click again to close
click again to close
Skill Level 5
Relevance:5 Technical Level:3
Page Synopsis: Neurorestoration is possible but it takes a positive attitude to endeavor the work
page 51 PTBICF > COGNITION HEALING from STROKE (also helpful with TBI
page 50
page 52

Full report please visit https://bra.in/6pWbDY
There are many promising therapies including:
1) diet ('Mum, 82, who couldn't recognise her own son due to dementia gets memory back - after changing her diet)
2) HBOT
Click for fifteen HBOT links 2) Effect of hyperbaric oxygen therapy on chronic neurocognitive deficits of post-traumatic brain injury patients: retrospective analysis https://bmjopen.bmj.com/content/8/9/e023387 3) The Complete Guide to Hyperbaric Oxygen Therapyhttps://elanaspantry.com/the-complete-guide-to-hyperbaric-oxygen-therapy/?fbclid=IwAR1HSk7Y_JJm-nkkUp4eXsQzgDPZC4RsxVHuZyHNbVLN7dVTjsTd7jl7_zE 4) Can Hyperbaric Oxygen Repair the Damaged Brain?https://www.dana.org/article/can-hyperbaric-oxygen-repair-the-damaged-brain/?fbclid=IwAR3sFgscF2wkuHUqyfNm8L-8eE13NOYtiia6SkGpgCCjn3XoJGrWsWIDJNY 5) Forever young – We can reverse aging with HBOThttps://www.aha-hyperbarics.com/blog/2020/11/27/forever-young-we-can-reverse-aging-with-hbot 6) Effect of hyperbaric oxygen therapy on chronic neurocognitive deficits of post-traumatic brain injury patients: retrospective analysis https://bmjopen.bmj.com/content/8/9/e023387 7) The Complete Guide to Hyperbaric Oxygen Therapyhttps://elanaspantry.com/the-complete-guide-to-hyperbaric-oxygen-therapy 8) Can Hyperbaric Oxygen Repair the Damaged Brain?https://www.dana.org/article/can-hyperbaric-oxygen-repair-the-damaged-brain 9) A BREAKTHROUGH OXYGEN THERAPY MAY BE ABLE TO REVERSE BRAIN DAMAGEhttps://futurism.com/neoscope/a-breakthrough-oxygen-therapy-may-be-able-to-reverse-brain-damage 10) Study Reveals Oxygen-Rich Air Can Reverse Severe Brain Damagehttps://nocamels.com/2013/02/study-reveals-oxygen-rich-air-can-reverse-severe-brain-damage 11) Long-term daily mHBOT and full recoveries w/ ongoing maintenancehttps://forums.phoenixrising.me/threads/long-term-daily-mhbot-and-full-recoveries-w-ongoing-maintenance.54006 12) Israeli scientists claim they’ve partially REVERSED cellular aging process for 1st time in historyhttps://www.rt.com/news/507255-scientists-reverse-cellular-aging 13) Hyperbaric oxygen treatment: Clinical trial reverses two biological processes associated with aging in human cellshttps://www.sciencedaily.com/releases/2020/11/201120150728.htm Hyperbaric oxygen therapy (HBOT) https://www.drmyhill.co.uk/wiki/Hyperbaric_oxygen_therapy_(HBOT)Long-Term Hyperbaric Oxygen Treatment Induces Significant Remyelination and a Recovery of Sensorimotor Functionhttps://journals.plos.org/plosone/article?id=10.1371%2Fjournal.pone.0097750
About HBOT (click to open)https://elanaspantry.com/the-complete-guide-to-hyperbaric-oxygen-therapy/?fbclid=IwAR1CH7aRUeifoW2IRAC71CPINQxnEA8v4K5oqI_Ebk4xuCfUUh-hTJP75Zc https://www.dana.org/article/can-hyperbaric-oxygen-repair-the-damaged-brain/?fbclid=IwAR2mbxZBXijWR0px687OM1MWB93Ur6_P5HrA41LXM5Vy-tVFYqhI1IN-EG8 https://hbot.com/chronic-fatigue-syndrome-directions-for-immunotherapy/?fbclid=IwAR2-EJtpn2WCrlchgKM5jONt35W8FVtzbxkQ3OBMmIJNOyU_FOF20Cd2DMM https://www.oxyhealth.com/solace-210.html?fbclid=IwAR33AtBkMZ3W5EWhdVm7jspoPqk-8MJmuo2CSLA1tzFwGQg7x3Va4eAL3H8 https://bmjopen.bmj.com/content/8/9/e023387?fbclid=IwAR0-6URrF88WHTgD6X4nupwXSCDCmlJmmtLCroRm_6_tDG0Fua2aZAob7zE https://www.rt.com/news/525059-researchers-reverse-biological-aging/?fbclid=IwAR3Iy-eY_3UWgnhRiMuD-SrOSQBc9CwH6qW0HFg665yFAgg8mBYdjFrl6yY https://www.rt.com/news/507255-scientists-reverse-cellular-aging/?fbclid=IwAR3wwM_OouF9qa3KouLTKWOdtMOA_2Kqwb6k-JbodbZh1UPsw1Ze375CTYE https://www.drmyhill.co.uk/wiki/Hyperbaric_oxygen_therapy_(HBOT)?fbclid=IwAR2WrQsP2CeDE6asxB6yUvHmeyIlpc6slZkIDLOWYcvzgoacCkHdvPCz6mQ https://forums.phoenixrising.me/threads/long-term-daily-mhbot-and-full-recoveries-w-ongoing-maintenance.54006/?fbclid=IwAR1WVyBXh_raJDGpvi9mstlpO78AsTSQAI-0initUBkoYV0Jmzqm4Kw1hGo https://tbitherapy.com/hbot-for-brain-injury/?gclid=Cj0KCQjwlMXMBRC1ARIsAKKGuwjTMyESjGwm4b-LxFptXrkZZiLLISmCwkVd8jGA1tJxRBtk0BHUWh0aAuXIEALw_wcB&fbclid=IwAR0-6URrF88WHTgD6X4nupwXSCDCmlJmmtLCroRm_6_tDG0Fua2aZAob7zE https://www.brainline.org/article/hbot-way-heal-injured-brain?fbclid=IwAR0a_XUTW8c3d_l5jqmD803voPHjcC4WO6PD_HL2h92qe-AVRNrQsnmDCnA