Not so much a synopsis but a well deserved rant, did you know that the the NIH won't do studies on CFS but will study long covid? That's good news for us as there's a lot of overlap between CFS and long covid.
AXA1125 A New Mitochondrial Enhancer Is Being Trialed in Long COVID https://www.healthrising.org/blog/2021/11/05/axa1125-mitochondrial-enhancer-long-covid
trials have been chronic fatigue syndrome’s Achilles heel. Except for cognitive behavioral therapy CBT and graded exercise therapy GET, which have dominated the clinical trials arena in ME/CFS to an astonishing amount, biological treatment trials have been few and far between. When they have occurred, they’ve been small and follow-up – even when they’ve had positive results – has been rare.
Numerous treatment trials, however, have already been showing up in long COVID. Just last week Health Rising reported on a budding new long-COVID and ME/CFS treatment called Inspiritol, and others, including fecal transplants, oxaloacetate, are already underway.
The NIH’s quick embrace of long-COVID treatment trials demonstrates just how different the situation is. Apparently out of an abundance of caution, the NIH will not fund any ME/CFS treatment trials. It only wants to move on ME/CFS treatment trials after it believes it’s likely to get a good result. Dr. Koroshetz has said he believes bad results could doom the field for years.
Not so with long COVID. Even though the NIH knows far more about ME/CFS than it does about long COVID, and even though it has yet to release its grant rewards for long COVID research, the NIH has already opened up an “urgent” grant award asking for applications for long COVID treatment trials.
The difference is the NIH has a lot of money to spend on long COVID and Congress – which gave the NIH that money- is watching. The NIH isn’t the only institution, though, that’s pumping money into long COVID treatment trials. A consortium of 30 UK researchers, health professionals, patients, and industry partners called STIMULATE-ICP Symptoms, Trajectory, Inequalities, and Management: Understanding Long-COVID to Address and Transform Existing Integrated Care Pathways plans to run treatment trials in over 4,500 people with long-COVID. Two drugs rivaroxaban and colchicine have already been slated for trials
As if there wasn't already enough to read on this site ! to understand the disparity of funding you can visit the following pages about the lack of NIH testing, but don't let it frustrate you too much remember your cortisol levels! author chuckles and winks
https://www.healthrising.org/blog/2020/07/24/open-letter-covid-19-long-hauler-me-cfs
https://www.healthrising.org/blog/2021/09/18/nih-mammoth-effort-understand-treat-long-covid
https://www.healthrising.org/blog/2021/10/19/mass-nih-funded-chronic-fatigue-research-centers
https://www.healthrising.org/blog/2021/06/10/insights-chronic-fatigue-syndrone-long-covid5802
https://www.healthrising.org/blog/2022/01/24/2022-the-year-ahead-pt-i-the-long-covid-research-boom
the NIH is remiss to test drugs for which the resultant mechanism of action in healing or addressing CFS will remain unknown. In other words, at best a drug can show a correlation to remission but can't be considered cause, and that is not solid enough science to pursue or something of that manner.
Anyways, Nimodipine seems helpful and I'm willing to try it, though there are nootropics that seem even more helpful, so please read on in the site
Skill Level 4
Relevance:3 Technical Level:2
This page may make a huge difference, though it is a lot to read. Recommended to skim and revisit twice and again with a practitioner
page 10 CFS > SUPPLEMENTS and NUTRITION > NOOTROPICS > NIMODIPINE
page 9
page 11

Nimodipine-chronic-fatigue-syndrome-fibromyalgia https://www.healthrising.org/treating-chronic-fatigue-syndrome/drugs/nimodipine-chronic-fatigue-syndrome-fibromyalgia
A Calcium channel blocker and vasodilator that been available in the U.S. for over 30 years, and can be found in over 60 countries world-wide.
Nimodipine is mostly used to suppress blood vessel spasms that can occur during cerebral hemorrhaging and vascular ischemia. It’s ability to increase blood flows in the brain cerebral perfusion could be helpful in ME/CFS and POTS given increasing evidence of reduced brain blood flows and possibly vasoconstricted cerebral blood vessels.
As Susan Parker https://www.actionforme.org.uk/assets/components/discuss/attachments/2/6193/nimodipine%20use%20in%20me,%20jan%202014.pdf points out, Nimodipine is able to easily cross over into the brain, and because it effects the arteries in the brain more than the rest of the body, is unlikely to cause blood pressure issues.
Nimodipine may also be able to regulate immune functioning, enhance mitochondrial activity, reduce pain, and inhibit the activity of the microglial cells in the brain that are believed to be causing neuroinflammation in ME/CFS and fibromyalgia.
![]()
ME/CFS and FM Doctors Report
Dr. Jay Goldstein rated Nimodipine the third most effective of 23 medications for ME/CFS. Dr. Mason Brown, a U.K. doctor, developed a protocol for ME/CFS – of which Nimodipine was the cornerstone – which he claimed was effective in 80% of his patients.
* Dr. Jay Goldstein – the top 23 drugs for chronic fatigue syndrome https://www.healthrising.org/forums/resources/dr-jay-goldsteins-top-23-drugs-for-chronic-fatigue-syndrome-me-cfs.341
One of those was Dr. Kristina Downing-Orr, a psychologist who recovered from a very severe case of ME/CFS. Downing-Orr later wrote a book “Beating Chronic Fatigue Syndrome” outlining Dr. Brown’s protocol as well as a nutritional protocol.
