found all 3 patients benefiting from high dose thiamine treatment. Thiamine deficiency which can be caused by a defective enzyme system can produce similar symptoms to ME/CFS. A study found that fatigue associated with ulcerative colitis and Crohn’s disease can be caused by a thiamine deficiency and that high doses of thiamine resolved this fatigue. Despite this, across multiple studies examining various disease state, patients have normal blood thiamine levels yet improve significantly when taking high dose thiamine. A study has speculated that this may be due to low cellular thiamine transportation or enzymatic problems. The three Fibromyalgia patients studied experienced no side effects as a result of high dose thiamine. Patients with other disease states taking high dose thiamine have reported insomnia and tachycardia. In the Fibromyalgia- high dose thiamine study, patients started at 600mg of thiamine a day and gradually increased this dose. Abrupt improvement was seen when patients reached 1800mg a day. Anecdotally, ME/CFS patients that have responded to high dose thiamine seem to have an optimal dose that varies from patient to patient. The challenge is to find this optimal dose without exceeding it and experiencing any side effects. If a patient doesn’t respond to thiamine, they may benefit from Benfotiamine or Allithiamine, which may be better absorbed. Vagus Nerve Stimulation https://livingwithchronicfatiguesyndrome.wordpress.com/2015/02/01/sulforaphane-nicotine-gum-curcumin-and-vns/ Dr. VanElzakker has theorised that the vagus nerve being infected could explain many of the features of ME/CFS. The vagus nerve has been implicated in several other illnesses such as epilepsy, with stimulation of the nerve proving beneficial. A study implanted Fibromyalgia patients with a vagus nerve stimulation device with the authors concluding that it was a “useful adjunct treatment.” A less invasive measure to stimulate the vagus nerve involves attaching a TENS machine’s electrode pads to the tragus part of the ear. Vitamin D Vitamin D deficiency can often be a secondary problem that arises when ME/CFS patients are unable to get proper supplementation from sunlight. A retroactive study of 221 ME/CFS patients found that Vitamin D levels were “moderately to severely suboptimal in CFS patients.” Numerous patients online have benefited to some degree from Vitamin D supplementation. Dr. Lapp recommends Vitamin D3 to almost all of his ME/CFS patients. Vitamin D side effects are rare at normal doses yet high Vitamin D may cause weakness, headaches or gastrointestinal symptoms. Some patients gain Vitamin D from sunlight or through daily lower level supplementation in the 1000-2000IU range that is available over-the-counter. To definitively raise Vitamin D levels, a single or once a month for several months prescription dose may be required. This may on occasions be as high as 100,000IU. Blood tests can monitor Vitamin D levels yet there is some conjecture about what levels are considered suboptimal. Studies have suggested that those with any form of chronic illness should try and maintain higher vitamin D levels than the healthy population. About These ListsThe key purpose behind creating the above lists was to show patients who have lost hope that there are treatment ideas for this illness. Another purpose of these lists was to compile much of the information that was spread haphazardly across this blog in a centralised and easy to access location. As I continue to write about other ME/CFS treatments on my blog, I will add them to this treatment page. There are many more treatments that I didn’t include in the above lists but ME/CFS patients may benefit from. The following are just some treatments that may help ME/CFS patients based on either study results or their use by some ME/CFS specialists; various probiotics, Glutathione, N-Acetyl Cysteine, methylation cycle treatments, MAF 314, IV saline solution, Gamma Globulin injections/IV, Lidocaine IV, Valtrex, Valcyte, Ergoloid, Levofolinic Acid, Nifedipine, Galantamine, Ampligen and Rituximab. There seems to be a degree of disease heterogeneity https://livingwithchronicfatiguesyndrome.wordpress.com/2010/10/09/a-meta-analysis-of-the-efficacy-of-graded-exercise-therapy-in-treating-cfs-part-3/ across the entire collection of ME/CFS studies and indeed often within single ME/CFS studies. Some studies require that just the overly broad Oxford Criteria be met for patient inclusion. In contrast, other studies are narrower and demand more severely affected patients sharing more common symptomology. Many ME/CFS studies aren’t adequately funded and hence; don’t have a high number of participants, lack a placebo group and aren’t considered high quality. If these idealistic studies existed, I would have written more about these and the corresponding treatments but unfortunately they don’t. It is for the above reasons that I often place a greater emphasis on what an ME/CFS specialist who has stringently diagnosed ME/CFS has found the clinical response rate of a treatment to be e.g. 30% of responders. This is why I have attempted to include as many clinical observations and comments from ME/CFS specialists as possible in the above lists. Finally, I should emphasise that patients should always consult with their physicians prior to taking any treatment. I am not a doctor and nothing on this blog should be construed as medical advice. It is imperative that patients and their physicians are aware of possible side effects, including those not listed before starting any treatment. Patients should also be aware of possible interactions between any treatment they commence and their current medications. Some treatments listed are recommended for short term use only while other treatments may require up to 6 months of usage before effects may be noticed. ME/CFS patients are renowned for having a higher sensitivity to treatments than patients with other diseases. In many cases it is wise to begin treatments at a lower dose to mitigate the chance of more severe side effects. From: 'DR. JAY GOLDSTEIN: A-Z TREATMENTS' http://www.cfstreatmentguide.com/dr-jay-goldstein-a-z-treatments.htmlA Typical Neurosomatic New Patient Treatment ProtocolAgents tried sequentially Onset of Action Duration of action1. Naphazoline HCL 0.1% gtt ┬OU 2 - 3 seconds 3 - 6 hours2. Nitroglycerin 0.04 mg sublingual 2 - 3 minutes 3 - 6 hours3. Nimodipine 30 mg po 20 - 40 minutes 4 - 8 hours4. Gabapentin 100-800 mg po 30 minutes 8 hours5. Baclofen 10 mg 30 minutes 8 hours6. Oxytocin 5-10 U IM or BIDorSyntocinon 1-2 puffs TID 15 minutes - 72 hrs 12 - 24 hours7. Pyridostigmine 30 - 60 mg po 30 minutes 4 - 6 hours8. Hydralazine 10 - 25 mg po 30 - 45 minutes 6 - 12 hours9. Mexiletine 150 mg po 30 - 45 minutes 6 - 8 hours10. Tacrine 10 mg 30 minutes 4 - 6 hours11. Risperidone 0.25 - 0.5 mg 45 - 60 minutes 8 - 12 hours12. Pindolol 5 mg BID 15 minutes - 7 days 12 hours13. Lamotrigine 25 - 50 mg QD 30 - 45 minutes 24 hours14. Sumatriptan 3 - 6 mg SQ 15 - 30 minutes 16 hours15. Ranitidine 150 mg BID 1 hour - 1 week 12 - 24 hours16. Doxepin HCL elixir 2 - 20 mg HS 1 hour variable17. Sertraline 25 - 50 mg QAMorParoxetine 10 - 20 mg QAM 1 hour - 8 weeks 1 - 2 days18. Bupropion 100 mg TID 30 minutes - 8 weeks 8 - 24 hours19. Nefazodone 100 - 300 mg BID 2 - 8 weeks 24 hours20. Venlafaxine 37.5 - 75 mg BID 1 - 4 weeks 24 hours21. Glycine powder 0.4 Gm/Kg/day in juiceorCycloserine 15 - 20 mg QD 1 hour 24 hours22. Felbamate 400 mg 30 minutes 6 - 8 hours23. Lidocaine 200-300 mgA-Z Treatments Comments are by Dr. GoldsteinAcetazolamide Diamox: This drug is a carbonic anhydrase CA inhibitor which is routinely used as a cerebral vasodilator in nuclear medicine. Patients will occasionally have a reduction in symptomatology with acetazolamide. Acetazolamide 250 mg eliminated the pain of a 41-year-old female patient with post-traumatic fibromyalgia, helped her feel very relaxed, and markedly reduced her other symptoms.Acetyl-L-Carnitine: In theory, a good drug. It should work as an acetyl group donor to increase acetylcholine, and the carnitine has already been shown to be effective in a double-blind experiment by the Drs. Plioplys. Acetyl-L-carnitine also increases the levels of nerve growth factor which are four times normal in the spinal fluid of FMS patients and increases other transmitters like adenosine and ATP. In practice, a semi-dud.Adderall: An amphetamine combination that a few patients find more energizing than plain dexedrine. Only about a third of CFS patients have a good response to stimulants, which act by squeezing dopamine DA and norepiniphrine NE out of neurons and glia. If these transmitters are much too low already, giving stimulants will further lower the signal-to-noise ratio and increase symptoms.Amantadine: A weak NMDA antagonist. Helpful for a few patients. Doses higher than the PDR recommends may be more effective, but there is an increased risk of adverse drug reactions when exceeding this dose. Israelis have given 100 mg IV with good results in neurogenic pain. IV amantadine is not available in the USA. Amantadine, ketamine, dextromethorphan, and a new MNDA antagonist, memantine, can be used in trigger point injections as well as gel applications for local pain.Ambien: The best sleeping pill. Does not cause dependence except in unusual circumstances.Aricept: A cholinesterase inhibitor marketed for Alzheimer's disease. Has the advantage of once-a-day dosing and no requirement for liver function test. Does not work as well as Cognex, perhaps because it is not a potassium channel blocker. Cognex has several effects on neurotransmitters relevant to CFS/FMS.Ascorbic Acid Vitamin C: Recent research into the role of ascorbic acid in the brain which has the highest concentrations of this substance in the entire body has shown that this agent may be beneficial in certain patients with CFS. Ascorbate has been found to be neuroprotective, particularly by inhibiting the redox site of the NMDA receptor and diminishing calcium influx. Trials of high-dose oral ascorbic acid have been generally disappointing. Administration of ascorbic acid is done via IV doses of 25 to 50 grams diluted in half-normal saline of Ringer's lactate over a period of about 90 minutes. Adding magnesium sulfate is recommended because ascorbic acid can cause magnesium shifts from extracellular to intracellular compartments. It is beneficial to add 500 mg of calcium gluconate since ascorbic acid is a calcium chelator and could possibly lower serum calcium. Responders to IV ascorbic acid generally feel considerably better in most respects the day after treatment.Baclofen: A greatly under used medication. A GABA-B agonist with few ADRs, it has an immediate onset of action and is still in my top 10.Vitamin B12: Besides being vital to transmethylation which helps to synthesize NE, B12 2g. orally in AM decreases inappropriate daytime melatonin secretion, thereby aiding in the treatment of the delayed sleep-wake cycle many CFS patients experience. Very large doses 10 g may aid transmethylation.BuSpar: The ideal anxiolytic in all respects except efficacy. Best used as an SSRI augmentation agent, especially combined with Visen not generic Pindolol. Augmentation strategies, of which there are many, do not work nearly as well in CFS as they do in major depression disorder.Clonidine: Another greatly underused drug. Can be good for central pain, ADD, anxiety. Helps all symptoms in some patients. Eliminates nightmares. Safe and cheap. Comes in a patch that lasts all day. Better than Zanaflex, another alpha-2 agonist. Tolerance and depression have not been much of a problem. Adverse drug reactions to clonidine can be reversed by yohimbine, an alpha-2 antagonist. Guanfacine Tenex is a less sedating alpha-2 antagonist with a 24-hour duration of action.Dexedrine: An effective stimulant. Makes some patients calm also. May synergize with Ultram. Desoxyn may be better but has neurotoxicity. Many patients like Adderall more.Depakote: In the CFS population its only value is in migraine prophylaxis, for which it is excellent.Dilantin: Useless in every CFS patient I have treated with it.DHEA: Theoretically excellent, it is a neurosteroid which is a GABA antagonist, not necessarily a good thing for some patients. Pregnenolone should be the best neurosteroid low in PMS.Felbamate Felbatol: Not used much because of requirement for hematologic and liver function test monitoring. Should be tried in every treatment-resistant patient. May work when nothing else does, especially for intractable headaches. It may cause headaches, however. There's no free lunch.Gabapentin Neurontin: Gabapentin, an antiepileptic drug with a novel mechanism of action, has become one of my five favorite medications the others are oxytocin, nimopidine, baclofen, and intravenous lidocaine to treat neurosomatic disorders.Gabitril: The only GABA reuptake inhibitor like Prozac is a serotonin reuptake inhibitor. Very effective and very safe if you follow PDR dosing suggestions. Increase the dose too rapidly and the patient may get delirious or manic. Effects are reversible with flumazenil if necessary.Gingko Biloba: Useful only for sexual dysfunction induced by serotonin reuptake inhibitors SRIs. Inhibits platelet aggregation. Rare reports of brain hemorrhage. This adverse reaction raises the risk/benefit ratio.Ginseng Saponins: Works a little like nitroglycerin, which converts to nitric oxide. Increases energy slightly.Gotu Kola: A mild stimulant with no apparent adverse reactions.Honey Bee Venom: As with any "natural product," bee venom has a multitude of ingredients. Patients should be skin tested for bee venom allergy first. Major constituents from my point of view are phospholipase A2 PLA2, which makes arachidonic acid, the precursor to eicosanoids prostaglandins, leukotrienes, etc., dopamine and NE. When it works, the patient often feels like he has been injected with rocket fuel. Effects last about one to two weeks. Has made three patients worse, two of whom were father and daughter. Patients should have an Epi-Pen if available and an antihistamine with them at all times. Plaquenil antagonizes PLA2. Arachidonic acid combines with effianolamine in the brain to make anandamide, an endogenous cannabinoid like marijuana.H2 Receptor Antagonists: The first treatments I developed for CFS were cimetidine and ranitidine. I based this therapy on my successful experience treating acute infectious mononucleosis with cimetidine. When a CFS patient responds to an H2 antagonist I use ranitidine, the onset of action is similar to that seen in acute infectious mononucleosis, i.e. one or two days at a dose of 150 mg b.i.d. Usually all symptoms are ameliorated. Some patients are unable to take any does of ranitidine because it makes them “hyper.”Hydergine: The most underused effective medication in the PDR. Extremely safe. A dopamine and acetylcholine agonist. There is nothing else like it. Other dopamine agonists seem to be restricted in action to the nigrostriatal dopaminergic tract, which is not important in CFS symptoms. Not the case with Hydergine, which is quite helpful for alertness, especially in those sedated by Baclofen. As with most medications listed, it can sometimes help all symptoms.Oxytocin: Oxytocin has a wide range of behavioral effects. Oxytocin neurons project to many areas of the limbic system, as well as to the frontal cortex. Oxytocin is involved in maternal behavior, female and male sexual behavior, feeding, social behavior, and memory. It also has effects on cardiovascular, autonomic, and thermoregulatory processes. Approximately one-fifth of my patients have a good response to IM oxytocin after failing to respond to numerous oral agents. Cognitive clarity is the most responsive symptom, with fibromyalgia and pain being second.Kava-Kava: One of the two best "natural products" for CFS. May take up to eight weeks to have an effect. No adverse drug reactions.Ketamine: The best single agent for CFS/FMS and all other neurosomatic disorders. Known best as an NMDA receptor antagonist the NMDA receptor is one of the several receptors for the excitatory amino acid glutamate, it increases dopamine in the limbic system, a very important objective in CFS. I administer it by slow intravenous infusion or in PLO gel for transdermal through the skin absorption. The intravenous route is more effective, but transdermal application can be done daily, and if effective, can obviate peaks and valleys and need for IVs. I have seen no cases of Ketamine abuse among my patients. Ketamine is one component of my "resurrection cocktail," for patients who have been bedridden for more than a year and whom I may only see once. The others are IV ascorbate, IV lidocaine, IV thyrotropin- releasing hormone which raises all biogenic amines plus acetylcholine, Nimotop, and Neurontin still the most effective oral agent but is being pushed by Tasmar. I am doing trials with Ketamine eyedrops.Klonopin: The benzodiazepine to use if you are going to use one. Affects neurosteroid biosynthesis.Kutapressin: I don't know how this drug works, but some patients have immediate symptomatic improvement after 2 ml IM. I don't usually prescribe it otherwise since there are so many immediate-acting options. It does increase bradykinin, and adverse drug reactions may be treated with drugs like Vasotec ACE inhibitors.Lamictal: One of the new anti-epileptic drugs. All of them increase GABA, and most of them are N-methyl-d-aspartate NMDA antagonists. Works immediately. The main adverse drug reaction is a rash, which can be minimized by gradual dosage escalations. Affects all symptoms. 