https://journals.plos.org/plosone/article?id=10.1371%2Fjournal.pone.0097750&fbclid=IwAR33AtBkMZ3W5EWhdVm7jspoPqk-8MJmuo2CSLA1tzFwGQg7x3Va4eAL3H8 https://forums.phoenixrising.me/threads/long-term-daily-mhbot-and-full-recoveries-w-ongoing-maintenance.54006/page-19?fbclid=IwAR1WVyBXh_raJDGpvi9mstlpO78AsTSQAI-0initUBkoYV0Jmzqm4Kw1hGo#post-2302526 https://forums.phoenixrising.me/threads/hard-hbot-therapy.81604/?fbclid=IwAR1NeM50NNdmT_Znr7JL6gloaqROw3gFLBGEop7ksOODAPU-zwYM1g2jNRY#post-2301644 6) Clinicshttps://newtownehyperbarics.com/?gclid=Cj0KCQiAkZKNBhDiARIsAPsk0WhQ7yqUO4RJjDrssm6G1HdoJhn5SF7WYtoy0sjbZ0c-VM8anpH9K9oaAnAnEALw_wcB https://www.oxyhealth.com/hyperbaric-chamber-rental-rfi5.html https://hyperbaricoxygentherapy.com https://www.hh-bayarea.com https://www.hyperbaricmedicalsolutions.com/blog/how-much-does-hyperbaric-oxygen-therapy-cost https://www.google.com/search?client=firefox-b-1-m&sxsrf=AOaemvJFowkFG-eWYkr1Rj3Keyl6gJm2EQ:1638223599549&q=Bay+Area+Hyperbarics+Los+Altos,+CA&ludocid=3144528847996958346&gsas=1&client=firefox-b-1-m&lsig=AB86z5VZedmDQSjO1HBuUCZFbmEE&sa=X&ved=2ahUKEwiOt9q9yr70AhVDFjQIHRS9BSoQvS56BAgBEAo https://www.google.com/search?client=firefox-b-1-m&sxsrf=AOaemvJFowkFG-eWYkr1Rj3Keyl6gJm2EQ:1638223599549&q=Advanced+Hyperbaric+Recovery+of+Marin,+Hyperbaric+Oxygen+Therapy+of+Marin+San+Rafael,+CA&ludocid=17274388007662961491&gsas=1&client=firefox-b-1-m&lsig=AB86z5X2Lp8li3uFd2aeckdfjf10&phdesc=wqENvz4nDs4&sa=X&ved=2ahUKEwiOt9q9yr70AhVDFjQIHRS9BSoQvS56BAgBEAc https://www.bayareahyperbarics.com/ https://www.google.com/search?q=class%202%20hbot&ie=utf-8&oe=utf-8&client=firefox-b-1-m https://www.oxygenhealthsystems.com/product/hyperbaric-oxygen-soft-chamber-36?gclid=Cj0KCQiAkZKNBhDiARIsAPsk0Wg-7RPtXw-PtlZUob5kR7FXDrGK2EztBxPKVgrdB9lN8Nj2EKvXInoaAj2aEALw_wcB https://hyperbaricoxygentherapy.com/faq https://oxfordrecoverycenter.com/hard-vs-soft-chambers-hyperbaric-oxygen-therapy-chambers
3) Nootropics
Note: there is too much info to place on this site, link goes to full report. Click for list of site topics
![]()
![]()
![]()
![]()
![]() <>xclick here to close and return to reportclick for full size, click 'x' button to close
<>xclick here to close and return to reportclick for full size, click 'x' button to close
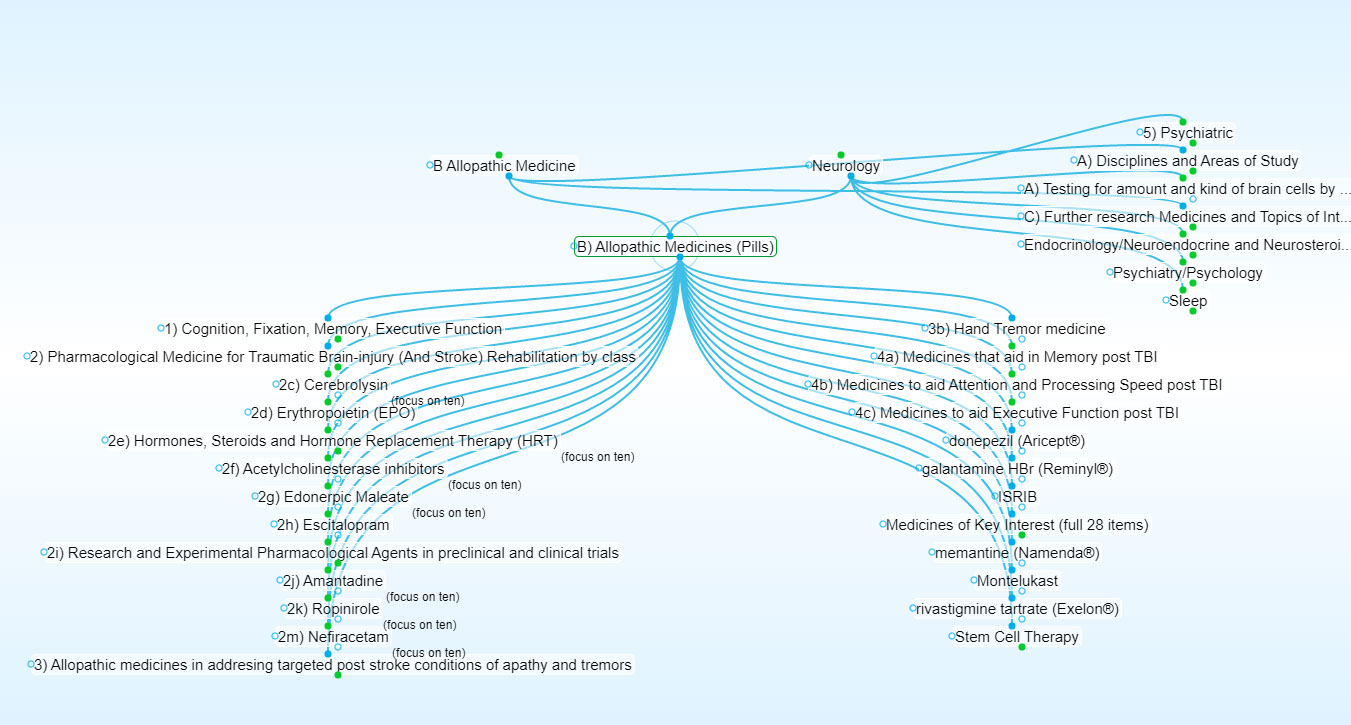
Please visit https://bra.in/5p7mJJ** for details, including medicines not listed on this site such as Escitalopram
Focus on medicine as text, not well formated below, go https://bra.in/5p7mJJ for full
5c) Further research
Further research
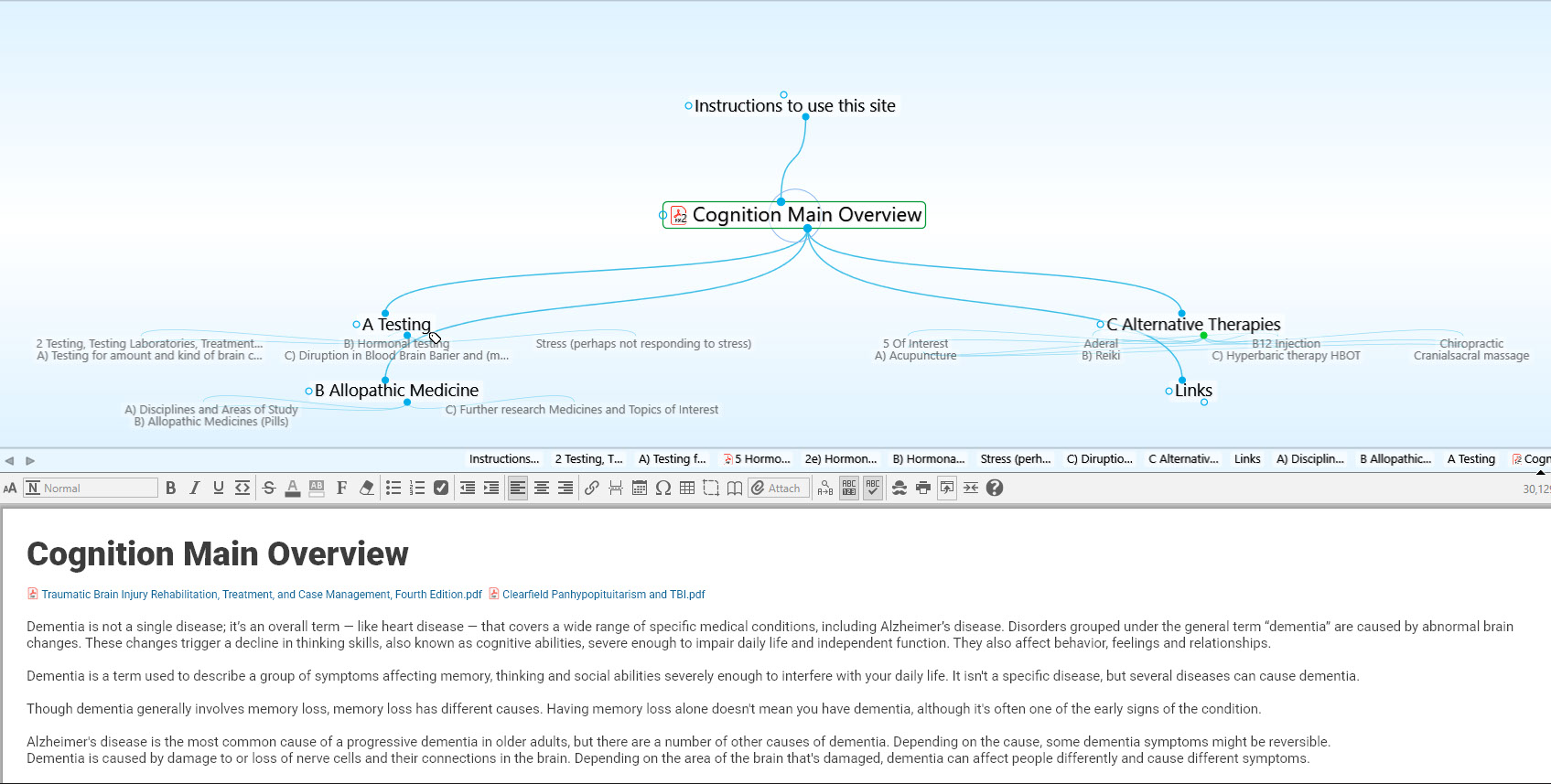
Dementia is not a single disease; it’s an overall term — like heart disease — that covers a wide range of specific medical conditions, including Alzheimer’s disease. Disorders grouped under the general term “dementia” are caused by abnormal brain changes. These changes trigger a decline in thinking skills, also known as cognitive abilities, severe enough to impair daily life andv independent function. They also affect behavior, feelings and relationships.
Dementia is a term used to describe a group of symptoms affecting memory, thinking and social abilities severely enough to interfere with your daily life. It isn't a specific disease, but several diseases can cause dementia.
Though dementia generally involves memory loss, memory loss has different causes. Having memory loss alone doesn't mean you have dementia, although it's often one of the early signs of the condition.
Alzheimer's disease is the most common cause of a progressive dementia in older adults, but there are a number of other causes of dementia. Depending on the cause, some dementia symptoms might be reversible.
Dementia is caused by damage to or loss of nerve cells and their connections in the brain. Depending on the area of the brain that's damaged, dementia can affect people differently and cause different symptoms.
Dementias are often grouped by what they have in common, such as the protein or proteins deposited in the brain or the part of the brain that's affected. Some diseases look like dementias, such as those caused by a reaction to medications or vitamin deficiencies, and they might improve with treatment.
Progressive dementias
Types of dementias that progress and aren't reversible include:
Alzheimer's disease. This is the most common cause of dementia.