Brown and Downing-Orr use Nimodipine to remove brain toxins neurotoxins they believed built up over the course of the disease. Gingko biloba, eight glasses of filtered water a day, L-Glutamine and evening primrose oil are used in conjunction with Nimodipine to improve brain circulation.
They also used strategies to assist with detoxification, repair the gut, assist the mitochondria, etc. Downing-Orr reported that the healing process was a gradual one, that periods of worsened health could be expected as the toxins were released, and that it would take from one to two years.
Parker lists fast and slow Nimodipine protocols for ME/CFS. Downing-Orr, who emphasizes that the drug may make you feel worse before you feel better, recommends a slow approach that begins with one quarter tablet a day for a week, adds another quarter tablet in the afternoon and slowly working its way up to one tablet total a day by week four. Some patients may need to start lower. Parker reported that some people with ME/CFS may not tolerate even the smallest doses.
Downing-Orr reports that some patients may also need up to two to four tablets a day for a month or more 4-5 months at the most. Bear in mind that both Brown and Downing-Orr considered Nimodipine as one part of a step-by-step multidimensional protocol. Find out more about their protocols here:
The Nimodipine Way? A Review of “Beating Chronic Fatigue: Your Step-by-Step Guide to Complete Recovery” https://www.healthrising.org/blog/2019/06/10/nimodipine-beating-chronic-fatigue-guide-downing-orr
Dr. Marilyn McNeil reported to the British Medical Journal article that small doses of Nimodipine https://www.bmj.com/rapid-response/2011/10/30/possibility-more-rapid-recovery-cfs-may-change-gps-attitudes she never took more than 1 1/4 tablets 37.5 mgs daily allowed her to rapidly recover from a severe case of ME/CFS which left her bed-ridden. Parker provides several success stories including that of a Toronto doctor, Dr. Sherkey, https://www.actionforme.org.uk/assets/components/discuss/attachments/2/6193/nimodipine%20use%20in%20me,%20jan%202014.pdf who reported that one patient, after eight years with ME/CFS, remained almost symptom-free two years after starting Nimodipine.
Parker, herself, was mostly housebound, before recovering 80% of her health using Nimodipine https://www.actionforme.org.uk/assets/components/discuss/attachments/2/6193/nimodipine%20use%20in%20me,%20jan%202014.pdf in combination with other treatments. in 2014 she reported that she can now walk 6 miles a day, and run and dance. Seven years after starting the drug she stated that she needed to remain on the drug 45 mg/day to maintain her health.
Finish author and ME/CFS patient Maija Haavisto reported http://www.fiikus.net/?cfstreatment that Nimodipine markedly improved her brain fog, and put it on her ‘definitely try’ for ME/CFS list. Remy in a major overview of the drug reported that Nimodipine markedly reduced her pain.
![]()
A Calcium Channel Blocker for ME/CFS and Fibromyalgia? Nimodipine Pt. II https://www.healthrising.org/blog/2019/06/12/nimodipine-calcium-channel-blocker-fibromyalgia-chronic-fatigue-pt-ii
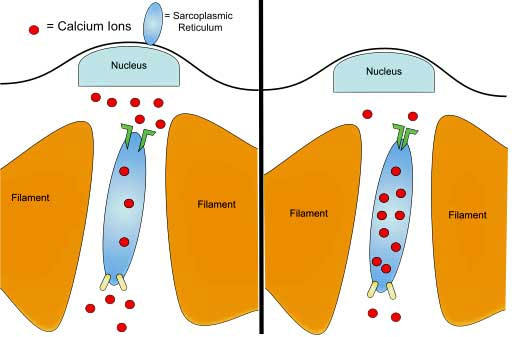
Among many other things, calcium ions also play a critical role in exercise
As with every ME/CFS/FM treatment responses to the drug are very variable. Some doctors have not had much success with it. Parker reported that Dr. Mason Brown found that https://www.actionforme.org.uk/assets/components/discuss/attachments/2/6193/nimodipine%20use%20in%20me,%20jan%202014.pdf “Nimodipine helps twenty percent of ME/CFS patients very quickly, another twenty per cent over six months, and all others to varying degrees over a period of time.” Dr. Shepard
https://www.meassociation.org.uk/2008/01/brief-notes-on-nimodipine-and-mecfs recommended that the drug be used with care and advises that anecdotal reports have been mixed.
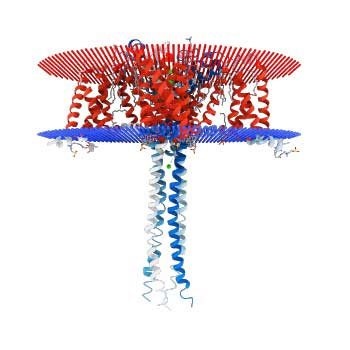
Crystalline structure of the N-type calcium channel believed involved in chronic pain
Susan Parker reports on the effects of other calcium channel blockers in ME/CFS and doctor’s experiences with Nimodipine and the various Nimodipine protocols used in ME/CFS here.
https://www.actionforme.org.uk/assets/components/discuss/attachments/2/6193/nimodipine%20use%20in%20me,%20jan%202014.pdf
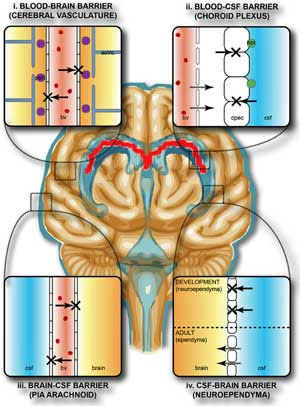
One of nimodipine’s advantages is its ability to cross the blood-brain barrier
Patient access to the drug is limited by practitioners who are reluctant to try it, and it’s cost – currently about $3-500/month in the U.S. right now. You can find some UK and U.S. doctors who’ve used Nimodipine to treat ME/CFS in Susan Parker’s overview
For a list of drug interactions and detailed protocol recommendations check out Susan Parker’s downloadable overview.