50-100 mg of Larnictal and 800-1200 mg of Neurontin have rendered euthymic in 30 minutes every patient with acute manic excitement I have treated. Zyprexa and Rilutek could be added to this cocktail if necessary. Lamictal is also an antidepressant and may also work over four weeks or so.IV lidocaine: In addition to its actions mentioned in Betrayal by the Brain, it also acts as an NMDA antagonist. It is the second best treatment. I have given it about a thousand times without a serious adverse drug reaction. Patients have come with great difficulty from other states or countries with the common lament of "If you can't help me I'm going to kill myself' I hear this about twice a week. At least two patients, achieving complete symptomatic relief with IV lidocaine, returned home and could not find a physician or nursing service to administer it. Since they could not move to southern California, they were again bedridden and had to crawl to the bathroom. Not able to live this way any longer, they committed suicide, a worse outcome than the lidocaine toxicity, which never happens. Many physicians will not prescribe any of the medications I use, even if they help their patients a lot. Some medium-sized cities have not one physician who will care for CFS patients. I must treat them from afar, a hazardous practice medicolegally.Marinol: Marinol-deta-9-tetrahydrocannobinol is a medication I use rarely, because of the medicolegal implications. Among other things, it is a dopamine agonist in the limbic system at the nucleus accumbens, a key structure in CFS, but an indirect one. It is also a calcium channel blocker. A few patients get total symptomatic relief with Marinol when one hundred other medications have failed. One such patient is applying for disability only because she cannot afford it. It is one of the last and best options for treating the diffuse pain of FMS, and is good for atypical facial pain. In five years it should be used routinely in many situations.Methadone: Another drug I don't use very often, and for the same reason, although California has passed a law that physicians cannot be prosecuted for using opioids responsibly to treat chronic pain. Thus, it is less risky for me. Physicians in some states are afraid to prescribe it. It is the opioid of choice. Besides being an agonist at the mu opioid receptor, it is an NMDA receptor antagonist like Ketamine, and blocks the serotonin transporter like SRIs. I described its use as an antidepressant about 15 years ago in the medical literature. It is very cheap, does not produce much opioid euphoria, and often ameliorates all neurosomatic symptoms.Nicotine Patch or Gum: I have been prescribing nicotine in these forms for a long time. Nicotine is analgesic, probably by virtue of its stimulating secretion of dopamine and norepinephrine. It binds to the nicotinic cholinergic receptor and can also have profound effects on mood, energy, and cognition. An occasional patient will have worsening of symptoms with nicotine.Papaverine SA: Marketed many years ago as a vasodilator, this medication will probably be discontinued shortly. It is the only drug available that inhibits adenylate cyclase, thereby increasing cyclic AMP, which you may recall from biology class as being pretty important. There is an experimental antidepressant, rolipram, which has a similar mode of action. It preferentially affects energy, alertness, and cognition, and has very few adverse drug reactions. It is a top-10 drug cheap, too.Pentazocine Talwin:Occasionally, an extremely treatment-resistant individual has felt much better after taking pentazocine plus naloxone Talwin-Nx.Spironolactone Aldactone: Spironolactone a mineralocorticoid receptor antagonist has been used for several years to treat premenstrual syndrome. My experience with spironolactone is that it helps only occasionally, but the effect is rapid 30 minutes or so, and thus can be assessed while the patient is in the office.St. John's Wort Hypericum: The other good "natural" remedy for CFS.Tasmar Tolcapone: Neither an exotic location on the Silk Road nor a Mafia-run turnpike in Chicago, Tasmar is a unique agent. It inhibits the enzyme catechol-ortho-methyltransferase COMT, one of the two enzymes monomine oxidase is the other that metabolizes dopamine and norepinephrine. Tasmar degrades them in the synaptic cleft. I have been waiting for this drug for years. It is marketed for Parkinson's disease, and most physicians have not heard of it yet. It can work as monotherapy, either acutely or after four weeks or so. It may be more effective immediately when combined with a dopamine agonist such as Requip quinpirole or a reversible inhibitor of monoamine oxidase RIMA such as meclobemide, which due to the wisdom of the FDA is available in every other industrialized country in the world but the USA. The package insert advises against combining it with irreversible MAOIs such as Nardil and Pamate, so I have not done so. This combination would leave reuptake as the only mechanism to terminate the post-synaptic effect of catecholamines, although rats do quite well on the two drugs. An accountant, unable to work for three years, is back to work now on meclobemide and Tasmar. Adding Sinemet may enhance the action of Tasmar, since it is metabolized to dopamine. Sinemet may be given instead of Requip or Mirapex, or concomitantly. Requip and Mirapex are useful in that they are D3 agonists also. The D3 receptor is located primarily in the limbic system. Since COMT is a methyl group acceptor, it may work better by combining it with S-adenosylmethionine SAMe, a methyl group donor with no adverse drug reactions, effective in FMS and depression. SAMe is available in many other countries, and certain buyer's clubs will supply you with it. Tasmar inactivates COMT, allowing SAMe to transfer methyl groups to precursors so that more norepinephrine can he formed. This process is termed "transmethylation" and is too complicated to discuss further in this column. Interested readers may consult the work of John R. Sinythies and R.J. Baldessarini and go from there.Topamax: Another new AED, Topamax has a little more affinity for the ANWA glutamate receptor, as well as the NMDA receptor. It has very few adverse drug reactions, and when it works, is quite energizing. Agonists at the third major class of glutamate receptor, the "metabotropic," of which there are of course various subtypes, are being developed as anxiolytics.Viagra: I don't have enough money to buy stock in anything, but buying Pfizer a few months ago would have been almost as good as buying Microsoft in 1985. This drug works by inhibiting type 5 phosphodiesterase, one of the six known enzymes to degrade cyclic GMP as important as cyclic AMP, but maybe not covered in biology class. Type 5 is supposed to be specific for the corpus cavemosurn of the penis and probably the clitoris as well. It is not all that specific, though, at least in my patients, who frequently experience flushing and headache. When Viagra works in CFS/FMS, patients experience a reduction in all symptoms. One patient whom I have been treating for 10 years had not responded to one medication until she took Viagra, whereupon she felt almost normal. Nitroglycerin and hydralazine, which stimulate cyclic GMP by different mechanisms, had not helped her.Zyprexa: One of the new "atypical neuroleptics," with Risperdal and Seroquel, Zyprexa can he used as a sleeping aid, antidepressant, anxiolytic, and of special relevance to my practice, is probably the most effective treatment for borderline personality disorder. You can look up the symptoms in the DSM-IV, personality disorder.SOURCES:“Treatment Protocol for Physicians.” The National Forum: http://www.ncf-net.org/forum/jay.htmDr. Goldstein's summary of his protocol for physicians.Goldstein, Jay A.Betrayal by the Brain: The Neurologic Basis of Chronic Fatigue Syndrome, Fibromyalgia Syndrome, and Related Neural Network Disorders.Binghamton, New York: Haworth Medical Press, 1996.This book is filled with valuable information about how the CFS/ME brain works, and how medications affect it, but you will need a background in biochemistry to make full use of it.“The Neuropharmacology of Chronic Fatigue Syndrome.” Jay Goldstein: http://www.cfids-cab.org/cfs-inform/Optimists/goldstein98.html http://www.cfids-cab.org/cfs-inform/Optimists/goldstein98.htmlIn this article, Dr. Goldstein provides an in-depth discussion of diagnosis, tests, associated disorders, and neurological findings in CFS/ME patients. From these, Dr. Goldstein draws the conclusion that other than limbic encephalopathy there is no other no other mechanism that could create the constellation symptoms found in CFS/ME.--- AMPLIGENFrom: 'CHRONIC FATIGUE SYNDROME: A TREATMENT GUIDE, 2ND EDITION' http://www.cfstreatmentguide.com/chronic-fatigue-syndrome-a-treatment-guide-2nd-edition.htmlPHARMACEUTICALS AND PRESCRIPTION DRUGSAmpligenAntibioticsAnticonvulsants: Neurontin gabapentin, Gabitril tiagabine Lyrica pregabalinAntidepressant Drugs: doxepin, amitriptyline, nortriptyline, desipramine, imipramine, trimipramine, clomipramine,fluoxetine, sertraline, paroxetine, citalopram, excitalopram, bupropion, phenalzine, tranylcypromine,trazadone, venlafaxine, duloxetine, mirtazapineAntifungal Agents: Nystatin, Diflucan, Nizoral, SporanoxAntihistamines: Benadryl diphenhydramine, Claritin loratadine, Allegra fexofenadine, Zyrtec cetirizine, Chlor-Trimeton chlorpheniramine maleate, Atarax and Vistaril hydroxyzine, Dramamine meclizine, DiVertigoAntiviral Agents: acyclovir, famcyclovir, amantadine, valacyclovir, valganciclovirArtesunateBenzodiazepines: clonazepam, diazepam, alprazolamBeta Blockers: propanolol Inderol, atenolol Tenormin, labetalol Normodyne, nebivolol BystolicCalcium Channel Blockers: Nicardipine, Nimodipine, Nifedipine, VerapamilCentral Nervous System Stimulants: Ritalin, Dexedrine, Lonamin, Provigil, StratteraCytotec misoprostolDiamox acetazolamideEpogen ProcritFlexeril cyclobenzaprineFlorinef fludrocortisoneGamma GlobulinGcMAFGuaifenesinH2 Blockers: Tagamet cimetidine and Zantac ranitidineHormones: Growth Hormone, Testosterone, Thyroid Hormones, HydrocortisoneHypnotics: Ambien, Lunesta, Rozerem, XyremKutapressin see: NexavirMidodrineNaltrexone LDNNexavir formerly KutapressinNitroglycerinOxytocinPain Relievers: Aspirin, NSAIDs, Tylenol, Aleve, Ultram, NarcoticsPentoxifyllinePlaquenilPyridostigmine MestinonQuestran cholestyramineRituximabTransfer Factor Yolanda's story click hereFormer model Yolanda Hadid drew cheers and skepticism when she went public with her fight against chronic neurological Lyme disease on “The Real Housewives of Beverly Hills” in 2013. The cameras tagged along as Yolanda, 53, experimented with treatments and struggled to make it to social events, telling castmates and viewers that her chronic disease left her too tired to get out of bed some days. But some accused her of inventing symptoms to gain sympathy, and a few of her fellow Housewives suggested that Yolanda — who is the mother of supermodels Bella and Gigi Hadid — may instead suffer from Munchausen syndrome, a mental disorder in which sufferers feign illness. Yolanda was first diagnosed with Lyme in late 2012, after first being told that she suffered from chronic fatigue syndrome — a diagnosis she said just didn’t feel right. Finally, a doctor in Belgium told Yolanda that her mysterious condition was a case of chronic neurological Lyme disease (a diagnosis that’s controversial among American doctors), which meant that the Lyme bacteria had set up shop in her brain. In her new memoir, “Believe Me” (St. Martin’s Press; out Tuesday), Yolanda reveals the real-life drama behind her on-screen struggle, and the dozens of experimental procedures she underwent to fight her disease, from international stem-cell transfusions to thrice-weekly colonics, along with alternative herbal treatments, including magic mushrooms in Bali and an Ayahuasca ceremony in California. “I had a lot of balls to do what I did — driving across the border to Tijuana , Mexico, in the middle of the night, and doing crazy treatments,” Yolanda tells The Post. “It’s crazy, but it was do-or-die for me. When I was in it, I had no fear.” Yolanda’s attempts at curing Lyme — detailed in her book and below — may seem excessive, but she says that she was desperate to find something to cure her aches, brain fog, vision loss and other symptoms of the disease. “You keep thinking, ‘One more week, two weeks, 90 days of antibiotics and I’ll be back in the game,’” she says. The stakes were raised when, a few years into her own fight, two of her children — 20-year-old model Bella and 18-year-old Anwar — were diagnosed as well. “People see Bella on the covers of magazines looking so beautiful, but they don’t know the heartache she has, and pain and joint ache and exhaustion that she faces seven days of the week,” Yolanda says. Yolanda, a successful model herself, was previously married to real estate tycoon Mohamed Hadid and, during her Lyme disease fight, music big shot David Foster. Yolanda and Foster divorced in 2016, after he reportedly told her that her “sick card was up.” Hadid brought her kids Gigi (from left), Anwar, and Bella to the Global Lyme Alliance benefit in 2015, where she revealed that Bella and Anwar also have the disease. But nearly six years after her initial diagnosis, Yolanda says that the financial burden of Lyme was astounding. Based on details revealed in the book and current rates for some of the treatments, she must have spent upward of $150,000 trying to cure herself. “I never kept a tally and I didn’t count it, but I can tell you that it’s a lot,” Yolanda says. “People spend their life savings on finding a cure, and there is no cure.” She’s even learned how to give herself IVs — setting up a temporary treatment lab in her guest bedroom — to keep her costs down. Yolanda’s health has steadily improved over the past year, but she hasn’t given up the fight. “I’m still on a very strict holistic plan, which really supports my immune system, because even in remission, I don’t think I can ever take my foot off the pedal and live my life the way I used to,” she says. Yolanda’s current plan includes twice-a-week vitamin IVs, a “toxin-free” diet and medications prescribed by Dietrich Klinghardt, a Woodinville, Wash.-based doctor who specializes in chronic illness. “I pinch myself every morning because I feel so much gratitude for being alive, and being able to be back working,” she says. Here is a breakdown of Yolanda’s wild health odyssey, which includes some medically questionable and unnecessary procedures. Sponaugle clinic in Florida, about $30,000Yolanda kicked off her treatment attempts in early 2013 with six weeks at Sponaugle, a Lyme-focused clinic in Florida. Experimental treatments included IV drips, colonics, coffee enemas, chiropractic adjustments and large numbers of supplements. She felt better, she says, but it wasn’t the cure she’d hoped for. Hyperthermia: Hadid spent three weeks at a Switzerland clinic which, among other treatments, heated her body to 103 degrees. Paracelsus Clinic in Switzerland, about $30,000 to $45,000Both Yolanda and then-husband David Foster flew to the Paracelsus Clinic in Lustmühle, Switzerland for treatments in September 2013 — three weeks of Lyme-focused procedures for her, and a week of general upkeep for him. She received IV infusions, ozone therapy thought to activate the immune system and a form of acupuncture called neural therapy. She also underwent hyperthermia, spending several hours in a chamber that heated her body to 103 degrees. The heat is supposed to kill viruses and bacteria, although the treatment has only been studied in cancer patients, not those who suffer from Lyme. “The bottom line is that Paracelsus wasn’t a magic bullet for me, and I’m learning that even the best clinics in the world cannot cure chronic Lyme,” she writes. “There is little magic in the world of the chronically ill.” TMS, roughly $14,400 for 36 sessionsTranscranial magnetic stimulation, or TMS, has been shown to help patients with major depression who don’t respond to medication, although Yolanda says that she underwent the procedures at UCLA Medical Center to combat her neurological fog. “After six weeks, my mood feels calmer and my brain function is a little more accessible,” she writes. “But once again, it doesn’t last and certainly is not a cure.” While the FDA-approved treatment can be covered by insurance in certain cases, an out-of-pocket session usually costs around $400. Stem-cell treatment in Tijuana, $30,000In spring 2014, Yolanda made her first trip to Tijuana, Mexico, for an embryonic stem-cell treatment with William Rader. (The treatment isn’t legal in the US, and Rader’s medical license was revoked by California authorities for negligence, professional misconduct, and false or misleading advertising, according to the LA Times). She ends up having to walk back across the border in what she describes as “a scene straight out of ‘Dallas Buyers Club,’” and says the energy-lifting results only lasted a few weeks. Ozone therapy in Tijuana: Hadid says that running her blood through a dialysis machine didn’t have lasting effects. Stem-cell harvesting and transplant in South Korea, cost unknownGoing off of a recommendation by fellow Lyme sufferer Ally Hilfiger, Yolanda made two trips to an unnamed doctor in Seoul, South Korea, the first in November 2014 to harvest stem cells, and the second in January 2015 to reinject those cells back into her body once they’ve had a chance to grow. The cells boosted her energy temporarily. “I consider the trips to Korea a big waste of time and money,” she writes. Antiparasitic and antimalaria drugs, $15,000New York-based Lyme expert Richard Horowitz prescribed antiparasite and antimalaria medication to combat Yolanda’s disease in November 2014, which she took for three months. “I’m appalled and infuriated . . . by how expensive these medications are,” she writes. “Just one bottle of Mepron medication is $2,000 and my daily Bicillin shots will be $3,000 per month, and none of it is covered by my health insurance! I want to scream from the rooftops how wrong this is.” Personal health concierge, an estimated $75 to $300 per hourIn winter 2015, Yolanda began working with a patient advocate, LA-based April Daisy White. A former writer, actress and call girl, White tells The Post that she acts as a “frontline detective” for Yolanda and others suffering with Lyme. “When Yolanda first brought me on board, she would say that she needed someone’s brain,” White says. She organized Yolanda’s medical information, booked appointments, kept track of her medications and even traveled with her to Mexico, Seattle and more for appointments. “I lived through many ups and downs with Yolanda,” White says. “She’s a wonderful fighter.” Yolanda worked with White every day in 2015, and now the two work together on an as-needed basis. ‘I had a lot of balls to do what I did — driving across the border to Tijuana, in the middle of the night, and doing crazy treatments.’ Colonics, $390 per weekRegular colonics at the Gentle Wellness Center in Santa Monica, Calif., helped Yolanda expel a 16-inch “monster” she suspects had been living in her body for 20 to 30 years. The discovery kicks off an obsession — Yolanda begins getting colonics three days per week in February 2015, although she says she no longer does the treatment. She even sets up an at-home parasite “lab” in her guest bathroom so she can dissect her own poop and send findings to get tested. Ozone therapy in Tijuana, cost unavailableYolanda headed back down to Tijuana in spring 2015 for a round of Recirculatory Hemoperfusion, or RHP, with chiropractor Louie Yu. He runs blood through a dialysis machine, which filters it and adds ozone, before pumping it back into the other arm. Yolanda marvels at the way the blood is dark when it comes out and red when it goes back in after getting an ozone wash, taking this as a sign that the treatment is working. (In actuality, all blood turns red after oxygen exposure.) Still, the results only last a few days before she feels sicker than before. Infusio treatment center in Frankfurt, $25,000 for two weeksAt the Infusio treatment center in Frankfurt, Germany, Yolanda spent 14 days undergoing a stem-cell treatment in which the cells are extracted, grown for 10 days and then injected back into the body. Ultimately, she says, the April 2015 procedure “didn’t work.” Adipose stem-cell treatment in the Bahamas, cost unavailableGoing off of a tip from actress Kelly Preston, Yolanda headed to the Okyanos Cell Therapy center in the Bahamas in June 2015 for an adipose stem-cell treatment, in which cells are harvested from her fat and then injected back into her eyes and nerves. Like her stem-cell treatments before, benefits were short-lived. Explant surgery, an estimated $10,000Thanks to full-body scans in 2015, Yolanda discovered that a burst breast implant was leaking free-floating silicone throughout her body. So she had her two existing implants, plus the silicone that had moved through her body, removed in what’s called explant surgery. The procedure, with Cleveland-based, board-certified reconstructive surgeon Dr. Lu-Jean Feng, starts at $8,250, plus hospital fees, and increases based on existing complications — such as ruptures, as in Yolanda’s case. She credits the silicone removal with kick-starting her current remission. Tvam surgery, cost unavailableTransvascular autonomic modulation, called TVAM, is meant to increase blood flow in patients with nervous system conditions by widening veins with a small inflated balloon, although the FDA warned in a statement this spring that there’s no evidence the surgery is either safe or effective. The FDA cautions that the treatment can lead to burst veins, blood clots, brain damage and even death, and singled out Yolanda’s doctor, Dr. Michael Arata, as promoting its benefits without any proof. Arata’s office tells The Post that he no longer performs the surgery, which Yolanda underwent in July 2016