Although not all causes of Alzheimer's disease are known, experts do know that a small percentage are related to mutations of three genes, which can be passed down from parent to child. While several genes are probably involved in Alzheimer's disease, one important gene that increases risk is apolipoprotein E4 (APOE).
Alzheimer's disease patients have plaques and tangles in their brains. Plaques are clumps of a protein called beta-amyloid, and tangles are fibrous tangles made up of tau protein. It's thought that these clumps damage healthy neurons and the fibers connecting them.
Vascular dementia. This type of dementia is caused by damage to the vessels that supply blood to your brain. Blood vessel problems can cause strokes or affect the brain in other ways, such as by damaging the fibers in the white matter of the brain.
The most common signs of vascular dementia include difficulties with problem-solving, slowed thinking, and loss of focus and organization. These tend to be more noticeable than memory loss.
Lewy body dementia. Lewy bodies are abnormal balloonlike clumps of protein that have been found in the brains of people with Lewy body dementia, Alzheimer's disease and Parkinson's disease. This is one of the more common types of progressive dementia.
Common signs and symptoms include acting out one's dreams in sleep, seeing things that aren't there (visual hallucinations), and problems with focus and attention. Other signs include uncoordinated or slow movement, tremors, and rigidity (parkinsonism).
Frontotemporal dementia. This is a group of diseases characterized by the breakdown of nerve cells and their connections in the frontal and temporal lobes of the brain. These are the areas generally associated with personality, behavior and language. Common symptoms affect behavior, personality, thinking, judgment, and language and movement.
Mixed dementia. Autopsy studies of the brains of people 80 and older who had dementia indicate that many had a combination of several causes, such as Alzheimer's disease, vascular dementia and Lewy body dementia. Studies are ongoing to determine how having mixed dementia affects symptoms and treatments.
Other disorders linked to dementia
Huntington's disease. Caused by a genetic mutation, this disease causes certain nerve cells in your brain and spinal cord to waste away. Signs and symptoms, including a severe decline in thinking (cognitive) skills, usually appear around age 30 or 40.
Traumatic brain injury (TBI). This condition is most often caused by repetitive head trauma. Boxers, football players or soldiers might develop TBI.
Depending on the part of the brain that's injured, this condition can cause dementia signs and symptoms such as depression, explosiveness, memory loss and impaired speech. TBI may also cause parkinsonism. Symptoms might not appear until years after the trauma.
Creutzfeldt-Jakob disease. This rare brain disorder usually occurs in people without known risk factors. This condition might be due to deposits of infectious proteins called prions. Signs and symptoms of this fatal condition usually appear after age 60.
Creutzfeldt-Jakob disease usually has no known cause but can be inherited. It may also be caused by exposure to diseased brain or nervous system tissue, such as from a cornea transplant.
Parkinson's disease. Many people with Parkinson's disease eventually develop dementia symptoms (Parkinson's disease dementia).
Dementia-like conditions that can be reversed
Some causes of dementia or dementia-like symptoms can be reversed with treatment. They include:
Infections and immune disorders. Dementia-like symptoms can result from fever or other side effects of your body's attempt to fight off an infection. Multiple sclerosis and other conditions caused by the body's immune system attacking nerve cells also can cause dementia.
Metabolic problems and endocrine abnormalities. People with thyroid problems, low blood sugar (hypoglycemia), too little or too much sodium or calcium, or problems absorbing vitamin B-12 can develop dementia-like symptoms or other personality changes.
Nutritional deficiencies. Not drinking enough liquids (dehydration); not getting enough thiamin (vitamin B-1), which is common in people with chronic alcoholism; and not getting enough vitamins B-6 and B-12 in your diet can cause dementia-like symptoms. Copper and vitamin E deficiencies also can cause dementia symptoms.
Medication side effects. Side effects of medications, a reaction to a medication or an interaction of several medications can cause dementia-like symptoms.