https://www.actionforme.org.uk/assets/components/discuss/attachments/2/6193/nimodipine%20use%20in%20me%20jan%202014.pdf
Resources
• Nimodipine use in M.E. / CFS: A comprehensive guide by Susan Parker https://www.actionforme.org.uk/assets/components/discuss/attachments/2/6193/nimodipine%20use%20in%20me,%20jan%202014.pdf – Free 34 page pdf
• The Nimodipine Way? A Review of “Beating Chronic Fatigue: Your Step-by-Step Guide to Complete Recovery”
https://www.healthrising.org/blog/2019/06/10/nimodipine-beating-chronic-fatigue-guide-downing-orr
• A Calcium Channel Blocker for ME/CFS and Fibromyalgia? Nimodipine Pt. II
https://www.healthrising.org/blog/2019/06/12/nimodipine-calcium-channel-blocker-fibromyalgia-chronic-fatigue-pt-ii
https://forums.phoenixrising.me/threads/no-pem-with-new-medication.48478 "When I started being sick, for the first year, I was crashing a lot, no matter how hard I tried not to. 21 days without a crash was my record. Then, in march 2016, I convinced my doctor to prescribe me Nimodipine Nimotop. I had bought a book about treating ME and had decided to follow this protocol that used Nimotop as it's main ingredient.”
I started with 7.5 mg once a day 1/4th of a pill, but could not tolerate it. I knew I had to manage the dosage myself according to side effects, so I decreased to 3.75 mg per day 1/8th of a pill. Then I was okay and from there I slowly increased my way up to 30 mg twice per day once in the morning, once in pm. Sometimes I had to decrease for a week then start going up again. I went as high as 45 mg twice a day, but my maintenance dose is 30 mg twice a day. This whole process took 2 months!
After 2 months, in May 2015, I stopped having crashes. I didn't realize it right away, because this is not the type of drug where you just wake up one day and feel like your life has miraculously changed... But I was recording everything in a journal, keeping stats and graphs, and in august, I realized I hadn't had one single crash for the whole summer!
Before taking Nimotop, I couldn't do any exercise without jeopardizing my health. I had stopped trying to go to the gym because it was making me crash. I had to stop working with my physical therapist, because no matter how much easier she made the program, I was still crashing. At the end of our work together, I was only doing stretches and still couldn't manage it. Walking was hard. When I took the dog for a walk, I had to sit down to rest every 15 minutes or so.
After Nimotop, I started going to the gym again. I had learned from all my crashes so I made up a nice program that was achievable and was able to stick to it 3 minutes of weight lifting over a period of 45 minutes. The weights are pretty heavy. Also, I was able to start biking again outside. At first I would only go for 20 minutes at a time, and my speed would stay around 12km/h. I went maybe 3 times a week. After a while, I could go for as long as 60 minutes, when I was having a good day. And my average speed increased to 18-20 km on those good days. That is quite an accomplishment compared to what I could do prior to Nimotop.
3 weeks ago I had a definite proof that Nimotop is what's making the difference. I had to stop it to take a stress echo, where I had to pedal lying down for less than 9 minutes. 24 hours later I had the first crash I had since Nimotop had started to work, in May 2016. It took me 10-12 days to go back to my baseline. I was depressed and scared, I was afraid I wouldn't go back to what I was. I started taking Nimotop as soon as I could and I slowly improved to my prior level. Gym is okay again.
I think people don't give enough credit to this drug. Most of those who try it want it to work really fast and they start off on high doses and get too many side effects and quit. I think if people took their time to slowly increase the dosage and tried it at least 3 months, they would have success more often. Sometimes it works on cognitive problems, also.
It's not a miracle drug and it doesn't solve all our problems. In fact, pretty much is the same with me, except for PEM. But removing PEM from this dreadful illness is already a precious gift"
Nimodipine is drug number 3 in Dr Jay Goldstein's Top 23 Drugs For ME/CFS Treatment.
Below are some snippets about nimodipine from Erica Verrillo's book Chronic Fatigue Syndrome: A Treatment Guide. Erica Verrillo has very kindly posted the first edition of her book online for anyone to read for free on her blog. I hope Erica does not mind me pasting a small snippet from this book below.
CALCIUM CHANNEL BLOCKERS
Nicardipene, Nimodipine, Nifedipine, Verapamil
DEFINITION. Calcium channel blockers inhibit the transmembrane influx of calcium ions into cardiac and smooth muscle.
BACKGROUND. Calcium channel blockers work by preventing calcium ions from entering smooth muscle cells. Calcium is especially important for the functioning of these cells and specialized cells in the heart. When calcium levels are lowered, the result is a relaxation of blood vessels, allowing an increased supply of blood and oxygen to the heart while decreasing its work load.
As a consequence of their effect on blood vessels, calcium channel blockers are useful in treating cardiovascular disorders, such as angina chest pain and coronary artery disease, and to lower blood pressure. These drugs also may improve exercise capacity and subsequently reduce the need for surgery in patients with cardiac problems.