Cholinergic 'Cholinergic' https://bra.in/7j9N8RFrom: Metabolic and neurophysiologic sequelae of brain injury: a cholinergic hypothesis. - PubMed - NCBI(https://www.ncbi.nlm.nih.gov/pubmed/3533278/)Taken in conjunction with data from earlier clinical and laboratory studies, our research also indicates that anticholinergic therapy may potentially benefit head-injured patients. From: Alterations in Cholinergic Pathways and Therapeutic Strategies Targeting Cholinergic System after Traumatic Brain Injury(https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4842943/) Traumatic brain injury (TBI) results in varying degrees of disability in a significant number of persons annually. The mechanisms of cognitive dysfunction after TBI have been explored in both animal models and human clinical studies for decades. Dopaminergic, serotonergic, and noradrenergic dysfunction has been described in many previous reports. In addition, cholinergic dysfunction has also been a familiar topic among TBI researchers for many years. Although pharmacological agents that modulate cholinergic neurotransmission have been used with varying degrees of success in previous studies, improving their function and maximizing cognitive recovery is an ongoing process. In this article, we review the previous findings on the biological mechanism of cholinergic dysfunction after TBI. In addition, we describe studies that use both older agents and newly developed agents as candidates for targeting cholinergic neurotransmission in future studies. Key words: :acetylcholine, cholinergic, nicotinic, traumatic brain injury Go to:(https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4842943/ "Go to other sections in this page") Introduction Traumatic brain injury (TBI) is a common cause of death and disability worldwide. Among the survivors of TBI in the United States, 70,000 to 90,000 have substantial long-term loss of cognitive function that results in a lifetime of disability.^1 Neuropsychological tests that assess various aspects of behavior such as social function, cognitive abilities, and psychiatric symptoms at 10–20 years after TBI show significant behavioral impairment at such chronic time points.^2 Specifically, there are problems in memory, attention, and information processing among many others. Much has been discovered about the biological mechanisms of injury, which includes oxidative stress, inflammation, neurotransmitter dysfunction, and mitochondrial dysfunction. Development of pharmacological treatment for persons with TBI, however, has been difficult because of the wide heterogeneity of disease and mechanisms of injury.^3 Acetylcholine (ACh) is a neurotransmitter that is composed of an ester of acetic acid and choline, and it is effective in regulating plasticity and arousal among many other functions. Cholinergic neurotransmission is a crucial factor in regulation of cognitive function, specifically in learning and memory,^4 as well as attention.^5 Both the septo-hippocampal cholinergic and the nucleus basalis-neocortical cholinergic pathways are important components of the neural circuitry of cognition. In the septo-hippocampal pathway, neurons of the medial septum and the diagonal band of Broca innervate the hippocampus via the fimbria–fornix bundle and the supracallosal striae. The nucleus basalis consists of a collection of magnacellular cholinergic neurons in the basal forebrain that provide diffuse, predominantly ipsilateral, projections to most of the cerebral cortex. Cholinergic inputs to the medial prefrontal cortex of rats mediate attentional processing,^6 and cholinergic inputs to hippocampus regulate memory consolidation.^7 In neurodegenerative diseases, such as Alzheimer's disease, loss of cholinergic functions is believed to be an important contributor to cognitive deficits. Similarly, TBI induces dysregulation of the cholinergic system, and this is believed to be one of the significant underlying causes of impairment of cognitive functions. Because of ACh's major role in numerous cognitive processes, the relationship between alterations in cholinergic neurotransmission and cognitive deficits after TBI has been investigated in many studies. The role of cholinergic dysfunction after TBI leading to long-term deficits in learning and memory have been described previously.^8,9^ As reviewed previously,^9,10^ the cholinergic system exhibits an acute surge in activity leading to massive release of ACh immediately after TBI.^11 Early studies documented acute cholinergic excess in cerebrospinal fluid (CSF) after TBI in humans.^12,13^ At later times, however, there is a persistent reduction in cholinergic function.^14,15^ In agreement with this, several studies have shown that TBI causes direct injury to cholinergic projections. Cholinergic neuronal loss is found in several areas of the forebrain such as the medial septal nucleus and nucleus of the diagonal band of Broca, which have major projections to the hippocampus.^16,17^ Human postmortem studies after TBI reported loss of ACh neurons in the nucleus basalis of Meynert, reflecting a general deficit in the cholinergic neurotramission,^18 and functional imaging of the brain after TBI suggested long-term cholinergic deficits.^19 Overall, the cholinergic system undergoes drastic change throughout the days to months after TBI. Therapeutically attenuating the acute injury to the cholinergic system and enhancing its function chronically has been the challenge of TBI researchers. In this review, we will outline the alterations in various components of the cholinergic system after TBI in both animal models and human clinical studies. Pharmacological agents targeting ACh neurotransmission have been shown in many studies to attenuate cognitive deficits in both neurodegenerative diseases as well as acute injury. For example, nicotinic agonists have shown promise in Alzheimer's disease.^20–22^ Similarly, acetylcholinesterase (AChE) inhibitors have been shown to be beneficial in Alzheimer's disease.^23,24^ The therapeutic effects of cholinergic agents on cognitive function were also evidenced in studies of TBI^25–29^as well as stroke.^30,31^ The importance of cholinergic signaling in TBI has been explored by a fair number of studies and reviews. An updated review is currently warranted, however, given the introduction of new pharmacological agents that are receptor specific and recent clinical trials. By reviewing and reinterpreting the studies that used pharmacological agents in the setting of TBI, both the cholinergic pathobiology of TBI as well as future strategies for targeting specific aspects of cholinergic deficit after TBI will be explored. Go to:(https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4842943/ "Go to other sections in this page") Muscarinic Receptors Muscarinic acetylcholine receptors (mAChR) are G-protein coupled receptors that are important for neurogenesis,^32 survival of newborn neurons,^33 and long-term potentiation (Fig. 1(https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4842943/figure/f1/)).^34,35^ These receptors are categorized to five subtypes (M~1–M~5). The M~1, M~3, and M~5 subtypes mediate excitatory function, whereas M~2 and M~4 subtypes mediate inhibitory function. Of particular interest is the M~2 autoreceptor, which is found presynaptically and inhibits ACh release. By activation of this receptor, ACh signaling is modulated by presynaptic feedback inhibition. !(C:\Users\julie\Brains\U01\B02\ead50c47-d204-46cd-8945-cd0ab32ec1d4/.data/md-images/31870dbc-7fd5-4a5d-b0c7-eb30ea3c93c4.webp) FIG. 1.(https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4842943/figure/f1/) Muscarinic acetylcholine receptor (AChR) regulation of ACh regulating enzymes. Activation of M~1, M~3, and M~5 are excitatory, leading to activation of phospholipase C (PLC), then subsequent calcium mediated C-Fos activation. This upregulates acetylcholinesterase (AChE) expression and downregulates choline acetylransferase (ChAT) and vesicular ACh transporter (vAChT) expression. Activation of M~2 and M~4 are inhibitory, however, and can inhibit cyclic AMP (cAMP) mediated signaling. Color image is available online at http://www.liebertpub.com/neu Alterations in mAChRs after TBI Although human postmortem study of inferior temporal gyrus tissue showed no alteration in muscarinic receptor binding,^36 many animal studies showed reduction of mAChR at an early time point after injury ranging from hours to days. Newborn piglets subjected to fluid percussion injury (FPI) had reduced mAChR determined by autoradiography at 6 h after injury.^37 At as early as 2 h after FPI in rats, there was decreased affinity of muscarinic receptor to positron emission tomography (PET) radiotracer in the hippocampus.^38 An autoradiography study in rats also showed early decrease in mAChR affinity in the hippocampus and brainstem at 1 h.^39 Studies using the controlled cortical impact (CCI) model of injury, however, showed a decrease in muscarinic receptors at slightly later time points: the earliest time of mAChR reduction was at 24 h, but no significant decrease was found at 2 h.^40 Similarly, no decrease was detected between the 1–24 h interval, and earliest mAChR deficit was found at 3 days by radioligand binding.^41 This difference in timeline of mAChR downregulation is possibly because of the differences in the nature of injury: FPI induces more diffuse mechanical injury compared with CCI. Although both types of injury produce diffuse axonal injury and cortical contusion injury, CCI's more focal distribution of energy may lead to delayed deficits in the pericontusional regions. In contrast, direct injury to a wider volume of tissue by FPI may lead to earlier changes in mAChR at pericontusional areas. mAChR, however, may also show compensatory increases at later time points, because an increased number of binding sites of mAChR was reported in the hippocampus and neocortex at 15 days after injury.^42 Most of these studies used PET tracer or radioactive ligand nonspecific to muscarinic receptor subtypes, but several studies indicated that this mAChR reduction may be largely because of a decrease in M~2~subtype. A specific autoradiography study differentiating M~1 and M~2 receptors showed that while there was no change in M~1 receptors, there was a significant decrease of M~2 receptors in several regions of the hippocampus.^43 Also, by immunohistochemistry, there was decreased M~2 staining at 2 and 4 weeks after CCI in the hippocampus.^44 This delayed decrease of M~2 receptors in the hippocampus was also confirmed at 4 weeks after CCI by Western blot analysis. Because M~2 receptors are autoreceptors inhibiting ACh release presynaptically, one possible explanation of this specific decrease is a compensatory downregulation of inhibitory autoreceptors to maintain high ACh release chronically. Pharmacological agents targeting mAChRs It is not clear whether these changes in mAChR are compensatory changes induced by injury or if they are direct consequences of injury. Regardless of the cause, several studies have suggested that mAChR blockade acutely after injury may be neuroprotective.^45,46^ TBI leads to acute elevations of ACh,^47 and excessive muscarinic cholinergic receptor activation can lead to epileptic damage.^48,49^ In these studies, injection of cholinergic agents into limbic regions or the hippocampus induced seizure activity as well as local necrosis of the tissue.^48,50^ Thus, administration of scopolamine, a muscarinic antagonist, at early time points after TBI may be neuroprotective by preventing the effects of acute elevations of ACh. Early administration of scopolamine, which has equal affinity for all five mAChR subtypes,^51 attenuates motor deficits,^46,52^ mortality, and weight loss^52,53^ after TBI in rats. Another possible benefit of scopolamine after TBI is by enhancing ACh release at chronic time points after TBI by blockade of the M~2 autoreceptor. Several microdialysis studies showed that scopolamine administration can evoke ACh release in the hippocampus^15,54^ and neocortex^14 at 14 days post-injury, likely by blocking presynaptic autoreceptors. Although the effect of scopolamine on ACh release is compromised in the setting of TBI compared with sham animals,^55 enhancing ACh release at chronic time points when there is decreased cholinergic activity may theoretically improve cognitive function. Thus, depending on the time frame of application, scopolamine can enhance cholinergic signaling by preventing injury (acute) or enhancing neurotransmission (chronic). M~1 vs. M~2 specific agents Similar to the effect of scopolamine administration, specific blockade of M~1 receptors using dicyclomine 15 min before injury reduced motor deficits.^56 In another study, dicyclomine treatment 5 min before injury attenuated the increase in spectrin breakdown products in the CSF after TBI, but it did not reduce neuronal degeneration assessed by fluoro-jade staining.^57 As discussed by Cox and colleagues,^57 functional deficits after TBI can occur in the absence of neuronal death. Thus, the behavioral improvement by dicyclomine treatment may not be because of preventing neuronal death but rather by preventing deficits in cholinergic neurotransmission by reversing sublethal cellular dysfunction such as deficits in long-term potentiation. Although dicyclomine did not affect the level of neuronal death, these findings from behavioral and biomarker studies support the idea that attenuating the effects of acute and excessive activation of ACh receptors (specifically M~1 receptors) is neuroprotective. Similarly, administration of muscarinic M~2 autoreceptor antagonist BIBN99 improves cognitive function as tested by Morris water maze (MWM) after FPI in rats.^25 Unlike the previous studies using dicyclomine, which was administered at the time of the injury, the administration of BIBN99 in this study was continuous for days after injury. Since specific block of M~2 autoreceptors can cause ACh release in the neocortex and hippocampus,^58,59^ the mechanism of BIBN99's effect on behavioral improvement may involve enhancement of ACh release. The therapeutic effect of BIBN99, however, is likely a combination of preventing ACh receptor activation both initially as well as chronically after injury. There was a therapeutic effect when animals were injected from 24 h after TBI and during the time of the MWM task from days 11–15, but not if injections were performed just during the days of MWM task. Previously mentioned scopolamine studies also used early administration after injury to achieve neuroprotection,^45,52,53^ indicating that muscarinic antagonism early after injury is important in inhibiting secondary injury. Targeting both M~1 and M~2 receptors further enhances the therapeutic effect. A partial M~1 agonist and M~2~antagonist, Lu 25-109-T, reduces TBI-induced choline acetyltransferase (ChAT) loss in the forebrain^60 and improves performance in the MWM^61 after TBI. This agent would theoretically activate understimulated M~1 receptors while inhibiting M~2 autoreceptors, thereby exogenously activating ACh receptors and amplifying endogenous ACh release at the same time. In this study, Lu 25-109-T was subcutaneously injected until 15 days post-injury, indicating that maintaining the cholinergic tone may be beneficial during the recovery phase of trauma. In summary, the inhibition of cholinergic receptors at acute time points after TBI by using mAChR specific antagonists such as scopolamine would inhibit the damage induced by excessive ACh release. At later time points, when there is general cholinergic hypofunction, agents with agonist properties for each subtype of receptor should be used to enhance ACh signaling. Go to:(https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4842943/ "Go to other sections in this page") Nicotinic Receptors Activation of nicotinic ACh receptor (nAChR) by binding of an agonist leads to influx of Na^+^ and Ca^2+^ (Fig. 2(https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4842943/figure/f2/)). The degree of permeability of Ca^2+^ depends on the subunit composition of the nAChR, because the α7 subunit containing nAChRs has a much higher Ca^2+^ permeability than the α3 or α4 subunit containing receptors.^62,63^ This property of regulating the intracellular Ca^2+^ level makes it an important mediator of learning and memory, which depends on signal transduction pathways involving extracellular signal-regulated kinase 1/2 (ERK 1/2) and cAMP response element binding protein (CREB).^64 In addition, Ca^2+^permeability makes α7 receptors also a possible contributor to excitotoxicity, because excessive influx of Ca^2+^ activated by glutamate release can lead to neuronal death. !(C:\Users\julie\Brains\U01\B02\ead50c47-d204-46cd-8945-cd0ab32ec1d4/.data/md-images/80ee4dc5-35fd-4eae-a969-785c7458eeff.jpg) FIG. 2.(https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4842943/figure/f2/) Activation of nicotinic α7 receptor and its effects. There are multiple effects of α7 receptor activation, including downstream pathways activating long-term potentiation as well as anti-apoptotic effects. In microglia, there is inhibition of pro-inflammatory cytokine expression. Color image is available online at http://www.liebertpub.com/neu Alterations of nAChRs after TBI Many previous studies have explored nAChR changes in various brain regions after TBI using autoradiography similar to studies exploring mAChR changes. Although one study reported no change in binding of ^3^Hepibatidine, which nonselectively binds to α3 and α4 subunit containing receptors in newborn piglets,^37 other studies report significant alteration in receptor levels. A rat model of injury using ^3^Hepibatidine showed reduction of α3 and α4 subunits in various regions such as the thalamus, hypothalamus, olfactory tubercle, gigantocellular reticular nucleus, and motor cortex^40 as well as subregions within the hippocampus.^41 Similar reduction of α7 nAChR levels were reported by a decrease in ^125^I α-bungarotoxin binding in newborn piglets after FPI in the CA1 region of the hippocampus, thalamus, and superior colliculus.^65 This finding was also correlated with a generalized decrease in α7 nAChR levels in all the brain regions of adult rats after FPI at 2 and 24 h post-injury in the same study. Decreased binding of α7 receptors was also shown after CCI in adult rats in the hippocampus, somatosensory cortex, stratum oriens, and superior colliculus as early as 1 h to 21 days after injury.^41 Compared with this, α3, α4 reduction is delayed, occurring at 72 h to 21 days. These changes in α7 receptors have numerous implications on the mechanisms of secondary injury. Several studies showed that activation of α7 receptors attenuates release of inflammatory mediators from macrophages and microglia.^66–68^ Also, α7 receptors have an anti-apoptotic effect mediated by pathways involving phosphatidylinositol 3-kinase-Akt^69 as well as by ERK1/2.^70 Based on these studies reporting TBI induced changes in nAChR levels, many groups have used pharmacological agents targeting these receptors, aiming to improve molecular and behavioral outcomes. Agents targeting nAChRs Nicotine administration, which would nonspecifically activate both α7 as well as α3 and α4 containing nAChRs, improves spatial learning and memory retention^71 and reverses α7 receptor deficits.