Subdural hematomas. Bleeding between the surface of the brain and the covering over the brain, which is common in the elderly after a fall, can cause symptoms similar to those of dementia.
Brain tumors. Rarely, dementia can result from damage caused by a brain tumor.
Normal-pressure hydrocephalus. This condition, which is caused by enlarged ventricles in the brain, can result in walking problems, urinary difficulty and memory loss.
Alzheimer's disease accounts for 60-80% of cases. Vascular dementia, which occurs because of microscopic bleeding and blood vessel blockage in the brain, is the second most common cause of dementia. Those who experience the brain changes of multiple types of dementia simultaneously have mixed dementia. There are many other conditions that can cause symptoms of dementia, including some that are reversible, such as thyroid problems and vitamin deficiencies.
Dementia is often incorrectly referred to as "senility" or "senile dementia," which reflects the formerly widespread but incorrect belief that serious mental decline is a normal part of aging.
Cognitive impairment can arise from virtually any poorly controlled chronic disease of the brain or the body’s organs, including hypertension, high cholesterol, heart disease, stroke, peripheral vascular disease, hypothyroidism, diabetes, chronic obstructive lung disease, kidney disease, infections, severe pain syndromes, obesity, sleep apnea, depression, anxiety, bipolar disorder, obsessive compulsive disorder, attention deficit disorder, multiple sclerosis, epilepsy, and alcohol, sedative, opiate or other chemical dependency. Single or repeated head injuries can impair cognition. Certain medications that get into the brain can impair cognition, such as tranquilizers, anticonvulsants, antipsychotics, older antidepressants, pain medications, and older bladder incontinence medications. Most of these conditions are treatable, particularly when memory cognitive disorders are detected early through annual monitoring of cognition after age 50 years old.
The degenerative brain disorders account for less than 50% of all people with memory cognitive disorders in primary care medical settings. These include Alzheimer’s Disease (AD), Parkinson’s Disease, Lewy Body Disease, Frontal Temporal Lobe Disease, and prion disease.
Recent studies show that although Alzheimer’s disease is not curable, it can be effectively treated to largely preserve independence and eliminate institutionalization in most individuals. In 2008, Atri Ali and colleagues at the Massachusetts General Hospital Memory Disorders Unit reported in the journal, AD and Associated Disorders, one of the most well analyzed longitudinal studies of Alzheimer’s disease. Patients treated for up to four years with the combination of Namenda and a cholinesterase inhibitor (Aricept, Exelon or Razadyne) delayed the functional rates of decline during the MCI stage by 33%, and during the dementia stage by 50-60%. This means that over the 14-year course of the MCI and dementia stages of AD, early detection, accurate diagnosis and combined therapy with Namenda and a cholinesterase inhibitor can delay the functional decline in AD patients by an average of 5-6 years. Since AD individuals spend an average of 4 years in institutions, the proper current approach can largely eliminate institutionalization.
Diet and exercise. Research shows that lack of exercise increases the risk of dementia. And while no specific diet is known to reduce dementia risk, research indicates a greater incidence of dementia in people who eat an unhealthy diet compared with those who follow a Mediterranean-style diet rich in produce, whole grains, nuts and seeds.
Excessive alcohol use. Drinking large amounts of alcohol has long been known to cause brain changes. Several large studies and reviews found that alcohol use disorders were linked to an increased risk of dementia, particularly early-onset dementia.
Cardiovascular risk factors. These include high blood pressure (hypertension), high cholesterol, buildup of fats in your artery walls (atherosclerosis) and obesity.
Depression. Although not yet well-understood, late-life depression might indicate the development of dementia.
Diabetes. Having diabetes may increase your risk of dementia, especially if it's poorly controlled.
Smoking. Smoking might increase your risk of developing dementia and blood vessel diseases.
Air pollution. Studies in animals have indicated that air pollution particulates can speed degeneration of the nervous system. And human studies have found that air pollution exposure — particularly from traffic exhaust and burning wood — is associated with greater dementia risk.
Head trauma. People who've had a severe head trauma have a greater risk of Alzheimer's disease. Several large studies found that in people age 50 years or older who had a traumatic brain injury (TBI), the risk of dementia and Alzheimer's disease increased. The risk increases in people with more-severe and multiple TBIs. Some studies indicate that the risk may be greatest within the first six months to two years after the TBI.
Sleep disturbances. People who have sleep apnea and other sleep disturbances might be at higher risk of developing dementia.
Vitamin and nutritional deficiencies. Low levels of vitamin D, vitamin B-6, vitamin B-12 and folate can increase your risk of dementia.
Medications that can worsen memory. Try to avoid over-the-counter sleep aids that contain diphenhydramine (Advil PM, Aleve PM) and medications used to treat urinary urgency such as oxybutynin (Ditropan XL).
Also limit sedatives and sleeping tablets and talk to your doctor about whether any of the drugs you take might make your memory worse.
PSCI post stroke cognitive impairment
belays, describes, ascribed indicative of underlying symptoms events illneses etc and is not natural or inasmuch as env toxins etc natural (vaccinesqm, future of nanoetc
1. Goals: Independent, Productive, Art producing, Engaged, Inspired,
Stroke symptoms (such as Post Stroke Apathy, loss of mobility/favoring a side, and possibly hand tremors) are often resulting from lesions in hipocampus and basal ganglia. There are experimental medicines in this report that treat not only symptoms but, as neurotrophic factors and hormonal growth signaling factors act as neurorehabilitative and neurogenerative agents. Also the past couple years have shown tremendous progress in stem cell therapies applied to a wide gamut of application, including recent trials of plurient cellimplementation.
The most effective treatment are a combination of therapy that includes:
1) working with endocrinological specialists to evaluate dosages (as per the link to 'Clearfield Hypopituitarism' plan, or similar)
2) working with a neurological specialist (better more precise imaging of affected regions to determine variety of cell types and amount per region, presence of lesions, etc.) and determining the best medicines
3) Working with Psychologist and Psychiatrist
4) Examining Non-Allopathic ('Alternative') Medicine
5) Maintaining healthy diet, sleep, exercise and encouragement in self directed planning and execution of socializing opportunities, artworks and other goals
How to use this site:
1) If you are lost in navigation, use one of the 8 links at the top of the browser ('Main Overview', 'Allopathic Medicine', etc)
2) Please review pdf's linked above (or to the left depending on browser).
The first 'Traumatic Brain Injury Rehabilitation, Treatment, and Case Management, Fourth Edition' has been inputed, though Chapters 15-17 warrant review.
The second 'Clearfield Panhypopituitarism and TBI' is covered in the HRT (Hormone Replacement Therapy) section, has been inputed and appears an integral resource/strategy/guideline/guide for review.
Introduction: Multidisciplinary approach required (From Neurorehabilitation of stroke https://www.researchgate.net/publication/51688267_Neurorehabilitation_of_stroke )
Despite ongoing improvements in the acute treatment of cerebrovascular diseases and organization of stroke services, many stroke survivors are in need of neurorehabilitation, as more than two-thirds show persisting neurologic deficits. While early elements of neurorehabilitation are already taking place on the stroke unit, after the acute treatment, the patient with relevant neurologic deficits usually takes part in an organized inpatient multidisciplinary rehabilitation program and eventually continues with therapies in an ambulatory setting afterwards. A specialized multidisciplinary neurorehabilitation team with structured organization and processes provides a multimodal, intense treatment program for stroke patients which is adapted in detail to the individual goals of rehabilitation. There are many parallels between postlesional neuroplasticity (relearning) and learning in the development of individuals as well as task learning of healthy persons. One key principle of neurorehabilitation is the repetitive creation of specific learning situations to promote mechanisms of neural plasticity in stroke recovery. There is evidence of achieving a better outcome of neurorehabilitation with early initiation of treatment, high intensity, with specific goals and active therapies, and the coordinated work and multimodality of a specialized team. In this context, interdisciplinary goal-setting and regular assessments of the patient are important. Furthermore, several further potential enhancers of neural plasticity, e.g., peripheral and brain stimulation techniques, pharmacological augmentation, and use of robotics, are under evaluation.