USES IN CFIDS. At the 1990 CFIDS conference in Los Angeles, Dr. Ismael Mena presented evidence of cerebral dysfunction in patients with CFIDS. Using neurologic spectroscopic scanning techniques, Dr. Mena reported that 71% of CFIDS patients have low blood flow hypoperfusion in the temporal lobe of the brain. He further reported that after treatment with calcium channel blockers, some of these patients exhibited clinically improved cerebral blood flow CFIDS Chronicle, Spring/Summer 1990.
A number of CFIDS clinicians have noted improvement in cognitive function in patients given calcium channel blockers. Cardene also is helpful in treating migraine-type headaches. Dr. Jay Goldstein also observed improvements in cognitive function and energy level in patients given calcium channel blockers. He has also noted increased exercise tolerance, decreased tender point sensitivity, and alleviation of panic disorder with nimodipine.
In October 1994, Dr. Robert Keller, Medical Director of the Center for Special Immunology in Miami, reported improvement of symptoms in 25 patients with CFIDS after treatment with the calcium channel blocker verapamil. Within 1 month of finding the optimal dose of verapamil, patients reported improvement in fatigue, memory, and myalgia. Dr. Keller also reported a decrease in the number of activated T cells, demonstrating that calcium channel blockers may have some immunomodulatory properties.
The book also notes some of the side effects that ME/CFS patients may experience with Nimodipine and other calcium channel blocker drugs:
Although calcium channel blockers can be effective for some of the more problematic CFIDS symptoms cognitive dysfunction, side effects can be a problem. The most common are lowered blood pressure which can be serious if blood pressure is already low, severe pressure headaches, dizziness, gastrointestinal problems diarrhea, constipation, and weakness.
In addition, hypertensive effects can be exaggerated by concomitant use of other drugs that affect blood pressure, such as beta blockers. Tagamet cimetidine also increases the effects of calcium channel blockers. The use of calcium channel blockers requires close supervision by a physician.
Apparently nimodipine is unique among calcium channel blocker drugs in that it can cross the blood-brain barrier, and enter into the brain
"My calcium channel blocker side effect was brutal insomnia. I was on Lercanidipine. Every month or so I would sleep an hour less per night. At the end before I figured it out I was sleeping only minutes a day, and broken up at that. I had been in decline that entire time. The first night on new actually old, they cause neuropathy instead meds I slept more than I had in the entire previous week, then twelve hours the next night, and I have been improving ever since. This is a side effect they don't warn about"
![]()
The Nimopedine protocol Downing-Orr, Kristina. Beating Chronic Fatigue
Nimodipine a prescription drug aimed to boost brain circulation – also known as Nimotop
• Ginkgo biloba to promote peripheral circulation
• Eight glasses of filtered or bottled water per day to flush out toxins and improve circulation
• L-Glutamine to promote brain function and general wellbeing
• Evening primrose oil to promote brain function and reduce muscle symptoms Nimodipine
We kickstart the healing process by ‘rebooting’ the body. At the core of this programme is the view that the vital brain functions – those which govern our body’s health – are malfunctioning, leading to the bizarre array of symptoms that characterise CFS, as we have seen.
The prescription drug Nimodipine also known as Nimotop is the cornerstone of this treatment and is the starting point of this plan. Nimodipine is a calcium channel blocker, originally used with people who have had strokes. However, this protocol has been designed especially for CFS patients and the drug works in this context to eliminate brain toxins which have built up as part of the CFS disease process. Once these neurotoxins are reduced and then flushed out, your brain will function much better, because blood flow to the important gland master controls the HPA axis will increase. As a result, the healing mechanisms should then be switched back on, allowing your body to start to recover. You will need to purchase a pill cutter for the Nimodipine which comes in 30mg tablets. You can find one at any pharmacy. The dose required varies from person to person, but we all start with the same tiny amount: one quarter tablet. It is best to take Nimodipine with food in the beginning because this slows down the rate of absorption and you want the process to be slow, so as not to strain your body. Also, try to take it at the same times every day.
Week one Take one quarter tablet of Nimodipine in the morning and eight glasses of water per day. Do not be tempted to take more Nimodipine.
Week two Continue taking one quarter tablet in the morning, but increase the dose by taking another quarter in the afternoon preferably not after 4 p.m. as it can interfere with sleep. So you will now be taking a total of one half a tablet per day. Continue drinking the eight glasses of water and, as before, do not be tempted to increase the Nimodipine dose.
Week three Increase your morning dose of Nimodipine to a total of one half a tablet, but continue taking the one quarter in the afternoon, so that you are now taking three quarters of a tablet per day. As always, drink the water and don’t be tempted to increase the Nimodipine dose. This advice remains consistent throughout the whole programme.
Week four While still taking one half a Nimodipine tablet in the morning, now increase your afternoon dose to one half. You are now taking a total of one full Nimodipine tablet a day. As always, drink your water quota. Week five Increase your morning dose of Nimodipine to three quarters of a tablet, but your afternoon dose of one half remains the same. Use the above schedule as a guide: some people will need less Nimodipine, for example, a total of one tablet, while others might need more, say a total of two or even three tablets maximum four. However much Nimodipine you need – and how you will know this is explained in the box below – the instructions are the same: you start with just one quarter tablet and steadily and slowly build up. Note: in some cases, the starting dose of a quarter tablet might be too much, in which case it’s recommended either to begin with an eighth of a tablet or to take one quarter every two or three days.
Essential protocol instructions 1. Always remember to drink the eight glasses of water a day and make sure it’s bottled or filtered.