^72 Other studies showed therapeutic potential of agents that specifically activate α7 receptors—namely, choline. Dietary treatment using choline, a selective α7 nAChR agonist, for 2 weeks before TBI leads to improved spatial memory function, reduced cortical tissue loss, and microglial activation after TBI.^73 There are multiple effects of choline, however, besides α7 nAChR activation that may aid in neurorecovery. Choline is also an intermediary in ACh formation, and its administration may enhance ACh synthesis. Accordingly, injection of a naturally occurring compound, cytidine 5'\-diphosphocholine (CDP-choline), which is metabolized to form choline, attenuates TBI induced ACh surge in the hippocampus and neocortex as well as enhances spatial memory in rats.^27 In addition, CDP-choline treatment can reduce hippocampal neuronal loss and cortical lesion volume.^74 In a double-blind, placebo-controlled, multicenter trial using CDP-choline for 90 days,^75 no significant cognitive benefit was found, however. The reasons for this lack of agreement between animal studies and human trial are unclear, but may be because of the complexity of human TBI and heterogeneity of the injury mechanism. Choline is also a main building block for phospholipid, which is important for membrane formation, and it is released from damaged cellular membranes after TBI,^76 likely because of phospholipid degradation and decreased circulatory clearance. Thus, its abundant supply after TBI by CDP-choline treatment is believed to aid in stabilization and repair of damaged membranes.^77 Other mechanisms to explain the neuroprotective effects of CDP-choline have been suggested, however, such as increased levels of antioxidant glutathione,^78 which reduces oxidative damage. α7 receptor specific agents Newer pharmacological agents with specific affinity to α7 receptors were used in various brain injury studies.^79–84^ In rats with intracerebral hemorrhage in the striatum, intraperitoneal injection of α7 agonist PNU-282987 reduced the number of activated microglia/macrophages and neuronal loss.^82 In contrast, α4β2 specific agonist RJR-2403 did not ameliorate these neuronal losses induced by intracerebral hemorrhage, supporting the crucial role the α7 receptor has in attenuating brain injury. Because the majority of nAChRs in the striatum are composed of α4β2 and α6β2 subunits, α7 is a minority in neuronal cells. The beneficial effect of α7 activation is thus likely because of its effect on microglia, reducing inflammatory response. Similarly, PNU-282987 was neuroprotective in a subarachnoid hemorrhage model of rats.^83 Its administration decreased cleaved caspase-3 and neuronal cell death. In addition, it improved neurological deficits assessed by spontaneous activity, limb movements, climbing, and various other functions. Aside from enhancing ACh neurotransmission, attenuating inflammation, and enhancing membrane synthesis, α7 receptor activation may be important targets for improving learning and memory. The α7 receptors have high Ca^2+^ permeability and are known to activate ERK ½ signaling^70 and CREB signaling^85 pathways, which are central components of learning and memory.^64 A wide variety of α7 agonists such as choline, GTS-21, SSR-180711A, and PNU-282987 are able to activate this pathway,^86 and positive allosteric modulator PNU-12596 enhances this α7 receptor activation effect, which will be reviewed later. Accordingly, behavioral experiments with α7 agonist AR-R 17779 given to adult rats resulted in improved learning and memory tested in radial maze.^87 These agents have not been tested in a TBI setting but could serve as potential candidates for cognitive function enhancing agents during recovery. Go to:(https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4842943/ "Go to other sections in this page") Alterations in Intracellular Cholinergic Enzymes after TBI Changes in choline acetytransferase and vesicular acetylcholine transporter Changes among the cholinergic neurons have been described in many TBI studies. A commonly used marker of cholinergic neuron is ChAT, a presynaptic enzyme for ACh synthesis and a marker of integrity of presynaptic cholinergic function and structure. Most of the regions of the brain have decrease in either ChAT levels or its activity after TBI. In rats, there is a moderate reduction of ChAT activity in the dorsal hippocampus, frontal and temporal cortices 1 h after injury (25, 32, and 23%, respectively), but there is greater than a 50% increase in ChAT activity in the parietal cortex.^88 Similarly, other studies in rats after FPI showed decreased ChAT positive neurons in the basal forebrain^16^and medial septal nucleus, nucleus of the diagonal band of Broca, and nucleus basalis of Meynert in 10–15 days.^17 Human postmortem studies also show decrease in ChAT activity—there is a 50% reduction of ChAT activity in the inferior temporal gyrus samples after TBI.^36 Reduction of ChAT activity was also found in bilateral cingulate, inferior temporal, and posterior parietal regions.^89 Histological analysis of neurons in the nucleus basalis of Meynert showed significant damage in patients who died after TBI, and decreased intensity of ChAT immunoreactivity was also found in these damaged neurons (survival times 1–300 h, median=27 h).^18 Such decrease in ChAT levels and activity may not only indicate cholinergic neuronal death; ChAT immunoreactivity decrease was not accompanied by changes in cresyl violet-staining in rats after TBI.^60 In support of this, the decrease in ChAT immunoreactive cells after TBI in rats was only transient, and there was no significant difference by 28 days.^16 The decrease in level and activity of ChAT is likely a combination of cholinergic neuronal loss as well as downregulation of the ChAT protein. Another important regulator of ACh neurotransmission is vesicular ACh transporter (vAChT), an enzyme that is responsible for loading ACh into secretory vesicles. This enzyme also has time dependent alteration in levels after TBI: downregulation acutely, but upregulation at subacute to chronic time points. At acute time points after injury (2 h–72 h) vAChT expression is reduced in multiple brain regions including the thalamus, hypothalamus, motor cortex, and basal forebrain in adult rats.^40 Starting at weeks after injury, however, there is an upregulation. Increased hippocampal vAChT protein has been reported using immunohistochemistry and Western blot at 2–4 weeks (but not at 1 day or 1 week after injury).^44 At 4 weeks after injury, there is an increase in mRNA as well as protein levels of vAChT in the hippocampus.^90 This increase is also present at least up to 1 year after injury in the hippocampus as well as the cortex of rats.^91 Both ChAT and vAChT are crucial for the function of presynaptic ACh release. The reported alterations in these studies may reflect a combination of pathological process and compensatory changes. Given the ACh surge at immediate time points after injury, the decrease in vAChT levels may reflect compensatory downregulation to prevent excessive ACh receptor activation. Also, a direct effect of the injury leading to compromised function of presynaptic cholinergic neuronal function may underlie these changes. The increase in vAChT levels at weeks to 1 year after injury, however, correlates with the general behavioral recovery of animals at chronic time points,^91 indicating the compensatory nature of this change. Go to:(https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4842943/ "Go to other sections in this page") AChE Changes after TBI AChE is a crucial regulator of cholinergic neurotransmission that metabolizes acetycholine after its release in the synaptic terminals. By decreasing or increasing its function, the level of ACh activating its receptors can be changed, and thus the strength of ACh signaling is affected. Because the activity level of AChE has been shown to be associated to attention and working memory,^92 there have been several efforts to characterize activity of AChE in different brain regions after TBI to understand the basis of TBI-induced cognitive deficits. Immediately after TBI, massive release of ACh and glutamate causes excitotoxic damage as well as compensatory changes in the regulators of the cholinergic system such as AChE. Alterations in AChE after TBI Several studies reported short-term alterations in AChE activity after TBI. Acutely after injury, basal forebrain showed an increase in AChE activity at 2–24 h, which normalized by 72 h. This increase in basal forebrain AChE activity also occurred in newborn pigs at 6 h after TBI.^93 After exposure to acute stress, such as a forced swim protocol, acute ACh release in the basal forebrain leads to upregulation of AChE mRNA to possibly restore physiological levels of ACh.^94 Thus, AChE expression and activity may be upregulated in the basal forebrain as a compensatory response to acutely increased cholinergic neurotransmission. Stress from restraining also transiently increases ACh levels in the hippocampus of rats.^95 In addition, cold and immobilization stress increased AChE activity in the cerebrum of rats.^96 This increase in AChE activity may have an important contribution to functional losses, because transgenic mice that overexpress AChE have spatial learning and memory deficits.^97 Because application of AChE inhibitors in patients with Alzheimer's disease and enhancing ACh signaling can improve cognitive function,^98 this increase in AChE and subsequent decrease in ACh signaling may underlie post-TBI cognitive deficits. Although the explanation of this AchE activity change has not been thoroughly explored by TBI researchers, a possible mechanism can be gleaned from a previous study using corticohippocampal brain slice. Application of AChE inhibitors to a corticohippocampal brain slice to increase ACh levels and subsequent ACh signaling caused alterations in cholinergic enzymes.^94 AChE mRNA levels were increased, but ChAT and vAChT mRNA were decreased. These alterations occurred 20 min after increase in c-Fos levels, correlating with the expression of enzymes that regulate cholinergic signaling. This bidirectional modulation of cholinergic gene regulation was presumed to be because of the increase in c-Fos levels. The increase in c-Fos has previously been shown to occur in other studies where muscarinic agonists were administered: c-Fos was increased in frontal, cingulate, and retrosplenial cortex.^99,100^ Thus, after TBI, acute increase in ACh have been shown to correlate with signaling cascades leading to AChE overexpression and ChAT and vAChT underexpression via c-Fos. Another study, however, has shown that hippocampus, hypothalamus, and motor cortex has decreased AChE activity acutely (between 2–24 h).^101 AChE activity deficit was also present in the hippocampus in a blast injury model of TBI.^102 AChE activity may not be regulated just by transcriptional change affecting its concentration, but it likely involves additional mechanisms such as release of soluble form of AChE, which has been reported in the setting of hypoxic damage.^103 The regional differences in AChE activity may reflect different mechanisms of control, as well as different levels of cholinergic neurotransmission in these regions. At chronic periods after TBI, there is a general hypofunction of the cholinergic system as evidenced by reduction of ACh synthesis^15 and release.^54 In addition, there is a general decrease in the AChE activity in several cortical areas, likely as a compensatory change for decreased ACh release. PET imaging determined the decrease in AChE activity in human subjects with TBI more than 1 year after injury, with the most prominent decrease found in parieto-occipital regions of the neocortex.^104 These cholinergic deficits may be in part because of dysfunction of the basal forebrain cholinergic system, which has been demonstrated in the past.^16–18^ To reverse these deficits in ACh neurotransmission, cholinesterase inhibitors have been used to increase the availability of cortical ACh by inhibiting enzymatic catabolism of ACh. These agents have been well characterized and studied widely in Alzheimer's disease animal models and clinical patients. These include ENA713, rivastigmine, physostigmine, tacrine, and donepezil. These agents have various differences in central nervous system (CNS) specificity, hepatotixicity, and other peripheral side effects. AChE inhibitor studies in animals and humans The efficacy of physostigmine in treating cognitive deficits after TBI has been observed in many animal studies as well as patients with TBI. In rats with TBI that were given physostigmine by continuous infusion, there was an improvement in locomotor function assessed by rotarod task,^105 attenuation of brain tissue loss, as well as spatial learning and memory deficit assessed by MWM.^106 This study also indicated that not only AChE inhibition alone, but AChE inhibition in combination with continuous training is important for reversing cognitive deficits. Early case studies of TBI patients with physostigmine enhanced several aspects of cognitive function such as improving verbal recall and attention, as well as reducing confusion.^107–109^ Physostigmine also improved memory after TBI assessed by standardized neuropsychological tests.^110 One possible mechanism of physostigmine induced behavioral improvement after TBI is regulation of cerebral blood flow (CBF). As previously shown by Scremin and associates,^111 measurement of CBF with autoradiography techniques showed that the site of impact after TBI has decreased CBF at 2–24 h after injury. Cerebral cortex contralateral to focus of contusion was shown to have hyperemia in this study. Physostigmine reversed this decrease in CBF after TBI in the ipsilateral side and also increased CBF in the contralateral side to the trauma. Because cholinergic activation enhances CBF in the neocortex,^112 hyperemia contralateral to contusion was postulated to be because of increased ACh synthesis and turnover.^76,113^ Thus, the behavioral benefit of physostigmine after TBI may be because of enhancing perfusion after TBI and enhancing neurological function secondarily. Physostigmine, however, has an extremely short half-life and narrow therapeutic window. It has significant systemic side effects, such as reducing heart rate and blood pressure, which has discouraged its use in patients and led to developments of newer AChE inhibitors that have more CNS specific effects. Another AChE inhibitor, ENA713, which diffuses mainly into the CNS, has been used in animal TBI experiments. Its administration improved reflex and motor function in a closed head injury model in rats.^28^Aside from increasing neuronal cholinergic function, ENA713 reduced the disruption of the blood–brain barrier after injury and thus reduced vasogenic edema. The mechanism of this reduction in blood–brain barrier disruption has not been clarified, but this effect is also found with rivastigmine treatment, another AChE inhibitor with central specificity. Rivastigmine ameliorates spatial memory impairments, motor deficits, and edema in a closed head injury in mice.^29 This neuroprotection was dependent on both nicotinic and muscarinic receptors, because using either mecamylamine (nicotinic antagonist) or scopolamine (muscarinic antagonist) prevented neuroprotection. These studies by Chen and coworkers^28,29^ used one-time injection of AChE inhibitor acutely after injury (5 min–2 h). Because these agents would have inhibited AChE for a short term, the improvement in spatial learning ability was attributed to attenuation of damage in the cholinergic system, rather than increased intrasynaptic ACh levels during the days of behavioral testing.^29 Rivastigmine, however, has only a very modest effect that was shown in clinical studies. A randomized, prospective, double-blind study showed no difference between the placebo and rivastigmine treated group.^114 Only a subgroup analysis among moderate to severe injured patients treated with rivastigmine showed improvements in verbal learning/memory and information processing. Similarly, in an open-labeled, multicenter study that was performed as a follow-up, rivastigmine has shown mostly no benefit except in ra apid visual information processing test, a measure of sustained attention, using a subgroup analysis.^115 Tetrahydroaminoacridine (tacrine) is also a centrally acting AChE inhibitor with disappointing results in the previous studies. Administration of tacrine did not improve MWM performance in rats after TBI.^26^Even in sham rats, tacrine worsened MWM performance in a dose dependent manner. This result, however, may be because of the NMDA receptor antagonist property of tacrine.^116 Because inhibition of NMDA receptor after TBI results in profound memory deficits,^117,118^ tacrine's failure to enhance memory is possibly because of its interaction with the NMDA receptors. In addition to this lack of effects, it also has poor tolerance and significant hepatic toxicity, discouraging clinical trials with this drug in patients with TBI.^119 Donepezil: centrally specific agent with less systemic effects Donepezil, a centrally acting AChE inhibitor with a much milder side effect profile than other AChE inhibitors,^120 has recently gained attention as a treatment option for patients with TBI in several initial case studies more than a decade ago.^121,122^ The clinical use of donepezil for cognitive deficits in Alzheimer's disease and anecdotal evidence from several case reports^122,123^ have indicated a therapeutic effect of donepezil in improving cognitive function after TBI. As extensively reviewed by Ballesteros and colleagues,^124 the effect of donepezil was assessed by various neuropsychological tests in several small case series and case reports, as well as randomized controlled trials.^124 Donepezil was shown to improve cognitive function by mini-mental status examinations^122 as well as subjective improvement in vigilance and attention.^125 Other tests have also shown improvements in intelligence quotient,^126 visual memory,^127 verbal learning and memory,^128 affective-behavioral function,^129 and attention and auditory/visual memory.^130 Several studies, however, reported no significant change in cognitive functions after donepezil treatment.^131–133^ The evidence for effectiveness of donepezil was deemed uncertain because of scarcity of data and poor methodological quality of many of these studies.^124 Despite its specificity to central AChE and low toxicity, more studies are needed to validate donepezil's efficacy in patients with TBI. Among these studies using AChE inhibitors, simply increasing the intrasynaptic concentration of ACh or activation of ACh receptors may not be sufficient to result in behavioral improvements after TBI. Repeated AChE inhibitor administration may reduce ACh synthesis, because constant activation of the presynaptic M~2 autoreceptors may inhibit presynaptic release of ACh.^26 Also, excessive stimulation of mAChRs may lead to M~1 receptor downregulation.^134,135^ Because normal signaling leading to cognitive benefit will involve complex and synchronous neurotransmitter release, simply increasing the absolute concentration of synaptic ACh may not be therapeutic. As such, continuous physostigmine infusion with subcutaneous osmotic pump resulted in progressive impairment of locomotor performance at higher doses, whereas a lower dose was able to improve the performance.^105 Also, a higher rate of physostigmine infusion did not lead to improvement in MWM performance after TBI, but there was improvement compared with controls only at lower rate of infusion.