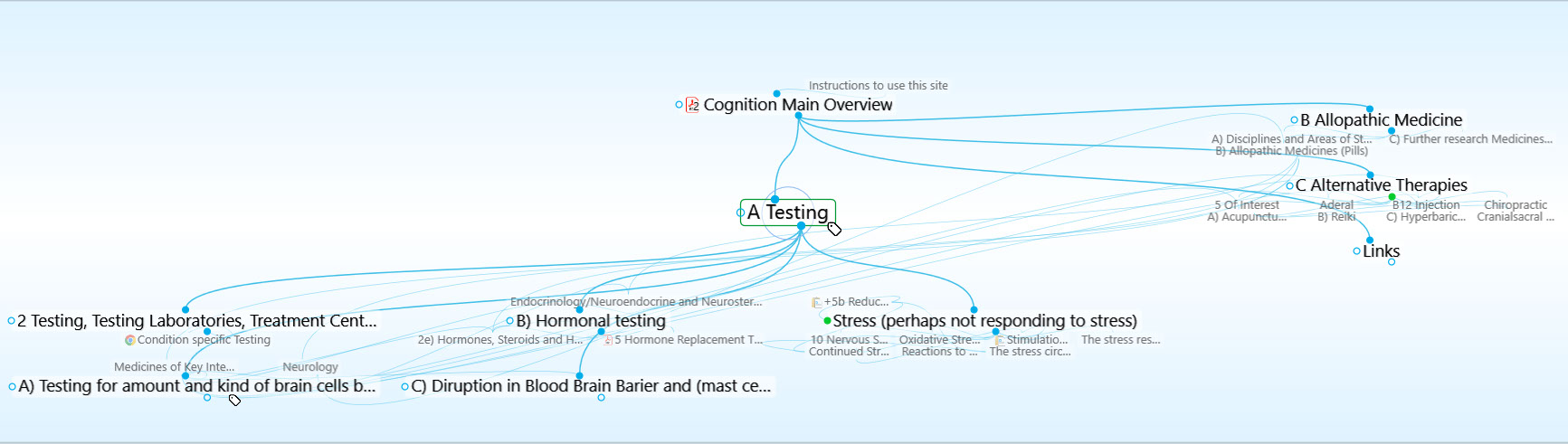
Testing for amount and kind of brain cells by evaluating R2t\* signal from MRI scan
From: https://m.medicalxpress.com/news/2018-09-overlooked-mri-scans-amount-kind.html
Overlooked signal in MRI scans reflects amount, kind of brain cells
September 24, 2018 , Washington University School of Medicine
An MRI scan often generates an ocean of data, most of which is never used. When overlooked data is analyzed using a new technique developed at Washington University School of Medicine in St. Louis, they surprisingly reveal how many and which brain cells are present—and show where cells have been lost through injury or disease.
The findings, published online the week of Sept. 24 in Proceedings of the National Academy of Sciences, eventually may lead to new ways to diagnose Alzheimer's disease, multiple sclerosis, traumatic brain injury, autism and other brain conditions through a simple brain scan.
"There's no easy way to detect the loss of neurons in living people, but such loss plays a role in many neurological diseases," said Dmitriy Yablonskiy, Ph.D., a professor of radiology at the university's Mallinckrodt Institute of Radiology, who directed this study together with Marcus Raichle, MD, a professor of radiology and the Alan A. and Edith L. Wolff Distinguished Professor of Medicine. "We've shown in the past that there's a signal that goes down in parts of the brain in people with Alzheimer's disease, multiple sclerosis and traumatic brain injury, but we didn't know what it meant. Now, we know it means neurons have died in those areas."
Most researchers studying brain function with MRI are only interested in a small portion of the MRI signal. They want to see how the MRI signal changes when a person performs a task, not what stays the same. Researchers trying to understand vision, for example, focus on the signal variation due to the brain activity when a person looks at a picture, and discard the parts of the signal that hold steady. But that is like looking at the waves along the surface of the ocean, and ignoring the mass of water beneath.
Yablonskiy, Raichle and colleagues including Jie Wen, Ph.D., an instructor in radiology and the study's first author, Manu Goyal, MD, an assistant professor of radiology and of neurology, and Serguei Astafiev, Ph.D., a senior scientist in psychiatry, decided to find what the rest of the ocean could tell us about how the brain works.
They analyzed the background data on an MRI scan and found a signal, which they called R2t\*, that remained largely unchanged when people performed tasks but varied across parts of the brain. Then, they compared the R2t\* signal with data from the Allen Human Brain Atlas, which maps genes active in various areas of the brain. The researchers found three sets of gene networks that tracked with the R2t\* signal—the genes were more active where the signal was strong, and less active where the signal was weak. These groups of genes, it turned out, reflected the different kinds and numbers of brain cells, and the extent of connections between them.
In other words, this quick new MRI scan gave the researchers all they needed to know to determine how densely packed and interconnected the neurons are in any part of the brain. This information could help us understand how a person's brain develops and changes from infancy to old age, and how we build memories and learn. It could also give clues to brain illness or injury.
"We did some studies on traumatic brain injury where we found some areas of the brain are already losing neurons even though the standard scans show nothing," Yablonskiy said.
The researchers also applied their technique to the hippocampus—the memory center of the brain—in people with Alzheimer's disease. They found that not only was the hippocampus smaller than in healthy people, but the remaining part was not healthy—it had lost cells and begun to decay.
"There are MRI scans now that can detect brain atrophy even before people show symptoms of Alzheimer's disease," Yablonskiy said. "Our technique can show the brain degrading even before it begins to atrophy."
Yablonskiy and colleagues are now working on applying their technique to brain diseases and disorders including Alzheimer's, schizophrenia, multiple sclerosis and autism, as well as to understanding how a healthy brain develops and grows.
"We've developed a method that takes a six-minute scan and tells you what types of cells are there and how extensively they're connected," Yablonskiy said. "As babies develop, neurons start growing, they connect with each other, they start forming memories. Nobody really knows how this is done. But this method could help us understand normal development, as well as how brain diseases develop."