2. Do not increase the Nimodipine dosage more quickly than advised, no matter how impatient you are to progress. You must follow the protocol exactly as outlined. The key to the success of this treatment is its steadiness. Nimodipine flushes out neurotoxins and you don’t want to overwhelm your body with these all at once, as it might not be strong enough yet to process them effectively.
3. You must monitor how you feel. If you experience mild facial flushing, headaches or nausea at any point, you have taken too much Nimodipine. If so, just cut back on your dosage, a quarter of a tablet at a time, until those symptoms disappear, then use this as a starting point to build up the dose again slowly. If you experience these symptoms at the start of the programme, reduce the starting dosage to one eighth a tablet per day, slowly building up from there.
4. If you do take too much Nimodipine and experience severe facial flushing, for example, you can obtain another prescription drug from your doctor called Propranolol, which is a beta blocker. Dr Mason Brown recommends 40mg per episode to counteract any discomfort and the Nimodipine should also be reduced. This should not be needed if you follow the protocol exactly, but sometimes when people are too hasty and progress at a faster pace than is recommended, the minor symptoms of facial flushing, headache and nausea can become very uncomfortable. In such cases, the beta blockers should ease the symptoms.
5. Nimodipine is a temporary treatment. Some people only need it for a month or so, while others will need it for longer four or five months at most.
6. If you begin your weekly increase and experience facial flushing or headaches which are mild, but noticeable, don’t increase the dose for another week. Stay at the same dose for another week, then try again. If you continue to experience these symptoms, you will know that you have reached your maintenance dose and it’s time to start reducing.
7. As you progress with the Nimodipine, you should experience an increase in cognitive and emotional function and a decrease in symptoms, including migraines. In other words, you should notice an improvement in brain function. This is how you will know you are improving.
8. At some point, you will reach a maximum maintenance dose and require no further increase in Nimodipine. You will know you have reached this point when your brain and emotional functions have greatly improved and if, when trying to up your dose, you experience a slight headache different from the usual CFS migraine; in my experience, neither severe nor disabling, but more like a niggle, mild facial flushing or increased heartbeat. These are signs that the Nimodipine has done its job and you should remain at the previous week’s dosage.
9. At some point, this maintenance dose will itself cause the same telltale signs of taking too much. This is because your brain circulation is improving, the neurotoxins have been reduced and your body is healing. When this happens, begin reducing the dosage, by carefully reversing the protocol. So, say you have reached a dose of two tablets per day, you then reduce by taking one tablet in the morning, but three quarters of a tablet in the afternoon. Remain at this level until you again experience the indicators that it is time to reduce, and continue the process until you are no longer taking any Nimodipine.
10. Avoid grapefruit while taking Nimodipine as it interferes with the medication’s effectiveness and always check with your doctor about other medication interactions.
This protocol is really very easy to follow. The programme has been designed specifically for people who are at home. The amount of Nimodipine taken is very small and the build-up is very slow so as to ensure minimal reactions. Just monitor your progress and pay attention to how you feel. You can always adjust the dosage accordingly. You are now in charge of your recovery. Psychologically this is very important. CFS no longer controls you because you have the means to combat the illness. You can pace this treatment according to how you feel and this sense of empowerment should instill in you a sense of confidence. Julia For me, the symptoms were brain fog, brain fog, brain fog. I couldn’t remember anything at all. I was also severely depressed. I could get around and even worked in a part-time job, but I felt tearful all the time and the world just seemed like one big blur to me. I was taking antidepressants, but they just didn’t work for me, and that made me more depressed. When I started taking the Nimodipine, after a couple of weeks I started to think more clearly and I felt stronger emotionally. I remember thinking, ‘Ah, so this is how it feels when the antidepressants actually work’. The good news is, I was never depressed in the first place, it was all CFS. Most of my symptoms were brain related and one by one they all cleared up. Once the Nimodipine did its job, I didn’t even have to take antidepressants any more.
Ginkgo biloba at the same time as you take the Nimodipine, you can also begin taking the following supplements, starting with ginkgo biloba. Ginkgo biloba is a popular health-food supplement. It is thought to help increase peripheral circulation i.e. to the body’s extremities, such as hands and feet. Take one 400mg capsule of gingko biloba per day. This dosage level is safe; however, if you experience any bruising, which is a known but rare side effect, you must stop taking it.
L-Glutamine L-Glutamine is an amino acid that is an important source of energy for the brain. It also works to improve digestive tract function. Take one 500mg capsule three times a day for a month, after which you reduce to twice a day for one month. After that, a maintenance dose of one 500mg table t a day is advisable.
Evening primrose oil
Evening primrose oil helps brain and muscle symptoms because it contains a substance called gamma-linolenic acid GLA which helps to relieve symptoms of pain, particularly muscle aches. The recommended dose is one 500mg capsule four times a day.
Step Two: Promoting Good Gut Health This step runs concurrently with Step One. You will need: • Prime Directive probiotic powder to replenish good bacterial flora Probiotics At the same time as you improve brain and body circulation, you will also need to tend to your gastro-intestinal tract functioning and start taking the probiotic. As we have seen earlier, many healthcare professionals acknowledge – although controversial – that a healthy gut is vital to a healthy body and mind. Since many people with CFS experience yeast overgrowth also called dysbiosis, Candida, or bad bacteria and this unhealthy balance can help prevent the absorption of vitamins and minerals, your digestive system needs to be addressed.