^106 With chronic treatment using high dosages, cholinergic neurotransmission may not be enhanced but instead compromised possibly because of the effects on M~2 autoreceptors as well as M~1 receptor downregulation. Aside from several studies having poor design or too few subjects, the heterogeneity of the effects of AChE inhibitors in human trials are also likely because of some studies using optimal doses and other using excessive doses, which compromises cholinergic signaling. Time dependent changes in the cholinergic system: excitotoxicity and chronic traumatic encephalopathy Time dependent changes in cholinergic signaling were mentioned in previous sections of this review. At early time points around TBI, blockade of mAChR was shown to be neuroprotective.^45,46,52,53,56^ Antagonists to muscarinic receptors such as scopolamine and dicyclomine were shown to reduce mortality or behavioral deficits. An important explanation of this neuroprotection is that mAChR blockade prevented cholinergic excitotoxicity. With the excessive activation of these receptors, there is depolarization and elevation of intracellular Ca^2+^ that leads to damaging effects to the neuron. Cholinergic excitotoxicity may also have a role in other major pathologies of the CNS such as ischemic stroke and epilepsy. Application of AChE inhibitors or muscarinic receptor agonists can induce seizures, which can lead to neuronal injury^48,136,137^ suggesting a possible role of excessive cholinergic signaling in epilepsy. In addition, a major pathologic mechanism in ischemic stroke is glutamate excitotoxicity, which can in turn lead to secondary release of excessive ACh and neuronal injury.^138 Although ACh excitotoxicity has been implicated in epilepsy and stroke, the role of this pathologic mechanism will need further future research. At chronic time points, the opposite effect occurs in the cholinergic signaling, because there is a general hypofunction of the system. Reduction of scopolamine evoked ACh release^54 and decrease in nAChR that contain α7, α3, and α2 subunits have been reported.^40,41^ These changes show that there is a degeneration of specific components of the cholinergic neuronal circuitry. After TBI, chronic traumatic encephalopathy (CTE) ensues. Thus, degeneration of specific components of cholinergic signaling (e.g., α7 nAChR) may occur in CTE. The details of which components of the cholinergic signaling pathway degenerate in CTE and the timeline of these events will need further clarification in future studies. Go to:(https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4842943/ "Go to other sections in this page") Future Directions: Using Novel Agents to Enhance Cholinergic Function Future research with agents targeting the cholinergic system will show significant progress as newer agents with receptor specific agonist/antagonist properties are developed. Muscarinic agents that have receptor subtype specific properties, such as BIBN99 and dicyclomine, can be optimally used during times of recovery and rehabilitation. Agents that have a combination of agonist and antagonist properties, such as Lu 25-109-T, could also be used to inhibit M~2 autoreceptors while activating M~1 postsynaptic receptors. In addition, many studies are now showing cognitive enhancement and attenuation of neuroinflammation by selective targeting of α7 nAChRs. Agents such as GTS-21, SSR-180711A, AR\-R17779(https://www.ncbi.nlm.nih.gov/nuccore/R17779), and PNU-282987 may be useful in future TBI studies to show cognitive enhancement. In addition, novel agents such as allosteric modulators that have even more complex function in activation of cholinergic signaling may show significant benefit. Simple injection of nicotinic agonists into an animal may lead to nonspecific activation of cholinergic neurotransmission throughout all the regions of the brain that contain nicotinic receptors. Positive allosteric modulators (PAMs), however, cause more specific activation of cholinergic receptors by enhancing a pre-existing cholinergic signaling. These agents function by enhancing the potency of activation by endogenous nicotinic receptor activation without directly activating or desensitizing the target receptor. There are specific advantages of enhancing cholinergic signaling by PAMs than nonspecific activation by a direct application of nicotinic agonist, as previously reviewed.^139 For example, activation by α7 nAChR specific PAMs preserves the spatiotemporal patterns of endogenous α7 nAChR activation. In addition, unlike direct activation of nicotinic receptors by nicotinic agonists, which is prone to desensitization, the neurocognitive effects induced by α7 PAMs are not reduced by desensitization. Various benefits of PAMs have been demonstrated in previous studies.^140–147^ There are two subtypes of PAMs: Type I, which increases the peak amplitude of agonist induced response, and Type II, which increases the peak in addition to prolonging the current decay. Several of these agents have been used in either hippocampal slice study^141 or behavioral studies to improve cognitive function.^142,146,147^ In addition, α7 nAChR PAM can reduce infarct volume^143 and attenuate motor deficit ^144 in a mouse model of stroke. The exact mechanism of PAM in reducing stroke-induced damage has not been clarified, and future studies are needed to clarify this. These novel agents have not been used in the setting of TBI, but may be potential candidates for future studies given their unique advantages over cholinergic agonists. In the past, nonspecific receptor agonists have been used in an attempt to modulate the cholinergic system after TBI. Newer pharmacological developments, however, continue to provide a variety of agents that are receptor subtype specific and have varying agonist/antagonist properties. Using these agents individually or in combination may be helpful in preventing secondary injury as well as reversing chronic cognitive deficits after TBI.Several lines of clinical and laboratory evidence demonstrate that TBI can produce acute and chronic alterations in cholinergic systems. While therapies that target the cholinergic system have met with some laboratory success, improved therapies are needed for clinical translation in the future. Traumatic brain injury (TBI) results in varying degrees of disability in a significant number of persons annually. The mechanisms of cognitive dysfunction after TBI have been explored in both animal models and human clinical studies for decades. Dopaminergic, serotonergic, and noradrenergic dysfunction has been described in many previous reports. In addition, cholinergic dysfunction has also been a familiar topic among TBI researchers for many years. Although pharmacological agents that modulate cholinergic neurotransmission have been used with varying degrees of success in previous studies, improving their function and maximizing cognitive recovery is an ongoing process. In this article, we review the previous findings on the biological mechanism of cholinergic dysfunction after TBI. In addition, we describe studies that use both older agents and newly developed agents as candidates for targeting cholinergic neurotransmission in future studies.AcetylcholineKey words: :acetylcholine, cholinergic, nicotinic, traumatic brain injury Go to:(https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4842943/ "Go to other sections in this page") Introduction Traumatic brain injury (TBI) is a common cause of death and disability worldwide. Among the survivors of TBI in the United States, 70,000 to 90,000 have substantial long-term loss of cognitive function that results in a lifetime of disability.^1 Neuropsychological tests that assess various aspects of behavior such as social function, cognitive abilities, and psychiatric symptoms at 10–20 years after TBI show significant behavioral impairment at such chronic time points.^2 Specifically, there are problems in memory, attention, and information processing among many others. Much has been discovered about the biological mechanisms of injury, which includes oxidative stress, inflammation, neurotransmitter dysfunction, and mitochondrial dysfunction. Development of pharmacological treatment for persons with TBI, however, has been difficult because of the wide heterogeneity of disease and mechanisms of injury.^3 Acetylcholine (ACh) is a neurotransmitter that is composed of an ester of acetic acid and choline, and it is effective in regulating plasticity and arousal among many other functions. Cholinergic neurotransmission is a crucial factor in regulation of cognitive function, specifically in learning and memory,^4 as well as attention.^5 Both the septo-hippocampal cholinergic and the nucleus basalis-neocortical cholinergic pathways are important components of the neural circuitry of cognition. In the septo-hippocampal pathway, neurons of the medial septum and the diagonal band of Broca innervate the hippocampus via the fimbria–fornix bundle and the supracallosal striae. The nucleus basalis consists of a collection of magnacellular cholinergic neurons in the basal forebrain that provide diffuse, predominantly ipsilateral, projections to most of the cerebral cortex. Cholinergic inputs to the medial prefrontal cortex of rats mediate attentional processing,^6 and cholinergic inputs to hippocampus regulate memory consolidation.^7 In neurodegenerative diseases, such as Alzheimer's disease, loss of cholinergic functions is believed to be an important contributor to cognitive deficits. Similarly, TBI induces dysregulation of the cholinergic system, and this is believed to be one of the significant underlying causes of impairment of cognitive functions. Because of ACh's major role in numerous cognitive processes, the relationship between alterations in cholinergic neurotransmission and cognitive deficits after TBI has been investigated in many studies. The role of cholinergic dysfunction after TBI leading to long-term deficits in learning and memory have been described previously.^8,9^ As reviewed previously,^9,10^ the cholinergic system exhibits an acute surge in activity leading to massive release of ACh immediately after TBI.^11 Early studies documented acute cholinergic excess in cerebrospinal fluid (CSF) after TBI in humans.^12,13^ At later times, however, there is a persistent reduction in cholinergic function.^14,15^ In agreement with this, several studies have shown that TBI causes direct injury to cholinergic projections. Cholinergic neuronal loss is found in several areas of the forebrain such as the medial septal nucleus and nucleus of the diagonal band of Broca, which have major projections to the hippocampus.^16,17^ Human postmortem studies after TBI reported loss of ACh neurons in the nucleus basalis of Meynert, reflecting a general deficit in the cholinergic neurotramission,^18 and functional imaging of the brain after TBI suggested long-term cholinergic deficits.^19 Overall, the cholinergic system undergoes drastic change throughout the days to months after TBI. Therapeutically attenuating the acute injury to the cholinergic system and enhancing its function chronically has been the challenge of TBI researchers. In this review, we will outline the alterations in various components of the cholinergic system after TBI in both animal models and human clinical studies. Pharmacological agents targeting ACh neurotransmission have been shown in many studies to attenuate cognitive deficits in both neurodegenerative diseases as well as acute injury. For example, nicotinic agonists have shown promise in Alzheimer's disease.^20–22^ Similarly, acetylcholinesterase (AChE) inhibitors have been shown to be beneficial in Alzheimer's disease.^23,24^ The therapeutic effects of cholinergic agents on cognitive function were also evidenced in studies of TBI^25–29^as well as stroke.^30,31^ The importance of cholinergic signaling in TBI has been explored by a fair number of studies and reviews. An updated review is currently warranted, however, given the introduction of new pharmacological agents that are receptor specific and recent clinical trials. By reviewing and reinterpreting the studies that used pharmacological agents in the setting of TBI, both the cholinergic pathobiology of TBI as well as future strategies for targeting specific aspects of cholinergic deficit after TBI will be explored. Go to:(https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4842943/ "Go to other sections in this page") Muscarinic Receptors Muscarinic acetylcholine receptors (mAChR) are G-protein coupled receptors that are important for neurogenesis,^32 survival of newborn neurons,^33 and long-term potentiation (Fig. 1(https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4842943/figure/f1/)).^34,35^ These receptors are categorized to five subtypes (M~1–M~5). The M~1, M~3, and M~5 subtypes mediate excitatory function, whereas M~2 and M~4 subtypes mediate inhibitory function. Of particular interest is the M~2 autoreceptor, which is found presynaptically and inhibits ACh release. By activation of this receptor, ACh signaling is modulated by presynaptic feedback inhibition. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4842943/bin/fig-1.jpg FIG. 1.(https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4842943/figure/f1/) Muscarinic acetylcholine receptor (AChR) regulation of ACh regulating enzymes. Activation of M~1, M~3, and M~5 are excitatory, leading to activation of phospholipase C (PLC), then subsequent calcium mediated C-Fos activation. This upregulates acetylcholinesterase (AChE) expression and downregulates choline acetylransferase (ChAT) and vesicular ACh transporter (vAChT) expression. Activation of M~2 and M~4 are inhibitory, however, and can inhibit cyclic AMP (cAMP) mediated signaling. Color image is available online at http://www.liebertpub.com/neu Alterations in mAChRs after TBI Although human postmortem study of inferior temporal gyrus tissue showed no alteration in muscarinic receptor binding,^36 many animal studies showed reduction of mAChR at an early time point after injury ranging from hours to days. Newborn piglets subjected to fluid percussion injury (FPI) had reduced mAChR determined by autoradiography at 6 h after injury.^37 At as early as 2 h after FPI in rats, there was decreased affinity of muscarinic receptor to positron emission tomography (PET) radiotracer in the hippocampus.^38 An autoradiography study in rats also showed early decrease in mAChR affinity in the hippocampus and brainstem at 1 h.^39 Studies using the controlled cortical impact (CCI) model of injury, however, showed a decrease in muscarinic receptors at slightly later time points: the earliest time of mAChR reduction was at 24 h, but no significant decrease was found at 2 h.^40 Similarly, no decrease was detected between the 1–24 h interval, and earliest mAChR deficit was found at 3 days by radioligand binding.^41 This difference in timeline of mAChR downregulation is possibly because of the differences in the nature of injury: FPI induces more diffuse mechanical injury compared with CCI. Although both types of injury produce diffuse axonal injury and cortical contusion injury, CCI's more focal distribution of energy may lead to delayed deficits in the pericontusional regions. In contrast, direct injury to a wider volume of tissue by FPI may lead to earlier changes in mAChR at pericontusional areas. mAChR, however, may also show compensatory increases at later time points, because an increased number of binding sites of mAChR was reported in the hippocampus and neocortex at 15 days after injury.^42 Most of these studies used PET tracer or radioactive ligand nonspecific to muscarinic receptor subtypes, but several studies indicated that this mAChR reduction may be largely because of a decrease in M~2~subtype. A specific autoradiography study differentiating M~1 and M~2 receptors showed that while there was no change in M~1 receptors, there was a significant decrease of M~2 receptors in several regions of the hippocampus.^43 Also, by immunohistochemistry, there was decreased M~2 staining at 2 and 4 weeks after CCI in the hippocampus.^44 This delayed decrease of M~2 receptors in the hippocampus was also confirmed at 4 weeks after CCI by Western blot analysis. Because M~2 receptors are autoreceptors inhibiting ACh release presynaptically, one possible explanation of this specific decrease is a compensatory downregulation of inhibitory autoreceptors to maintain high ACh release chronically. Pharmacological agents targeting mAChRs It is not clear whether these changes in mAChR are compensatory changes induced by injury or if they are direct consequences of injury. Regardless of the cause, several studies have suggested that mAChR blockade acutely after injury may be neuroprotective.^45,46^ TBI leads to acute elevations of ACh,^47 and excessive muscarinic cholinergic receptor activation can lead to epileptic damage.^48,49^ In these studies, injection of cholinergic agents into limbic regions or the hippocampus induced seizure activity as well as local necrosis of the tissue.^48,50^ Thus, administration of scopolamine, a muscarinic antagonist, at early time points after TBI may be neuroprotective by preventing the effects of acute elevations of ACh. Early administration of scopolamine, which has equal affinity for all five mAChR subtypes,^51 attenuates motor deficits,^46,52^ mortality, and weight loss^52,53^ after TBI in rats. Another possible benefit of scopolamine after TBI is by enhancing ACh release at chronic time points after TBI by blockade of the M~2 autoreceptor. Several microdialysis studies showed that scopolamine administration can evoke ACh release in the hippocampus^15,54^ and neocortex^14 at 14 days post-injury, likely by blocking presynaptic autoreceptors. Although the effect of scopolamine on ACh release is compromised in the setting of TBI compared with sham animals,^55 enhancing ACh release at chronic time points when there is decreased cholinergic activity may theoretically improve cognitive function. Thus, depending on the time frame of application, scopolamine can enhance cholinergic signaling by preventing injury (acute) or enhancing neurotransmission (chronic). M~1 vs. M~2 specific agents Similar to the effect of scopolamine administration, specific blockade of M~1 receptors using dicyclomine 15 min before injury reduced motor deficits.^56 In another study, dicyclomine treatment 5 min before injury attenuated the increase in spectrin breakdown products in the CSF after TBI, but it did not reduce neuronal degeneration assessed by fluoro-jade staining.^57 As discussed by Cox and colleagues,^57 functional deficits after TBI can occur in the absence of neuronal death. Thus, the behavioral improvement by dicyclomine treatment may not be because of preventing neuronal death but rather by preventing deficits in cholinergic neurotransmission by reversing sublethal cellular dysfunction such as deficits in long-term potentiation. Although dicyclomine did not affect the level of neuronal death, these findings from behavioral and biomarker studies support the idea that attenuating the effects of acute and excessive activation of ACh receptors (specifically M~1 receptors) is neuroprotective. Similarly, administration of muscarinic M~2 autoreceptor antagonist BIBN99 improves cognitive function as tested by Morris water maze (MWM) after FPI in rats.