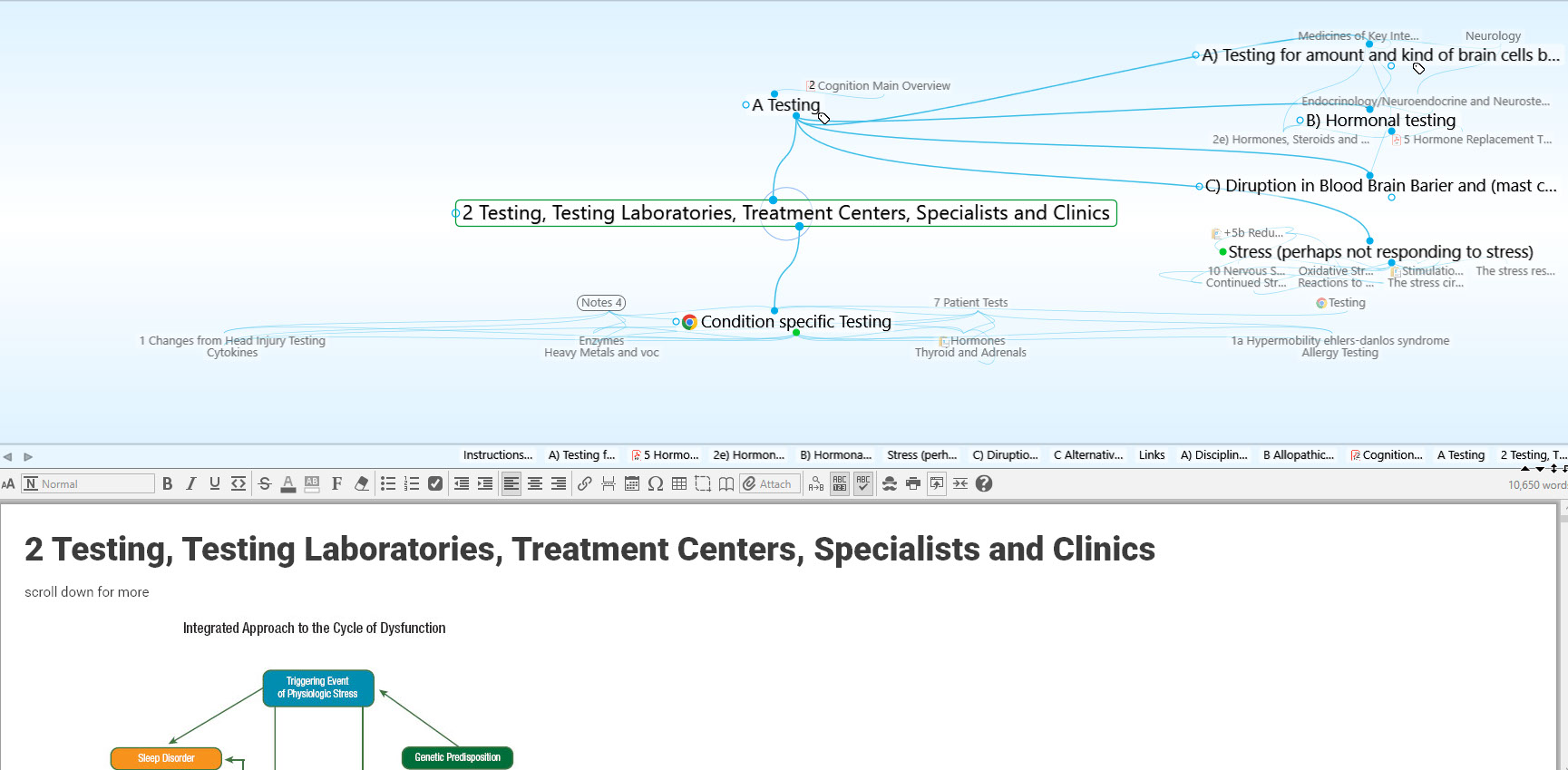
From: Pharmacotherapy Prescription Trends for Cognitive-Behavioral Disorder in Patients With Brain Injury in Korea https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5852227
Methylphenidate (52.1%) and amantadine (16.7%) were the most frequently prescribed medications for attention deficit. Donepezil (52.7%), memantadine (20.3%) and rivastigmine (20.3%) were the most frequently prescribed medications for memory deficit. Methylphenidate (42%) and amantadine (28%) were the most frequently prescribed medications for arousal deficit. SSRIs (55.8%) and SNRIs (36.5%) were the most frequently prescribed medications for depression. Table 3 shows the most commonly prescribed medications for treatment of each of the target symptoms associated with cognitive-behavioral disorder. Physiatrists generally prescribed a combination of two cognitive-behavioral medications (39%), followed by a combination of three medications (29%), monotherapy (20%) and a combination of four medications (6%) (Fig. 2). Donepezil and methylphenidate (96%) were the most preferred medications for cognitive-behavioral improvement, followed by SSRIs (84%), quetiapine (84%), bromocriptine (72%), and amantadine (68%). Among the several medications, respondents preferred donepezil as a first line drug and methylphenidate as a second line drug (19.1%) in combination pharmacotherapy (Fig. 3).
More information: Jie Wen el al., "Genetically defined cellular correlates of the baseline brain MRI signal," PNAS (2018). www.pnas.org/cgi/doi/10.1073/pnas.1808121115
examine regions affected (and effects on metabolic hypometabolic state).
what medicines may help the regions affected.
As mentioned, the MRI scan on 5/13/19 shows no new aneurysm, however please scan the results with the R2t\* as linked in prev email Scan results indicate and by looking at mri as linked determine more if excess, lack lessions etc would further elucidate subject perhaps bolster clearfield
1) Of the five medicines listed in the previous email, after examining and weighing the possible side effects, may Amantidine (one )be employed as therapies adjunct (to the increase in Venlaflaxin and 'occupational' type therapies)?
From: Neuropharmacology In TBI: What We Know & What We Don’t - ppt download Mount Sinai Hospital
Agents to Support Executive Function:
What We know:
There exits evidence to support use of Amantadine.
Meythaler et al 2002 found amantadine improved neurorecovery in TBI with DAI in Double-Blind randomized crossover 6 week trial
35 patients with TBI, GCS of 10 or less
Amantadine 200mg/day/placebo given in first 6 weeks or 2nd 6 weeks
Improved MMSE, DRS, GOS, and FIM cognitive Score in amantadine group in first 6 weeks, and no improvement in next 6 on placebo. No sig effect on GOAT
In group on amantadine in weeks 6-12, statistical sig improvment in MMSE, DRS, GOS, an FIM cog after active drug
No sig effect on GOAT
Conclusion: rapid functional improvement on amantadine when given in first 3 months after injury
Kraus et al 2005 found improvements of tests of executive function after treatment with amantadine in patients with chronic TBI
N=22, amantadine 200mg BID
Outcome measures: neuropsychological testing (pre and post-12 week treatment) and PET scanning on 6 participants
Results:
Significant improvements on tests of executive function
Analysis of PET data demonstrated significant increase in left prefrontal and medial temporal cortex glucose metabolism
This correlated with improvement in measures of executive function
Memory and attention did not significantly improve
The evidence to support the use of Atomoxitine is limited and conflicting.
In animal models with experimental TBI, low dose atomoxetine attenuated cognitive deficits after experimental TBI in a water maze study (Reid and Hamm 2008)
Performed worse with higher doses
No effect when started 11 days post injury
However: remember Ripley et al, 2014:
In adults with TBI at least 1 year from injury Atomoxetine dosed at 20 mg 2 x /day for 2 weeks did not improve scores on measures of attention (Ripley et al, 2014)
Citicoline does not improve cognition and function when used acutely or subacutely.
Citicoline is an endogenous compound, thought to have neuroprotecticve properties.