This programme recommends a probiotic powder called Prime Directive see Resources, p. 198 for stock lists – it is an organic product and based on Dr Mason Brown’s experience is most effective, but others are available in capsule form. However, make sure you go for a good-quality probiotic capsule teeming with billions of micro-organisms. Probiotics aim to replenish your digestive tract’s supply of good bacteria and can also help improve symptoms of thrush, indigestion and irritable
For Prime Directive, the instructions are simple – you just mix the powder with water. You begin with a very small quantity, either one quarter or one half a teaspoon a day, either in the morning or last thing at night. It is very important that you begin with a small dose and build up to the recommended amount slowly and steadily. I cannot emphasise this point enough. By tending to your gastro-intestinal health in this manner, replenishing your stock of good bacteria, the bad bacteria will die off and be processed by the immune system. As a result of this immune-system interaction, you can expect to experience an increase in flu-like symptoms, such as tiredness, achiness, irritability and emotional upset. This is all normal, healthy and to be expected.
However, because your body is still likely to be weakened and more fragile than that of a well person, you do not want to overload your system. You will have to gauge your symptoms here too. So if you do feel more tired than usual or other flu-like symptoms arise, either reduce your dose of Prime Directive or lay off the probiotics altogether for a day or two. This will give your body a chance to process the bad bacterial waste and eliminate it from your body. Once you start to notice an improvement in the way you feel, you can resume the probiotics. Overall, you can expect to take Prime Directive for two to three months and then stop.
However, I continue to take a pro-biotic every day as part of my daily health regime. Once, however, you begin to feel an increase in energy and a decrease in the flu-like symptoms, this means your body is now beginning to absorb better the vitamins and minerals in your diet. The energy from these nourishing substances is now finally reaching your cells.
Foods to avoid Certain foods are known to encourage the growth of bad bacteria in our gut and should be eliminated from your diet. They probably include many of your favourite foods but, to paraphrase an aphorism from a well-known dieting organisation – nothing tastes as good as energy feels:
• White flour
• White rice
• Sugar
• Honey and syrups
• Stock cubes
• Yeast extracts, such as Marmite
• Soy sauce
• Smoked meats and fish
• Pickles and relishes
• Peanuts
• Mushrooms
• Any food containing vinegar, such as mayonnaise
• Chilli and curries
• Citrus fruits, particularly oranges, lemons and grapefruits
• Dried fruit
• Cheese
• Tinned foods and tinned juices
Foods to include in your diet Once you have achieved good gut health, you want to ensure that the foods you choose also encourage the growth of good bacterial flora by providing the right environment for them to flourish. Here is a list of foods you should consider adding to your diet:
• Fresh vegetables and salad organic
• Avocados
• Seeds e.g. sunflower, pumpkin and flax
• Mild spices and herbs e.g. oregano, basil, nutmeg, cinnamon
• Herb teas and Rooibosch
• Cottage cheese
• Natural yoghurt from goat’s or sheep’s milk
• Rice cakes
• Soya and rice milk Fish all kinds
• Extra-virgin olive oil
• Artichokes
• Asparagus
• Bananas
• Buttermilk
• Endive
• Garlic
• Leeks
• Onions
• Shallots Tempeh a fermented soya-bean product For more information on improving your digestive health, I recommend two excellent books: Good Gut Healing by Kathryn Marsden Piatkus and The Beating Fatigue Handbook by Erica White Thorsons.
Step Three: Detoxifying the Body You will need:
• Revenol an antioxidant
• Milk thistle to boost liver function
Once you have seen signs of improvement from the earlier two steps, and you are comfortable with moving on, it is time to begin Step Three which aims to detoxify the body. I would recommend that you wait around a month before you begin the detoxification process. As you progress through Steps One and Two, always monitor how you feel. Once your neurotoxins have decreased, leading to improved cognitive function and your digestive tract has improved, leading to an increase in the absorption of minerals and vitamins, you should have reached a point where your body is feeling stronger.
Throughout this process, always ask yourself how you are feeling. You and you alone, can monitor your body’s response to each phase, so that you can tailor the programme according to your individual needs. This is not difficult, but it is essential, because only you can determine the rate of your own recovery. This is because, as we’ve seen, CFS is not a one-size-fits-all illness. Your body will have been exposed to two types of toxins: internal from cellular waste products and external pollutants, food additives and chemicals. Because your body has been malfunctioning, it has not been able to process these toxins efficiently, resulting in a build-up which we now need to address.
Revenol available at Neways – see Resources, p. 193 – and via the internet is recommended for detoxification. Although there are other antioxidants on the market, I would always use this one for our purpose here. It is a capsule combining vitamin C, beta-carotene, and maritime pine bark. Despite its nutrient-enriched content, Revenol is a powerful detoxifying agent. Detoxification should be undertaken very, very slowly because, again, the immune system will be responsible for processing these toxins. Also, you don’t want to overload your body with excessive toxins, as this will put strain on your liver.
This is why before you even begin considering detoxing your cells, you should wait until the ‘die-off’ reaction see p. 111 from your digestive tract has subsided substantially because you can, again, feel a sharp increase in flu-like symptoms, especially tiredness, when you are detoxifying. Some people only experience a mild increase in symptoms, while for others myself included this is more severe. Again, this is a healthy sign that your body is healing normally, but given the symptoms that are likely to occur, you should never push through the detoxification process. Slow, careful pacing is required. As in the case of the Nimodipine, the starting dose of Revenol is very low. Unlike Nimodipine, however, you will not have to wait a week before increasing the dose. You can base your decision on how you feel. You will need your pill cutter again. Begin with a quarter of a tablet. If you feel well, then increase the dose to one half a tablet the next day. You can continue in this way until you reach the product’s recommended daily amount. If, at any time, you feel an excessive degree of tiredness or flu-like symptoms, then just stop taking the Revenol for a day or two, resuming when you feel better. Alternatively, you can space out the dosage, so that you take it one day, then have a day or two off.