^25 Unlike the previous studies using dicyclomine, which was administered at the time of the injury, the administration of BIBN99 in this study was continuous for days after injury. Since specific block of M~2 autoreceptors can cause ACh release in the neocortex and hippocampus,^58,59^ the mechanism of BIBN99's effect on behavioral improvement may involve enhancement of ACh release. The therapeutic effect of BIBN99, however, is likely a combination of preventing ACh receptor activation both initially as well as chronically after injury. There was a therapeutic effect when animals were injected from 24 h after TBI and during the time of the MWM task from days 11–15, but not if injections were performed just during the days of MWM task. Previously mentioned scopolamine studies also used early administration after injury to achieve neuroprotection,^45,52,53^ indicating that muscarinic antagonism early after injury is important in inhibiting secondary injury. Targeting both M~1 and M~2 receptors further enhances the therapeutic effect. A partial M~1 agonist and M~2~antagonist, Lu 25-109-T, reduces TBI-induced choline acetyltransferase (ChAT) loss in the forebrain^60 and improves performance in the MWM^61 after TBI. This agent would theoretically activate understimulated M~1 receptors while inhibiting M~2 autoreceptors, thereby exogenously activating ACh receptors and amplifying endogenous ACh release at the same time. In this study, Lu 25-109-T was subcutaneously injected until 15 days post-injury, indicating that maintaining the cholinergic tone may be beneficial during the recovery phase of trauma. In summary, the inhibition of cholinergic receptors at acute time points after TBI by using mAChR specific antagonists such as scopolamine would inhibit the damage induced by excessive ACh release. At later time points, when there is general cholinergic hypofunction, agents with agonist properties for each subtype of receptor should be used to enhance ACh signaling. Go to:(https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4842943/ "Go to other sections in this page") Nicotinic Receptors Activation of nicotinic ACh receptor (nAChR) by binding of an agonist leads to influx of Na^+^ and Ca^2+^ (Fig. 2(https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4842943/figure/f2/)). The degree of permeability of Ca^2+^ depends on the subunit composition of the nAChR, because the α7 subunit containing nAChRs has a much higher Ca^2+^ permeability than the α3 or α4 subunit containing receptors.^62,63^ This property of regulating the intracellular Ca^2+^ level makes it an important mediator of learning and memory, which depends on signal transduction pathways involving extracellular signal-regulated kinase 1/2 (ERK 1/2) and cAMP response element binding protein (CREB).^64 In addition, Ca^2+^permeability makes α7 receptors also a possible contributor to excitotoxicity, because excessive influx of Ca^2+^ activated by glutamate release can lead to neuronal death. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4842943/bin/fig-2.jpg FIG. 2.(https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4842943/figure/f2/) Activation of nicotinic α7 receptor and its effects. There are multiple effects of α7 receptor activation, including downstream pathways activating long-term potentiation as well as anti-apoptotic effects. In microglia, there is inhibition of pro-inflammatory cytokine expression. Color image is available online at http://www.liebertpub.com/neu Alterations of nAChRs after TBI Many previous studies have explored nAChR changes in various brain regions after TBI using autoradiography similar to studies exploring mAChR changes. Although one study reported no change in binding of ^3^Hepibatidine, which nonselectively binds to α3 and α4 subunit containing receptors in newborn piglets,^37 other studies report significant alteration in receptor levels. A rat model of injury using ^3^Hepibatidine showed reduction of α3 and α4 subunits in various regions such as the thalamus, hypothalamus, olfactory tubercle, gigantocellular reticular nucleus, and motor cortex^40 as well as subregions within the hippocampus.^41 Similar reduction of α7 nAChR levels were reported by a decrease in ^125^I α-bungarotoxin binding in newborn piglets after FPI in the CA1 region of the hippocampus, thalamus, and superior colliculus.^65 This finding was also correlated with a generalized decrease in α7 nAChR levels in all the brain regions of adult rats after FPI at 2 and 24 h post-injury in the same study. Decreased binding of α7 receptors was also shown after CCI in adult rats in the hippocampus, somatosensory cortex, stratum oriens, and superior colliculus as early as 1 h to 21 days after injury.^41 Compared with this, α3, α4 reduction is delayed, occurring at 72 h to 21 days. These changes in α7 receptors have numerous implications on the mechanisms of secondary injury. Several studies showed that activation of α7 receptors attenuates release of inflammatory mediators from macrophages and microglia.^66–68^ Also, α7 receptors have an anti-apoptotic effect mediated by pathways involving phosphatidylinositol 3-kinase-Akt^69 as well as by ERK1/2.^70 Based on these studies reporting TBI induced changes in nAChR levels, many groups have used pharmacological agents targeting these receptors, aiming to improve molecular and behavioral outcomes. Agents targeting nAChRs Nicotine administration, which would nonspecifically activate both α7 as well as α3 and α4 containing nAChRs, improves spatial learning and memory retention^71 and reverses α7 receptor deficits.^72 Other studies showed therapeutic potential of agents that specifically activate α7 receptors—namely, choline. Dietary treatment using choline, a selective α7 nAChR agonist, for 2 weeks before TBI leads to improved spatial memory function, reduced cortical tissue loss, and microglial activation after TBI.^73 There are multiple effects of choline, however, besides α7 nAChR activation that may aid in neurorecovery. Choline is also an intermediary in ACh formation, and its administration may enhance ACh synthesis. Accordingly, injection of a naturally occurring compound, cytidine 5'\-diphosphocholine (CDP-choline), which is metabolized to form choline, attenuates TBI induced ACh surge in the hippocampus and neocortex as well as enhances spatial memory in rats.^27 In addition, CDP-choline treatment can reduce hippocampal neuronal loss and cortical lesion volume.^74 In a double-blind, placebo-controlled, multicenter trial using CDP-choline for 90 days,^75 no significant cognitive benefit was found, however. The reasons for this lack of agreement between animal studies and human trial are unclear, but may be because of the complexity of human TBI and heterogeneity of the injury mechanism. Choline is also a main building block for phospholipid, which is important for membrane formation, and it is released from damaged cellular membranes after TBI,^76 likely because of phospholipid degradation and decreased circulatory clearance. Thus, its abundant supply after TBI by CDP-choline treatment is believed to aid in stabilization and repair of damaged membranes.^77 Other mechanisms to explain the neuroprotective effects of CDP-choline have been suggested, however, such as increased levels of antioxidant glutathione,^78 which reduces oxidative damage. α7 receptor specific agents Newer pharmacological agents with specific affinity to α7 receptors were used in various brain injury studies.^79–84^ In rats with intracerebral hemorrhage in the striatum, intraperitoneal injection of α7 agonist PNU-282987 reduced the number of activated microglia/macrophages and neuronal loss.^82 In contrast, α4β2 specific agonist RJR-2403 did not ameliorate these neuronal losses induced by intracerebral hemorrhage, supporting the crucial role the α7 receptor has in attenuating brain injury. Because the majority of nAChRs in the striatum are composed of α4β2 and α6β2 subunits, α7 is a minority in neuronal cells. The beneficial effect of α7 activation is thus likely because of its effect on microglia, reducing inflammatory response. Similarly, PNU-282987 was neuroprotective in a subarachnoid hemorrhage model of rats.^83 Its administration decreased cleaved caspase-3 and neuronal cell death. In addition, it improved neurological deficits assessed by spontaneous activity, limb movements, climbing, and various other functions. Aside from enhancing ACh neurotransmission, attenuating inflammation, and enhancing membrane synthesis, α7 receptor activation may be important targets for improving learning and memory. The α7 receptors have high Ca^2+^ permeability and are known to activate ERK ½ signaling^70 and CREB signaling^85 pathways, which are central components of learning and memory.^64 A wide variety of α7 agonists such as choline, GTS-21, SSR-180711A, and PNU-282987 are able to activate this pathway,^86 and positive allosteric modulator PNU-12596 enhances this α7 receptor activation effect, which will be reviewed later. Accordingly, behavioral experiments with α7 agonist AR-R 17779 given to adult rats resulted in improved learning and memory tested in radial maze.^87 These agents have not been tested in a TBI setting but could serve as potential candidates for cognitive function enhancing agents during recovery. Go to:(https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4842943/ "Go to other sections in this page") Alterations in Intracellular Cholinergic Enzymes after TBI Changes in choline acetytransferase and vesicular acetylcholine transporter Changes among the cholinergic neurons have been described in many TBI studies. A commonly used marker of cholinergic neuron is ChAT, a presynaptic enzyme for ACh synthesis and a marker of integrity of presynaptic cholinergic function and structure. Most of the regions of the brain have decrease in either ChAT levels or its activity after TBI. In rats, there is a moderate reduction of ChAT activity in the dorsal hippocampus, frontal and temporal cortices 1 h after injury (25, 32, and 23%, respectively), but there is greater than a 50% increase in ChAT activity in the parietal cortex.^88 Similarly, other studies in rats after FPI showed decreased ChAT positive neurons in the basal forebrain^16^and medial septal nucleus, nucleus of the diagonal band of Broca, and nucleus basalis of Meynert in 10–15 days.^17 Human postmortem studies also show decrease in ChAT activity—there is a 50% reduction of ChAT activity in the inferior temporal gyrus samples after TBI.^36 Reduction of ChAT activity was also found in bilateral cingulate, inferior temporal, and posterior parietal regions.^89 Histological analysis of neurons in the nucleus basalis of Meynert showed significant damage in patients who died after TBI, and decreased intensity of ChAT immunoreactivity was also found in these damaged neurons (survival times 1–300 h, median=27 h).^18 Such decrease in ChAT levels and activity may not only indicate cholinergic neuronal death; ChAT immunoreactivity decrease was not accompanied by changes in cresyl violet-staining in rats after TBI.^60 In support of this, the decrease in ChAT immunoreactive cells after TBI in rats was only transient, and there was no significant difference by 28 days.^16 The decrease in level and activity of ChAT is likely a combination of cholinergic neuronal loss as well as downregulation of the ChAT protein. Another important regulator of ACh neurotransmission is vesicular ACh transporter (vAChT), an enzyme that is responsible for loading ACh into secretory vesicles. This enzyme also has time dependent alteration in levels after TBI: downregulation acutely, but upregulation at subacute to chronic time points. At acute time points after injury (2 h–72 h) vAChT expression is reduced in multiple brain regions including the thalamus, hypothalamus, motor cortex, and basal forebrain in adult rats.^40 Starting at weeks after injury, however, there is an upregulation. Increased hippocampal vAChT protein has been reported using immunohistochemistry and Western blot at 2–4 weeks (but not at 1 day or 1 week after injury).^44 At 4 weeks after injury, there is an increase in mRNA as well as protein levels of vAChT in the hippocampus.^90 This increase is also present at least up to 1 year after injury in the hippocampus as well as the cortex of rats.^91 Both ChAT and vAChT are crucial for the function of presynaptic ACh release. The reported alterations in these studies may reflect a combination of pathological process and compensatory changes. Given the ACh surge at immediate time points after injury, the decrease in vAChT levels may reflect compensatory downregulation to prevent excessive ACh receptor activation. Also, a direct effect of the injury leading to compromised function of presynaptic cholinergic neuronal function may underlie these changes. The increase in vAChT levels at weeks to 1 year after injury, however, correlates with the general behavioral recovery of animals at chronic time points,^91 indicating the compensatory nature of this change. Go to:(https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4842943/ "Go to other sections in this page") AChE Changes after TBI AChE is a crucial regulator of cholinergic neurotransmission that metabolizes acetycholine after its release in the synaptic terminals. By decreasing or increasing its function, the level of ACh activating its receptors can be changed, and thus the strength of ACh signaling is affected. Because the activity level of AChE has been shown to be associated to attention and working memory,^92 there have been several efforts to characterize activity of AChE in different brain regions after TBI to understand the basis of TBI-induced cognitive deficits. Immediately after TBI, massive release of ACh and glutamate causes excitotoxic damage as well as compensatory changes in the regulators of the cholinergic system such as AChE. Alterations in AChE after TBI Several studies reported short-term alterations in AChE activity after TBI. Acutely after injury, basal forebrain showed an increase in AChE activity at 2–24 h, which normalized by 72 h. This increase in basal forebrain AChE activity also occurred in newborn pigs at 6 h after TBI.^93 After exposure to acute stress, such as a forced swim protocol, acute ACh release in the basal forebrain leads to upregulation of AChE mRNA to possibly restore physiological levels of ACh.^94 Thus, AChE expression and activity may be upregulated in the basal forebrain as a compensatory response to acutely increased cholinergic neurotransmission. Stress from restraining also transiently increases ACh levels in the hippocampus of rats.^95 In addition, cold and immobilization stress increased AChE activity in the cerebrum of rats.^96 This increase in AChE activity may have an important contribution to functional losses, because transgenic mice that overexpress AChE have spatial learning and memory deficits.^97 Because application of AChE inhibitors in patients with Alzheimer's disease and enhancing ACh signaling can improve cognitive function,^98 this increase in AChE and subsequent decrease in ACh signaling may underlie post-TBI cognitive deficits. Although the explanation of this AchE activity change has not been thoroughly explored by TBI researchers, a possible mechanism can be gleaned from a previous study using corticohippocampal brain slice. Application of AChE inhibitors to a corticohippocampal brain slice to increase ACh levels and subsequent ACh signaling caused alterations in cholinergic enzymes.^94 AChE mRNA levels were increased, but ChAT and vAChT mRNA were decreased. These alterations occurred 20 min after increase in c-Fos levels, correlating with the expression of enzymes that regulate cholinergic signaling. This bidirectional modulation of cholinergic gene regulation was presumed to be because of the increase in c-Fos levels. The increase in c-Fos has previously been shown to occur in other studies where muscarinic agonists were administered: c-Fos was increased in frontal, cingulate, and retrosplenial cortex.^99,100^ Thus, after TBI, acute increase in ACh have been shown to correlate with signaling cascades leading to AChE overexpression and ChAT and vAChT underexpression via c-Fos. Another study, however, has shown that hippocampus, hypothalamus, and motor cortex has decreased AChE activity acutely (between 2–24 h).^101 AChE activity deficit was also present in the hippocampus in a blast injury model of TBI.^102 AChE activity may not be regulated just by transcriptional change affecting its concentration, but it likely involves additional mechanisms such as release of soluble form of AChE, which has been reported in the setting of hypoxic damage.^103 The regional differences in AChE activity may reflect different mechanisms of control, as well as different levels of cholinergic neurotransmission in these regions. At chronic periods after TBI, there is a general hypofunction of the cholinergic system as evidenced by reduction of ACh synthesis^15 and release.^54 In addition, there is a general decrease in the AChE activity in several cortical areas, likely as a compensatory change for decreased ACh release. PET imaging determined the decrease in AChE activity in human subjects with TBI more than 1 year after injury, with the most prominent decrease found in parieto-occipital regions of the neocortex.^104 These cholinergic deficits may be in part because of dysfunction of the basal forebrain cholinergic system, which has been demonstrated in the past.^16–18^ To reverse these deficits in ACh neurotransmission, cholinesterase inhibitors have been used to increase the availability of cortical ACh by inhibiting enzymatic catabolism of ACh. These agents have been well characterized and studied widely in Alzheimer's disease animal models and clinical patients. These include ENA713, rivastigmine, physostigmine, tacrine, and donepezil. These agents have various differences in central nervous system (CNS) specificity, hepatotixicity, and other peripheral side effects. AChE inhibitor studies in animals and humans The efficacy of physostigmine in treating cognitive deficits after TBI has been observed in many animal studies as well as patients with TBI. In rats with TBI that were given physostigmine by continuous infusion, there was an improvement in locomotor function assessed by rotarod task,^105 attenuation of brain tissue loss, as well as spatial learning and memory deficit assessed by MWM.^106 This study also indicated that not only AChE inhibition alone, but AChE inhibition in combination with continuous training is important for reversing cognitive deficits. Early case studies of TBI patients with physostigmine enhanced several aspects of cognitive function such as improving verbal recall and attention, as well as reducing confusion.^107–109^ Physostigmine also improved memory after TBI assessed by standardized neuropsychological tests.^110 One possible mechanism of physostigmine induced behavioral improvement after TBI is regulation of cerebral blood flow (CBF). As previously shown by Scremin and associates,^111 measurement of CBF with autoradiography techniques showed that the site of impact after TBI has decreased CBF at 2–24 h after injury. Cerebral cortex contralateral to focus of contusion was shown to have hyperemia in this study. Physostigmine reversed this decrease in CBF after TBI in the ipsilateral side and also increased CBF in the contralateral side to the trauma. Because cholinergic activation enhances CBF in the neocortex,^112 hyperemia contralateral to contusion was postulated to be because of increased ACh synthesis and turnover.^76,113^ Thus, the behavioral benefit of physostigmine after TBI may be because of enhancing perfusion after TBI and enhancing neurological function secondarily. Physostigmine, however, has an extremely short half-life and narrow therapeutic window. It has significant systemic side effects, such as reducing heart rate and blood pressure, which has discouraged its use in patients and led to developments of newer AChE inhibitors that have more CNS specific effects. Another AChE inhibitor, ENA713, which diffuses mainly into the CNS, has been used in animal TBI experiments. Its administration improved reflex and motor function in a closed head injury model in rats.