Citicoline is an approved therapy for TBI in 59 countries
COBRIT: Citicoline Brain Injury Treatment Trial was a large phase 3 double blind, RCT among 1213 patients at 8 US trauma centers to investigate Citicoline vs. placebo in pts. with TBI (mild, mod and severe), Zafonte et al 2012
90 days if citicoline 2000mg vs placebo initiated within 24 hours of injury
At 90 days measured TBI clinical trials network core battery (trails a and b, GOS-E, COWAT, CVLT, PSI, DS and WAISIII, Stroop 1 &2)
At 90 days there was no sig difference btwn 2 groups on the battery
Favorable imrpovement for the GOS-E in the citicholine group
COBRIT questions worldwide use of Citicholine
The evidence to support the use of Bromocriptine is limited
McDowell et al 1998 examined low dose bromocriptine on frontal lobe (working memory and executive function)
N=24,
double blind placebo controlled crossover
Gave bromocriptine 2.5 mg with testing 90 minutes later
Bromocripine improved tests of executive function and dual task performance, but not working memory or attention
The evidence to support the use of SSRIs is limited.
Horsfield et al 2002 studied Prozac 20-60 mg/day after TBI
N=5, 8 months
Cog and Memory tests: at baseline and after 8 months: Trails A, attention motor speed test, part of WAIS II, Some portions of test, but need addtiional research
Sertraline caused psychomotor slowing in further studies (next slide)
What We Don’t Know:
Conflicting results in the literature.
Large recent meta-analysis “Impact of Phamacolological Treatemtns on Cognitive and Behavioral Outcome in the Postacute States of Adult TBI,” Wheaton et al 2011, found:
SSRIs:
Citalopram and carbamezepine improve psychosocial function.
Serotonin increases post concussive sx and decrease psychomotor speed.
Milnacipran (serotonin and Noradren) improvement on cog testing (MMSE).
Dopaminergics:
Methyphenidate supported for psychosoical, cognitive, but mixed results on attention.
Amantadine improved global outcome on DRS (Maythaler 2002).
Cholinergic:
Support of donepazil for attention and memory (Zhang et al 2004), but no improvement with physiostigmine and lecithin.
Peptide Treamtents: Lysine/vasopressin had 1 study supporting improved memory, cerebrolysine improved memory and attention, no studies support desmopressin use.
CDP-Choline may improve memory, but impair attention.
Summary and Practice Recommendations:
Amantadine has most support for improving executive function after TBI, but is not supported in memory or attentional recovery.
It is unclear how bromocriptine improves executive function.
Citicoline and atomoxetine do not have literature that supports use in promoting cognitive function after TBI.
When treating executive function deficits, it is important to treat other impairments (emotional and behavior disturbances and motor dysfunction).
The literature is limited in medication use to treat executive function deficits.
SSRI’s have utility in non-depressed patients with stroke, with good functional results.
FLAME trial showed that in patient with ischemic stroke and moderate to severe motor deficits, the early prescription of fluoxetine with physical therapy led to enhanced motor recovery after three months.
Patients treated with citalopram for three months post stroke had a better recovery from disability one year after stroke than patients who did not receive antidepressant therapy.
Citalopram can enhance dexterity in chronic stroke patients.
Donepezil may improve the FIM motor score in elderly cognitively impaired patients post stroke.
Reboxetine induced a significant improvement in tapping speed and grip strength in ten patients with chronic stroke.
Currently there is limited evidence for supporting or refuting the use of levodopa to support post-stroke motor recovery.
Currently there is limited evidence for supporting or refuting the use of amphetamines to support post-stroke motor recovery.
The evidence for the efficacy of dopaminergic agents in aphasia therapy is mixed.
Donepezil has been shown to improve the severity of aphasia and motor aspects of speech in poststroke aphasia.
Memantine alone or combined with constraint-induced aphasia therapy in chronic poststroke aphasia patients improved aphasia severity. These effects persisted on long-term follow-up.
Melatonin has value for sleep disorders following head injury.
Trazodone is a multifunctional drug that helps patients with TBI sleep.
Amantadine is the agent of choice for treating profound hypoarousal following TBI, especially when a patient has a disorder of consciousness.
Amantadine and/or methylphenidate may improve emergence from coma in hypoxic ischemic encephalopathy resulting from cardiac arrest.
A very small number of patients with disorders of conscious are responders to zolpidem, and it is not possible to distinguish responders in advance.
Agitation is fairly common after brain injury, with incidence of 10-30% and in some reports 90%, and poses a danger to the patient and caregivers, interferes with rehabilitation, and affects disposition.
Clinician must evaluate and treat for treatable of agitation/behavioral problems that include environment, neurologic, metabolic, pain, medication, etc.
Stable environment is key as well as removing contraindicated medications.
Amantadine, methylphenidate, propranolol, valproic acid have evidence for treatment of agitation after brain injury.
Quetiapine can be used in severe cases of severe agitation, however olanzapine has slightly more support when agitation exists with psychosis.
Check levels, CBC and LFT as well as EKG where indicated.
Remember rules for any medication use: Start low and go slow, and remove when agents agitation begins to resolve.
Methylphenidate relatively safe, and recommended to improve attention, processing speed, concentration and vigilance but limited evidence that it improves functional outcome.
Atomoxetine does not significantly improve performance on measures of attention.
Cholinesterase inhibitors have preliminary evidence for recovery of attention.
We need additional studies to support use of medications for memory recovery after traumatic brain injury.
Escitalopram and Donepezil are supported in the literature for memory recovery in CVA.
2) Diketopiperazine
From: 'Neuroprotection for traumatic brain injury: translational challenges and emerging therapeutic strategies' https://www.cohenveteransbioscience.org/wp-content/uploads/2015/10/Loane-Trends-Pharmacol-Sci-2010.pdf
Diketopiperazines are cyclized dipeptides that were developed through a rational drug design program based on the tripeptide thyrotropin-releasing hormone (TRH) 74. TRH and TRH analogs inhibit multiple secondary injury factors and processes 74. They were shown to be highly neuroprotective in experimental neurotrauma across many laboratories and a small clinical randomized study of TRH in human SCI was promising 75. Four structurally different diketopiperazines demonstrated significant neuroprotective properties both in vitro and in animal TBI studies 76. One of these (35b) showed effectiveness across TBI models and species. In neuronal cell cultures, 35b provided neuroprotection in multiple models of necrotic and apoptotic cell death 77. Intravenous administration of 35b reduced both lesion volume and improved functional recovery after fluid percussion injury (FPI) in rats and CCI in mice 77,78. The therapeutic window was at least 8 hours. Treatment also significantly reduced apoptotic cell death 77.
Effects appeared to be pleiotropic, with treatment reducing multiple potential secondary injury factors (cyclins, calpains, cathepsin), while upregulating various endogenous neuroprotective and neurotrophic factors (BDNF, HSP-70, HIF-1) 76,79. In addition, data are available regarding pharmacokinetics, brain penetration after systemic administration and preclinical toxicology in the rat. Similar pleiotropic neuroprotective effects were reported with another diketopiperazine - cyclo-L-glycyl-L
treatment improved functional recovery and long-term histological outcomes, and reduced caspase-3 mediated apoptosis and microglial activation 80.
Given their multipotential neuroprotective effects in experimental TBI models, their clinically relevant therapeutic window, and their safety profile, the diketopiperazines are attractive candidates for further clinical investigation.