As Revenol is not a prescription drug, but is, in fact, a health supplement, you can continue taking it for as long as you want or need to, depending upon the detoxification process. You will know that the detoxification has finished, because once all the toxins have been removed, your immune system is no longer activated in response. Any symptoms that you will have experienced such as tiredness, achiness and irritability will have disappeared as a result. Revenol has done its job once your body is functioning more fully and the nutrients from your diet are able to reach your cells – you can then expect to feel more energy, more vitality and greater wellness than you would ever have imagined. For some, who have few built-up toxins, the process will be short. For others, it can be longer. I took Revenol for an entire year before I noticed any real improvement in my symptoms at all. This is because I had an extremely high concentration of toxins in my body.
However, I can assure you, it was worth every moment because I have regained my health. And I would do it all over again. Always remember to take Revenol after a meal, otherwise you might experience an upset stomach, due to the high concentration of vitamin C. Milk thistle While you are detoxifying you must also take a product called milk thistle, which contains a substance called silymarin. It is a popular supplement which can be obtained at any health-food shop and it is known to have liver-supporting properties. Your liver is your body’s filter and, as such, is responsible for cleaning out toxins, so while you are undergoing a process of detoxification meaning that more toxins will be pumped into your system, your liver will need more support than ever. Follow the recommended dose on the milk thistle bottle. You can continue taking it even after the detoxification process is complete i.e. when you are no longer experiencing flu-like symptoms and instead feel an increase in energy or you can choose to stop taking it once you no longer need Revenol.
Step Four: Replenishing Your Body You will need:
• A high-quality multivitamin supplement to support your body’s need for replenishment during the recovery
As you progress through Stages One to Three, your body will be working very hard to clear out the ‘sludge’ in your brain, gastro-intestinal tract and in your cells. Once these obstacles are removed, your body should now be in a more receptive state to accept all the health nutrients from your food. Because it has been effectively deprived of these nutrients not necessarily because your diet has been poor, but because of all the obstacles to smooth functioning, your body will benefit from some additional support in the form of certain vitamins and minerals. I would recommend a good multivitamin tablet the Solgar and BioCare ranges are particularly good. Look for one that contains vitamins C, B-complex and E, as well as calcium, magnesium, zinc and selenium, and follow the recommended dosage on the bottle. You can continue taking the multivitamin as part of your daily dietary requirement or stop altogether when you feel well. Of course, I would also recommend that you eat a healthy diet see Chapter Seven or consult a nutritionist. The Recovery Process As your body begins the healing process, you must rest in order to recuperate and recover. After a time, you should begin seeing the signs of healing. Your immune system will continue to remain activated, clearing out the sludge of toxins and dealing with any lingering viral infections which have placed added strain on your formerly beleaguered body. The process can take a while.
The rule of thumb is this: if you have had CFS for up to five years, then expect to take a year to recover or at least improve your quality of life dramatically. If you have been suffering the ill effects of the condition for longer, anticipate a two-year recovery period. Your body has been through the wringer with a serious illness, so patience, perseverance and pacing are required. Along the way, you should see evidence of major improvements, and with every new milestone – no matter how small in the beginning – you should feel victorious. Then, one day, after your newly healthy body has cleared the paths of toxins, the viruses have been sorted out and the flow of energy is now reaching your cells, thanks to a healthy gut and circulatory system, you should wake up with more vitality than you ever dreamed possible.
Think of recovery in stages as a progression: you start by embarking on the programme, then you notice improvements in your physical health; you then move on to the process of fitness and rehabilitation and, ultimately, you regain full health and re-engage with life as a healthy person. Use the chart overleaf to monitor your progress throughout the recovery process. Rate your progress on a scale from one to 100 where 0 = your worst symptoms and 100 = maximum health. Don’t be alarmed if progress is slow; always remember that you are recovering from a serious illness and this is bound to take time.
DAY 1 DAY 2 DAY 3 DAY 4 DAY 5 DAY 6 DAY 7 How am I feeling today generally? What are my cognitive symptoms? What are my emotions? What are my physical symptoms? In Conclusion We would all like to bounce back as soon as possible, but your body can only heal itself at its own rate. During this time of recovery, you can expect to see small improvements along the way. Even the tiny achievements – making tea, going for a walk, sitting down in a restaurant or going out with friends – will take on new significance and be joyous events. So, remember:
1. Be patient.
2. Try not to worry or stress about your recovery time. It won’t make your healing time any faster; in fact, psychological distress can delay the process.
3. Accept that you need time. Allow yourself to lie back, rest and heal. For right now, this is your job.
4. Always monitor your symptoms and pace yourself accordingly.
5. Always keep your doctor in the loop.
6. Use the mantra, ‘Things must get worse before they can get better’. If you have flu-like symptoms it means your body is in the process of eliminating toxins and healing.