^28^Aside from increasing neuronal cholinergic function, ENA713 reduced the disruption of the blood–brain barrier after injury and thus reduced vasogenic edema. The mechanism of this reduction in blood–brain barrier disruption has not been clarified, but this effect is also found with rivastigmine treatment, another AChE inhibitor with central specificity. Rivastigmine ameliorates spatial memory impairments, motor deficits, and edema in a closed head injury in mice.^29 This neuroprotection was dependent on both nicotinic and muscarinic receptors, because using either mecamylamine (nicotinic antagonist) or scopolamine (muscarinic antagonist) prevented neuroprotection. These studies by Chen and coworkers^28,29^ used one-time injection of AChE inhibitor acutely after injury (5 min–2 h). Because these agents would have inhibited AChE for a short term, the improvement in spatial learning ability was attributed to attenuation of damage in the cholinergic system, rather than increased intrasynaptic ACh levels during the days of behavioral testing.^29 Rivastigmine, however, has only a very modest effect that was shown in clinical studies. A randomized, prospective, double-blind study showed no difference between the placebo and rivastigmine treated group.^114 Only a subgroup analysis among moderate to severe injured patients treated with rivastigmine showed improvements in verbal learning/memory and information processing. Similarly, in an open-labeled, multicenter study that was performed as a follow-up, rivastigmine has shown mostly no benefit except in ra apid visual information processing test, a measure of sustained attention, using a subgroup analysis.^115 Tetrahydroaminoacridine (tacrine) is also a centrally acting AChE inhibitor with disappointing results in the previous studies. Administration of tacrine did not improve MWM performance in rats after TBI.^26^Even in sham rats, tacrine worsened MWM performance in a dose dependent manner. This result, however, may be because of the NMDA receptor antagonist property of tacrine.^116 Because inhibition of NMDA receptor after TBI results in profound memory deficits,^117,118^ tacrine's failure to enhance memory is possibly because of its interaction with the NMDA receptors. In addition to this lack of effects, it also has poor tolerance and significant hepatic toxicity, discouraging clinical trials with this drug in patients with TBI.^119 Donepezil: centrally specific agent with less systemic effects Donepezil, a centrally acting AChE inhibitor with a much milder side effect profile than other AChE inhibitors,^120 has recently gained attention as a treatment option for patients with TBI in several initial case studies more than a decade ago.^121,122^ The clinical use of donepezil for cognitive deficits in Alzheimer's disease and anecdotal evidence from several case reports^122,123^ have indicated a therapeutic effect of donepezil in improving cognitive function after TBI. As extensively reviewed by Ballesteros and colleagues,^124 the effect of donepezil was assessed by various neuropsychological tests in several small case series and case reports, as well as randomized controlled trials.^124 Donepezil was shown to improve cognitive function by mini-mental status examinations^122 as well as subjective improvement in vigilance and attention.^125 Other tests have also shown improvements in intelligence quotient,^126 visual memory,^127 verbal learning and memory,^128 affective-behavioral function,^129 and attention and auditory/visual memory.^130 Several studies, however, reported no significant change in cognitive functions after donepezil treatment.^131–133^ The evidence for effectiveness of donepezil was deemed uncertain because of scarcity of data and poor methodological quality of many of these studies.^124 Despite its specificity to central AChE and low toxicity, more studies are needed to validate donepezil's efficacy in patients with TBI. Among these studies using AChE inhibitors, simply increasing the intrasynaptic concentration of ACh or activation of ACh receptors may not be sufficient to result in behavioral improvements after TBI. Repeated AChE inhibitor administration may reduce ACh synthesis, because constant activation of the presynaptic M~2 autoreceptors may inhibit presynaptic release of ACh.^26 Also, excessive stimulation of mAChRs may lead to M~1 receptor downregulation.^134,135^ Because normal signaling leading to cognitive benefit will involve complex and synchronous neurotransmitter release, simply increasing the absolute concentration of synaptic ACh may not be therapeutic. As such, continuous physostigmine infusion with subcutaneous osmotic pump resulted in progressive impairment of locomotor performance at higher doses, whereas a lower dose was able to improve the performance.^105 Also, a higher rate of physostigmine infusion did not lead to improvement in MWM performance after TBI, but there was improvement compared with controls only at lower rate of infusion.^106 With chronic treatment using high dosages, cholinergic neurotransmission may not be enhanced but instead compromised possibly because of the effects on M~2 autoreceptors as well as M~1 receptor downregulation. Aside from several studies having poor design or too few subjects, the heterogeneity of the effects of AChE inhibitors in human trials are also likely because of some studies using optimal doses and other using excessive doses, which compromises cholinergic signaling. Time dependent changes in the cholinergic system: excitotoxicity and chronic traumatic encephalopathy Time dependent changes in cholinergic signaling were mentioned in previous sections of this review. At early time points around TBI, blockade of mAChR was shown to be neuroprotective.^45,46,52,53,56^ Antagonists to muscarinic receptors such as scopolamine and dicyclomine were shown to reduce mortality or behavioral deficits. An important explanation of this neuroprotection is that mAChR blockade prevented cholinergic excitotoxicity. With the excessive activation of these receptors, there is depolarization and elevation of intracellular Ca^2+^ that leads to damaging effects to the neuron. Cholinergic excitotoxicity may also have a role in other major pathologies of the CNS such as ischemic stroke and epilepsy. Application of AChE inhibitors or muscarinic receptor agonists can induce seizures, which can lead to neuronal injury^48,136,137^ suggesting a possible role of excessive cholinergic signaling in epilepsy. In addition, a major pathologic mechanism in ischemic stroke is glutamate excitotoxicity, which can in turn lead to secondary release of excessive ACh and neuronal injury.^138 Although ACh excitotoxicity has been implicated in epilepsy and stroke, the role of this pathologic mechanism will need further future research. At chronic time points, the opposite effect occurs in the cholinergic signaling, because there is a general hypofunction of the system. Reduction of scopolamine evoked ACh release^54 and decrease in nAChR that contain α7, α3, and α2 subunits have been reported.^40,41^ These changes show that there is a degeneration of specific components of the cholinergic neuronal circuitry. After TBI, chronic traumatic encephalopathy (CTE) ensues. Thus, degeneration of specific components of cholinergic signaling (e.g., α7 nAChR) may occur in CTE. The details of which components of the cholinergic signaling pathway degenerate in CTE and the timeline of these events will need further clarification in future studies. Go to:(https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4842943/ "Go to other sections in this page") Future Directions: Using Novel Agents to Enhance Cholinergic Function Future research with agents targeting the cholinergic system will show significant progress as newer agents with receptor specific agonist/antagonist properties are developed. Muscarinic agents that have receptor subtype specific properties, such as BIBN99 and dicyclomine, can be optimally used during times of recovery and rehabilitation. Agents that have a combination of agonist and antagonist properties, such as Lu 25-109-T, could also be used to inhibit M~2 autoreceptors while activating M~1 postsynaptic receptors. In addition, many studies are now showing cognitive enhancement and attenuation of neuroinflammation by selective targeting of α7 nAChRs. Agents such as GTS-21, SSR-180711A, AR\-R17779(https://www.ncbi.nlm.nih.gov/nuccore/R17779), and PNU-282987 may be useful in future TBI studies to show cognitive enhancement. In addition, novel agents such as allosteric modulators that have even more complex function in activation of cholinergic signaling may show significant benefit. Simple injection of nicotinic agonists into an animal may lead to nonspecific activation of cholinergic neurotransmission throughout all the regions of the brain that contain nicotinic receptors. Positive allosteric modulators (PAMs), however, cause more specific activation of cholinergic receptors by enhancing a pre-existing cholinergic signaling. These agents function by enhancing the potency of activation by endogenous nicotinic receptor activation without directly activating or desensitizing the target receptor. There are specific advantages of enhancing cholinergic signaling by PAMs than nonspecific activation by a direct application of nicotinic agonist, as previously reviewed.^139 For example, activation by α7 nAChR specific PAMs preserves the spatiotemporal patterns of endogenous α7 nAChR activation. In addition, unlike direct activation of nicotinic receptors by nicotinic agonists, which is prone to desensitization, the neurocognitive effects induced by α7 PAMs are not reduced by desensitization. Various benefits of PAMs have been demonstrated in previous studies.^140–147^ There are two subtypes of PAMs: Type I, which increases the peak amplitude of agonist induced response, and Type II, which increases the peak in addition to prolonging the current decay. Several of these agents have been used in either hippocampal slice study^141 or behavioral studies to improve cognitive function.^142,146,147^ In addition, α7 nAChR PAM can reduce infarct volume^143 and attenuate motor deficit ^144 in a mouse model of stroke. The exact mechanism of PAM in reducing stroke-induced damage has not been clarified, and future studies are needed to clarify this. These novel agents have not been used in the setting of TBI, but may be potential candidates for future studies given their unique advantages over cholinergic agonists. In the past, nonspecific receptor agonists have been used in an attempt to modulate the cholinergic system after TBI. Newer pharmacological developments, however, continue to provide a variety of agents that are receptor subtype specific and have varying agonist/antagonist properties. Using these agents individually or in combination may be helpful in preventing secondary injury as well as reversing chronic cognitive deficits after TBI. Several lines of clinical and laboratory evidence demonstrate that TBI can produce acute and chronic alterations in cholinergic systems. While therapies that target the cholinergic system have met with some laboratory success, improved therapies are needed for clinical translation in the future. From: 4. Neurotransmitter Systems • Functions of Cells and Human Body(http://fblt.cz/en/skripta/regulacni-mechanismy-2-nervova-regulace/5-neurotransmisni-systemy/)Cholinergic systemAcetylcholine is the only neurotransmitter containing a quaternary ammonium group.It is the neurotransmitter used in neuromuscular junctions of all vertebrates, ale preganglionic neurons of the autonomous nervous system and all postganglionic parasympathetic neurons. In the CNS it modulates many cortical activities such as arousal, sleep and memory consolidation.Synthesis and inactivation of acetylcholineAcetylcholine (ACh) is an ester of choline and acetic acid. It is synthesised in one step by transferring the acetyl group from acetyl-CoA to choline. This reaction is catalysed by choline acetyltransferase.The brain receives all its choline from the blood. Choline is mostly synthesised in the liver by a triple methylation of ethanolamine; S-adenosylmethionine (SAM) is the donor of methyl groups. Ethanolamine is produced by a decarboxylation of serine.The cholinergic signal is terminated by the serine hydrolase acetylcholine esterase (AChE) bound to the postsynaptic membrane. The hydrolysis produces choline, which is taken up by the presynaptic neuron and recycled, and acetate. The catalytic activity of AChE depends primarily on three amino acid residues – serine, histidine and glutamate (a similar triad exists also in serine proteases with aspartate instead of glutamate). The hydroxyl group of serine attacks the ester bond. AChE is not entirely specific for ACh, it also hydrolyses other choline esters.Cholinergic signalling in the nervous system is mediate by two receptor types with several subtypes:1) Muscarinic receptorsThese are metabotropic receptors coupled to G proteins, which then regulate ion channel opening. The response of the postsynaptic neuron is thus relatively slow. So far five subtypes of muscarinic receptors have been identified. 1. a) M1 receptors These so called neuronal receptors are found in abundance in the CNS, particularly in the hippocampus and cortex. This receptor mediates an excitatory response via a Gq protein starting a signalling cascade leading to a decreased permeability for potassium. It is thought that a decrease in their function or density is one of the causes of dementia. 1. b) M2 receptors Often labelled as cardiac receptors they are expressed in cardiomyocytes but can be found in high densities in neuronal tissues as well. They mediate an inhibitory response via a Gi protein, which activates potassium channels (via its beta-gamma subunit dimer) thus causing membrane hyperpolarization. This is the mechanism by which the vagus nerve exerts its negative chronotropic effect on the sinoatrial node and the negative dromotropic effect on the atrioventricular node. In the CNS M2 receptors act as autoreceptors on presynaptic neurons mediating negative feedback inhibition in the cortex and the hippocampal formation. 1. c) M3 receptors These receptors mediate the cholinergic stimulation of exocrine glands and the contraction of smooth muscles in the GIT and other organs. M3 receptors are coupled with a Gq protein, which increases intracellular calcium concentration via the activation of phospholipase C and the formation of IP3 and DAG from PIP2. Although they exist in the CNS at a relatively low density they can induce a potent emetic effect.The effect of ACh on blood vessels is worth pointing out. While ACh can cause smooth muscle contraction in blood vessels it causes vasodilation. This is not a direct effect on the smooth muscle but rather a heterotropic inhibition of noradrenergic sympathetic activity and the stimulation of NO production in the endothelium.M3 receptors are being intensively studied due to their role in the development of type 2 diabetes. In the CNS they are expressed in areas responsible for the monitoring and regulation of blood glucose levels, i.e. in parts of hypothalamus and parasympathetic nuclei of the brainstem. In the pancreas they are expressed in beta-cells of the islets of Langerhans, which explains why certain antipsychotic agents used to treat schizophrenia may cause blood glucose dysregulation and increase the risk of T2D via blocking M3 receptors. 1. d) M4 receptors This group of receptors is still relatively poorly studied. Their mechanisms of effect is similar to M2 receptors (Gi-protein activating K^+^ channels). They are found mainly in the striatum, where they function mainly as regulatory autoreceptors on cholinergic neurons (the same role as M2 receptors in the hippocampus and other cortical regions).In the striatum M4 receptors attenuate the activity of excitatory D1 receptors, through which dopamine increases the activity of the extrapyramidal motor system. The physiological implications of this interaction are unclear. 1. e) M5 receptors Similar to M1 and M3 receptors M5 receptors are couple with a Gq-protein. Most studies on M5 receptors to date were performed in vitro.2) Nicotinic receptorsThese are ionotropic receptors opening cation channel permeable for sodium and potassium, in some subtypes also for calcium. The basic division is into a muscular type (N~M receptor) present mostly in the neuromuscular junction and a neuronal type (N~M) found in all postsynaptic terminals in autonomic ganglia. In the CNS N~M receptors function as heteroreceptors for other systems (GABA, serotonin, glutamate, dopamine). They increase the permeability for calcium and increase the amount of released neurotransmitters.Cholinergic neurons are found mainly in the basal nucleus of Meynert and in septal nuclei.These neurons project into the cortex and the hippocampus. They play a role in the activation of certain cortical areas and in short term memory consolidation. The neurons of the basal nucleus and medial septum are damaged in Alzheimer’s disease.Another group of cholinergic neurons can be found in the tegmentum of the brainstem, which send their projections into the cerebellum, hypothalamus and lower portions of the CNS. These affect arousal, sleep cycle and are important for the initiation of the REM sleep phase.There are cholinergic interneurons in the striatum, which form a part of the basal ganglia circuit and thus play a role in the regulation of posture, movement initiation and selection of appropriate movement patterns.Clinical correlation:Some acetylcholine esterase inhibitors are used to treat diseases such as Alzheimer’s disease or myasthenia gravis. Some are highly toxic substances such as extremely effective organophosphates. These compounds form a strong covalent bond with the OH group of the serine residue in the active site of the enzyme, which lasts for weeks. Organophosphates are mostly used as insecticides and as such can cause accidental intoxications. There are also highly toxic volatile organophosphates used as nerve gases such as sarin, tabun and VX. Acetylcholine - MEpedia https://me-pedia.org/wiki/Acetylcholine Acetylcholine Imbalance -- Sensitivity to Meds!!! | Phoenix Rising ME/CFS Forums
https://forums.phoenixrising.me/threads/acetylcholine-imbalance-sensitivity-to-meds.56829 Acetylcholine Induced MAJOR LONG-TERM FATIGUE!!! | Phoenix Rising ME/CFS Forums
https://forums.phoenixrising.me/threads/acetylcholine-induced-major-long-term-fatigue.58024 Acetylcholine Choline Deficiency in Chronic Illness - The Hunt for the Missing Egg – Genetic Genie https://geneticgenie.org/article/acetylcholine-deficiency-in-chronic-illness-the-hunt-for-the-missing-egg

National Library of Medicine search for chronic fatigue syndrome
https://www.ncbi.nlm.nih.gov/search/all/?term=chronic%20fatigue%20syndrome
Sample sceenshot
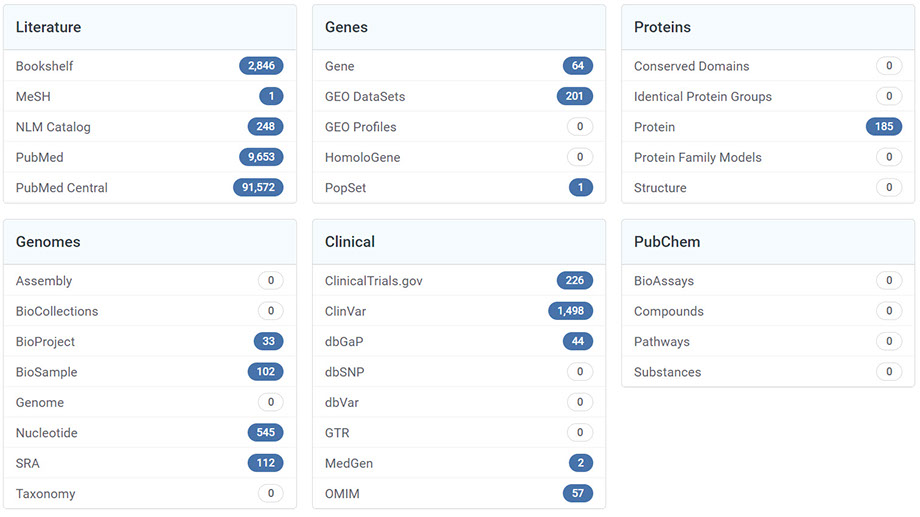
site
CFS is complex there are 7 subsets so what works for some doesn't work for other patients, until it is better understood and medicines developed to address all the issues conditions coconditions
Just as it is a diagnosis of exclusion so the medicine must be administered by trial
When we don't know what specifically our malaise is or where it comes from, then it's best to consider/examine the possible sources. In the attempt to identify (and learn how to manage, and hopefully fix) my Chronic Fatigue Syndrome (itself a 'mystery illness') I have researched a wide gamut of possible threats to our biological entity and systems - as well as studied associated proposed healing modalities.