Nutritional protocol
Although the medical approach in the previous chapter is highly effective as the first step to strengthening the body, it’s not for everyone. Some people feel that the independent nature of the programme is too demanding or they shy away from having to take and monitor prescription medication. If you fit into this category, there is another option for you – the nutritional method. You will still have to monitor your reactions and will still experience a die-off reaction see p. 111, but this purely nutritional approach is a highly effective treatment for CFS. Although I did not use this programme when I had CFS, mainly because I was not aware of it then, I can, however, recommend the two professionals who devised it. Alessandro Ferretti Alex and Jules Cattell are two highly qualified nutritionists who work in partnership and I have enormous respect for them. Through their understanding of the causes and nature of CFS they have designed an easy-to-follow programme, which you can undertake at home. Although they would recommend that you work with a nutritionist for support and to boost your chances of success, it is not absolutely necessary. For more information about Alex and Jules, see Resources p. 193. The aim of this approach, which chimes in with the philosophy of the renowned American CFS medical expert, Dr Jacob Teitelbaum see p. 54, is to nourish and heal the body through good food, dietary improvements and vitamin and mineral supplementation. There is also a strong overlap between this approach and Dr Mason Brown’s method. As always, consult your doctor before making any changes to your diet or health regime. The Goal of the Nutritional Method The nutritional model has been designed to reboot your body by building up and improving your:
• Immune system
• Gastro-intestinal function
• Circulation
• Adrenal function
• Cell mitochonsdria
• Liver function.
General Dietary Advice We’ll begin by making improvements to your food and diet. It might be a hackneyed expression, but when it comes to CFS, we really are what we eat. Food, diet and nutrition are the cornerstones of health and wellbeing, so it should come as no surprise to you that their role is essential in your recovery. Many people with CFS have food imbalances, mainly blood-sugar dysregulation. 1 Their diets are often too low in protein and too high in carbohydrates, leading to a dysregulation of blood-sugar levels. It has been observed elsewhere that many people with CFS have problems with their blood-sugar levels. When we refer to blood sugar, we mean energy. So if your blood sugar is too low, you can experience many of the same symptoms associated with CFS – fatigue, weakness, headaches, emotional disturbances, dizziness, fainting although just because you experience low blood sugar does not automatically mean you have CFS.
Conversely, if you experience consistently very high levels of sugar in the blood, it could lead to the development of chronic conditions, such as diabetes, or throw your energy levels into a tailspin. So the aim here is to eat foods which carefully regulate your blood sugar and keep it well balanced. These should be foods that either release sugar slowly into your bloodstream or those which contain no sugar at all. Blood-sugar levels often become dysregulated because of your diet. If you are experiencing low blood-sugar symptoms, for example, you might be tempted to turn to sweetened foods or caffeine, leading to a sharp rise in sugar levels in your system. This burst will quickly be followed by a crash, resulting once again in low blood sugar and its corresponding symptoms. The temptation is then to turn to the quick-fix foods such as cakes, biscuits, caffeine, leading to a neverending cycle of boom and bust. Regulating your blood sugar will mean that more energised. To improve your health and vitality, it is recommended that you adopt a ‘hunter-gatherer’ approach to food. Use the following guidelines which will keep your blood sugar on an even keel, and set you up for life:
• Lean protein at every meal chicken, game, fish – especially oily varieties, some organic red meat, eggs, tofu/ tempeh, fresh nuts and seeds.
• Few or no grains wheat, oats, rye – they can stress the intestinal tract.
• Plenty of green vegetables/ salad.
• Water, Rooibosch and herbal teas to replace caffeinated tea, coffee, fizzy drinks and alcohol.
• Aim for a ratio of one third protein to two thirds carbohydrates at every meal and for each snack. You don’t have to be obsessive in terms of measuring out exact portions. It is roughly one handful of meat to two handfuls of vegetables.
Other good food guidelines Here are some other tips to help regulate blood-sugar levels and give you more energy:
• Cut out all alcohol.
• Avoid drinks containing caffeine, such as tea, coffee, cola.
• Eliminate refined grains, such as cornflour, white rice, and white flour because they release sugar into the bloodstream very quickly.
• Avoid foods with chemicals, additives or preservatives.
• Stay away from foods containing sugar including honey and malt.
• Aim to eat five small meals a day, rather than three large ones.
• Always have breakfast.
• Learn to cope with stress see Chapter Ten, as people often turn to comfort eating and choose refined carbohydrates for an emotional boost.
• Eat whole grains – whole brown rice, maize meal and wholewheat pasta.
Essential Protocol Instructions
As with the medical model, the nutritional option specifies a special cocktail of essential vitamins and minerals to reboot your body into action. If you have been ill with CFS for some time, your body will likely have been denied the nutrients it needs for healthy functioning. While the ‘hunter-gatherer’ approach to food is the first step to a nutritious lifestyle, you will also need to boost your system with dietary supplements. Some of the supplements used here are the same as those recommended in the last chapter; others are different. You can carry on taking the supplements indefinitely at the recommended dosage, once your body has stabilised or you can stop altogether when you feel better. Before I detail the specific CFS formula, there are eight key points you will need to remember:
1. For moderate sufferers In general, always begin with the lowest dose possible for each product, unless otherwise specified below. The goal is to build up slowly to the full dose, depending on how you feel. I would introduce supplementation step-by-step.
2. So on Day One, take all the supplements in Step One, on Day Two, add the additional supplements for Step Two, Day Three add the recommended supplementation for Step Three and so on. Keep going until you are taking all the supplements. You might want to spread out the process throughout the day; for example, taking half the supplements in the morning and the other half in the afternoon. Should you feel overwhelmed at any point, just cut back on the dosage or adopt a day-on, day-off policy.
2. For severe sufferers CFS can leave your body in a severely weakened state. If you are particularly fragile or frail, it is recommended that you introduce supplementation
back to top
back to top
back to top
back to top
back to top
back to top
back to top
back to top
back to top
back to top
back to top
back to top