What I have found is that there are internal and external threats and factors. The external factors I break down into pathogens and toxic substances. Pathogens I then break down into: Virus; Bacteria; Fungus/Mold; Parasites; Myocoplasma; Spirochites (and possibly pleomorphs and retroviruses).
The toxic substances category include many and varied sources including: heavy metals; pesticides/fungicides; phtalates; food additives/dyes/preservatives; a huge list of hormone disrupting chemicals (including BPA, dioxins, atrazine, perchlorate, bromine, perfluorinated chemicals, glycol ethers, arsenic, alkylphenol, Parabens, etc.); volotile organic compounds (VOC's) (sources including cosmetics, asbestos from non \-US made laundry machine belts, dryer sheets, dust, chemical solvents, cleaning products, aspartame, plastics run in dishwasher, offgasing of automotive plastic and mattresses, unshielded microwaves, smartgrid pings, chlorine in shower both absorbed by skin and inhaled as vapor ).
Internal factors may include: one's psychology (being generally at ease and content, versus experiencing stress); diet (getting enough vitamin b12, etc.); sunlight exposure (vitamin D); microbiome balance; hormonal balance; immune system; exercise/flexibility (exercise because our glands only circulate hormones when we are moving, and mostly with up and down motion), etc.
Our microbiome is important as it interacts and affects many biological systems (our immune system; digestive; central nervous system; hormonal system; and psychology/psychobiology). Many attest that fixing one's gut is key. Adressing this includes varied methods such as: drinking bone broth; use of Xifaxan (a perscription medicine); reintroducing probiotics by eating raw organic leafy greens (lightly washed in tapwater and not consuming prewashed/precut packaged greens - as they are first rinsed in chlorine before water, which destroys probiotic microcolonies). The leaves (preferably chard or kale) fold over and protect the colonies as they make their way to the small intestine, where they are needed most (this works considerably better than consuming cheese, yogurt or probiotic capsules). Drinking raw juiced celery before anything in the morning introduces salts required for production of the six types of hydrochloric acid required for digestion.
Regular doctors aren't always able to help, as they often don't have time to keep up on the latest research (especially regarding obscure or 'mystery illnesses'). In fact, there is a 7 to 15 year gap between discoveries published in medical journals and the resulting implementation in practice. Sometimes private specialists or clinics have better insight (but that is costly). To add to the confusion is that there are different kinds of doctors (allopathic; naturopathic; aryuvedic; osteopathic; tcm, etc.).
As testing is expensive, and clinics that specialize in abstruce illnesses are also expensive, I have found it best to do one's own research then find a doctor within the healthcare insurance system who is willing to listen to the latest studies and consider 'alternative' treatment
this report is layed out what has worked for most as well as what is recommended for my specific case in order of what to try, and the associated costs, with much depending on the test results
In my case I have 3 conditions, CFS, OCD and ptbicf. It is likely the tests will find brain and hormone abnormalities and the recommended medicines
depending on which theory and or doctor clinic protocol you follow or which subset you have
Test
Hormone replacement
Pharmaceuticals
non allopathic treatments
review and redo tests, adjust hormonal treatment, try different allopathic and non allopathic treatments
hormone therapy, supplements, amantadine, piracetam, ubi, hbot, fmt, firs, antiparasite, tests,
ketamine tens
stemcell trials
hormone therapy, supplements, amantadine and ldn, antiviral, hbot, firs, tests, hormone therapy, supplements, amantadine, cerblysin, 3pills, hbot, fmt, firs, test etc
psylo, huasca
supplements now, supplements to order, supplements to try
clinics and costs, enroll and mac download and site promo and online journal, etc
CFS is complex there are 7 subsets so what works for some doesn't work for other patients, until it is better understood and medicines developed to address all the issues conditions coconditions
Just as it is a diagnosis of exclusion so the medicine must be administered by trial
![]()
When we don't know what specifically our malaise is or where it comes from, then it's best to consider/examine the possible sources. Several indications of CFS have been reported, including 'altered levels of cytokines (13), immunoglobulins (13), autoantibodies (14), RNase L (15), 2′-5′oligo-adenylate synthetase (15), melatonin (16), dehydroepiandrostenedione (16), growth hormones (17), acylcarnitine (18), folic acid (19), vitamins (20), amino acids (20), carnitine Coenzyme Q10 (20), fatty acids (20) and minerals (20,21). Altered cell populations and activity of the immune system have also been reported (13,22). In addition, alterations in T-cell phenotype and proliferative response, along with the specific signature of the NK cell phenotype, have been reported in certain individuals with CFS (23). Other homeostatic changes involving the opioid system (24) and arginine vasopressin system (24) may be associated with CFS. Furthermore, adrenocorticotropic hormone and the cortisol response appear to be aberrant among patients with CFS (16).
The severe levels of fatigue and disability associated with CFS may be associated with peripheral inflammation and immune activation of blood cells, as is the case with neuroinflammatory and autoimmune illnesses (25). The mental and physical fatigue associated with CFS appears to be the consequence of interactions between multiple systemic and central pathways that take place via immune-inflammatory and neuroinflammatory networks (26). Such interactions would be supported by the activation of cytokines and immune cells, which has been reported in numerous previous studies (27,28' https://www.spandidos-publications.com/mmr/14/3/1875
![]()
https://clinmedjournals.org/Journal-of-Musculoskeletal-Disorders-and-Treatment.php 'Recent findings have identified various causes of CFS/ME, with the common denominator being heavy stress on the body and/or the immune system causing a wide range of mitochondrial dysfunction 14-21. 1. Viral infections, such as Influenza and herpes, infections caused by EBV, CMV, Varicella, HHV6, and HHV7 2. Bacterial infections, such as pneumonia 3. Blood transfusions 4. Physical injuries such as trauma and burn injuries 5. Yeast infections 6. Susceptible immune system 7. Hormonal imbalance 8. Mold exposure 9. Heavy metal exposure 10. Vaccinations 11. Mental health problems, e.g. mental illness, stress, and emotional trauma 12. Genetic predisposition - CFS/ME is more common in blood relations'
![]()
When prescribed steroidal asthma inhalers around the time was exposed to spraypaint, and concurrently prescribed steroidal topical creams for a rash is when developed CFS Corticosteroids given during acute viral infection may trigger myalgic encephalomyelitis https://me-pedia.org/wiki/Corticosteroids_given_during_acute_viral_infection_may_trigger_myalgic_encephalomyelitis call and sue
In the attempt to identify (and learn how to manage, and hopefully fix) my Chronic Fatigue Syndrome (itself a 'mystery illness') I have researched a wide gamut of possible threats to our biological entity and systems - as well as studied associated proposed healing modalities.
What I have found is that there are internal and external threats and factors. The external factors I break down into pathogens and toxic substances. Pathogens I then break down into: Virus; Bacteria; Fungus/Mold; Parasites; Myocoplasma; Spirochites (and possibly pleomorphs and retroviruses).
The toxic substances category include many and varied sources including: heavy metals; pesticides/fungicides; phtalates; food additives/dyes/preservatives; a huge list of hormone disrupting chemicals (including BPA, dioxins, atrazine, perchlorate, bromine, perfluorinated chemicals, glycol ethers, arsenic, alkylphenol, Parabens, etc.); volotile organic compounds (VOC's) (sources including cosmetics, asbestos from non \-US made laundry machine belts, dryer sheets, dust, chemical solvents, cleaning products, aspartame, plastics run in dishwasher, offgasing of automotive plastic and mattresses, unshielded microwaves, smartgrid pings, chlorine in shower both absorbed by skin and inhaled as vapor ).
Internal factors may include: one's psychology (being generally at ease and content, versus experiencing stress); diet (getting enough vitamin b12, etc.); sunlight exposure (vitamin D); microbiome balance; hormonal balance; immune system; exercise/flexibility (exercise because our glands only circulate hormones when we are moving, and mostly with up and down motion), etc.
Our microbiome is important as it interacts and affects many biological systems (our immune system; digestive; central nervous system; hormonal system; and psychology/psychobiology). Many attest that fixing one's gut is key. Adressing this includes varied methods such as: drinking bone broth; use of Xifaxan (a perscription medicine); reintroducing probiotics by eating raw organic leafy greens (lightly washed in tapwater and not consuming prewashed/precut packaged greens - as they are first rinsed in chlorine before water, which destroys probiotic microcolonies). The leaves (preferably chard or kale) fold over and protect the colonies as they make their way to the small intestine, where they are needed most (this works considerably better than consuming cheese, yogurt or probiotic capsules). Drinking raw juiced celery before anything in the morning introduces salts required for production of the six types of hydrochloric acid required for digestion.
Regular doctors aren't always able to help, as they often don't have time to keep up on the latest research (especially regarding obscure or 'mystery illnesses'). In fact, there is a 7 to 15 year gap between discoveries published in medical journals and the resulting implementation in practice. Sometimes private specialists or clinics have better insight (but that is costly). To add to the confusion is that there are different kinds of doctors (allopathic; naturopathic; aryuvedic; osteopathic; tcm, etc.).
As testing is expensive, and clinics that specialize in abstruce illnesses are also expensive, I have found it best to do one's own research then find a doctor within the healthcare insurance system who is willing to listen to the latest studies and consider 'alternative' treatment
In this report is layed out what has worked for most as well as what is recommended for my specific case in order of what to try, and the associated costs, with much depending on the test results
![]()
In my case I have 3 conditions, CFS, OCD and ptbicf. It is likely the tests will find brain and hormone abnormalities and the recommended medicines
depending on which theory and or doctor clinic protocol you follow or which subset you have
Test
- Hormone replacement
- Pharmaceuticals
- Non allopathic treatments
- Review and redo tests, adjust hormonal treatment, try different allopathic and non allopathic treatments
- Hormone therapy, supplements, amantadine, pyracetam, ubi, hbot, fmt, firs, antiparasite, tests,
- Ketamine, tens
stemcell trials
hormone therapy, supplements, amantadine and ldn, antiviral, hbot, firs, tests, hormone therapy, supplements, amantadine, cerblysin, 3pills, hbot, fmt, firs, test etc
psylo, huasca
supplements now, supplements to order, supplements to try
![]()
clinics and costs, enroll and mac download and site promo and online journal, etc
![]()
Nearly half of Americans have one or more chronic diseases, 45% 133 million Americans have one or more, The diagnosis of childhood chronic diseases has almost quadrupled over the past four decades
Swiss researchers found that the Bacillus thuringiensis (Bt) toxin produced for pesticidal purposes by genetically modified (GM) Bt corn can affect the kidney and liver, and somewhat affect the heart, adrenal glands, spleen, and our blood production system.
The BT toxin in corn attacks the friendly bacteria in the human gut which makes it impossible to form a gut barrier which lines the intestines and colon protecting us against pathogens. Dr Rhonda Patrick told us we need Vitamin B complex, a high fiber diet (at lest 35 grams a day) and probiotics to make a gut barrier. The gut barrier in addition to protecting us from pathogens can make fatty acids which attach themselves to macrophages and double their working life. Macrophages are scavengers whose job is to engulf or eat up infecting germs and even infected cells
Poly and perfluoroalkyl substances, more commonly known as PFAS or more commonly as forever chemicals, are everywhere. There are around 4,700 chemicals in the PFAS family. They contain linked chains of carbon and fluorine. Toxic ‘forever chemicals’ are contaminating plastic food containers. Harmful PFAS chemicals are being used to hold food, drink and cosmetics, with unknown consequences. Laboratory animals exposed to high doses of one or more of these PFAS have shown changes in liver, thyroid, and pancreatic function, as well as some changes in hormone levels. PFAS have been linked to obesity, high cholesterol, diabetes, and liver issues etc.
Searches on https://link.springer.com for 'Chronic Fatigue Syndrome' yield thousands of results
click here to download the page below