3) Peptide modulation
From: Traumatic brain injury and recovery mechanisms: peptide modulation of periventricular neurogenic regions by the choroid plexus–CSF nexus
In traumatic brain injury (TBI), severe disruptions occur in the choroid plexus (CP)–cerebrospinal fluid (CSF) nexus that destabilize the nearby hippocampal and subventricular neurogenic regions. Following invasive and non-invasive injuries to cortex, several adverse sequelae harm the brain interior: (i) structural damage to CP epithelium that opens the blood–CSF barrier (BCSFB) to protein, (ii) altered CSF dynamics and intracranial pressure (ICP), (iii) augmentation of leukocyte traffic across CP into the CSF–brain, (iv) reduction in CSF sink action and clearance of debris from ventricles, and (v) less efficient provision of micronutritional and hormonal support for the CNS. However, gradual post-TBI restitution of the injured CP epithelium and ependyma, and CSF homeostatic mechanisms, help to restore subventricular/subgranular neurogenesis and the cognitive abilities diminished by CNS damage. Recovery from TBI is faciltated by upregulated choroidal/ependymal growth factors and neurotrophins, and their secretion into ventricular CSF. There, by an endocrine-like mechanism, CSF bulk flow convects the neuropeptides to target cells in injured cortex for aiding repair processes; and to neurogenic niches for enhancing conversion of stem cells to new neurons. In the recovery from TBI and associated ischemia, the modulating neuropeptides include FGF2, EGF, VEGF, NGF, IGF, GDNF, BDNF, and PACAP.
Homeostatic correction of TBI-induced neuropathology can be accelerated or amplified by exogenously boosting the CSF concentration of these growth factors and neurotrophins. Such intraventricular supplementation via the CSF route promotes neural restoration through enhanced neurogenesis, angiogenesis, and neuroprotective effects. CSF translational research presents opportunities that involve CP and ependymal manipulations to expedite recovery from TBI.
![]()
also the presentation clearfield is very compelling, that is that medium range testing as a whole may be considered low that regions affected and hypofunction, and rohibinol etc. on our end we continue occupational therapy and have increased her walking challenge to up hills and longer outings as well as smn, as are the other 5 medicines. similar hypometabolic etc, and clinic
A compelling aspect to neorotrphic meds is the prospect of nourishing and repairing damaged cells and kickstarting misconstrued paths/states locked in to negative cost inneficient drawing mito states as well as disruptoions in the neuropeptide enzymatic pathwaychannels mechanisms neuropeptides etc. so, interested in following thnks
edonerpic maleate, a neural plasticity enhancer, could be a clinically potent small compound with which to accelerate rehabilitation after brain damage.
4) Inosine
Despite years of research, no effective therapy is yet available for the treatment of traumatic brain injury (TBI). The most prevalent and debilitating features in survivors of TBI are cognitive deficits and motor dysfunction. A potential therapeutic method for improving the function of patients following TBI would be to restore, at least in part, plasticity to the CNS in a controlled way that would allow for the formation of compensatory circuits. Inosine, a naturally occurring purine nucleoside, has been shown to promote axon collateral growth in the corticospinal tract (CST) following stroke and focal TBI. In the present study, we investigated the effects of inosine on motor and cognitive deficits, CST sprouting, and expression of synaptic proteins in an experimental model of closed head injury (CHI). Treatment with inosine (100 mg/kg i.p. at 1, 24 and 48 h following CHI) improved outcome after TBI, significantly decreasing the neurological severity score (NSS, p<0.04 vs saline), an aggregate measure of performance on several tasks. It improved non-spatial cognitive performance (object recognition, p<0.016 vs saline) but had little effect on sensorimotor coordination (rotarod) and spatial cognitive functions (Y-maze). Inosine did not affect CST sprouting in the lumbar spinal cord but did restore levels of the growth-associated protein GAP-43 in the hippocampus, though not in the cerebral cortex. Our results suggest that inosine may improve functional outcome after TBI.
![]()
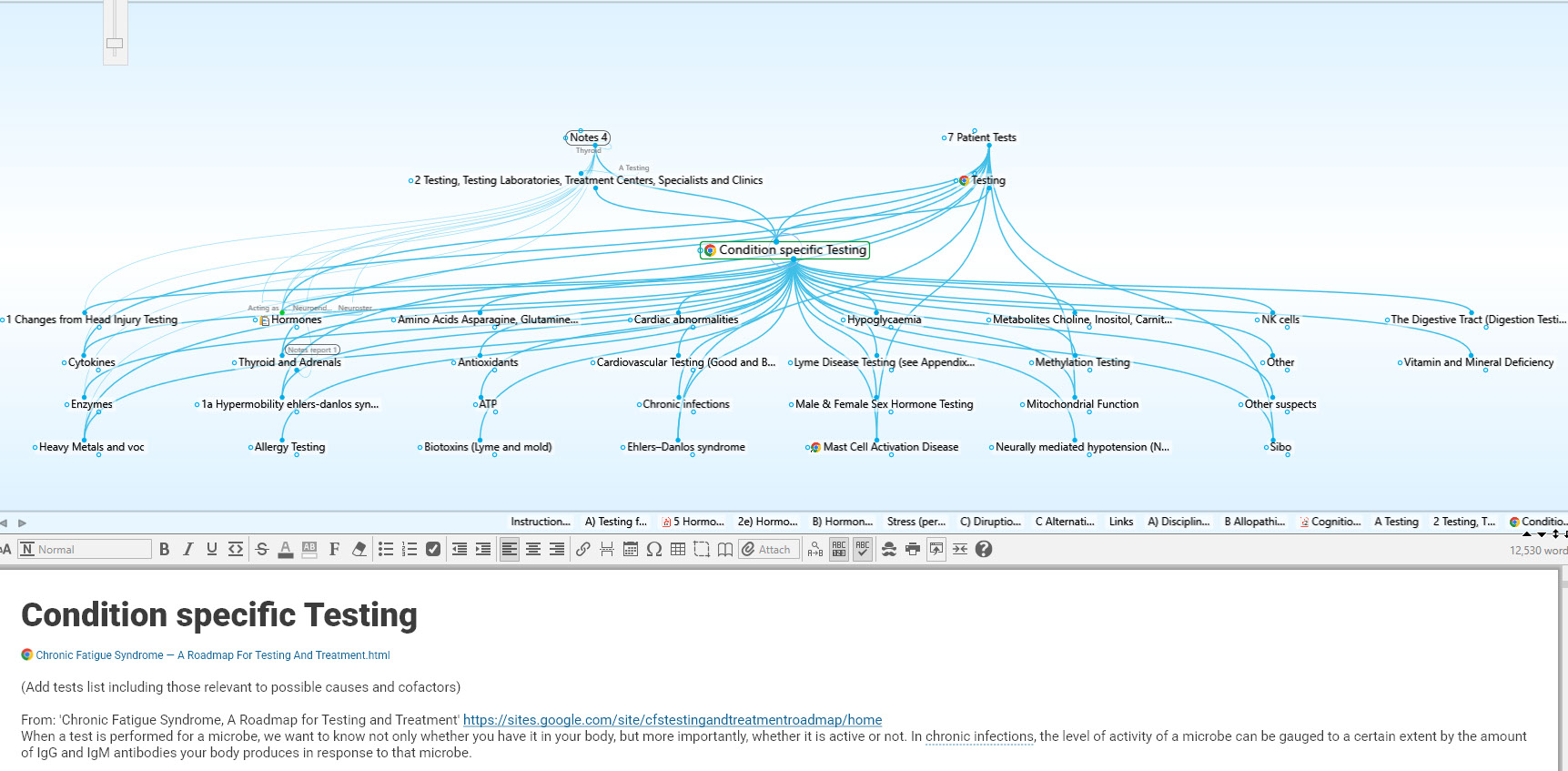
From: 'Chronic Fatigue Syndrome, A Roadmap for Testing and Treatment' https://sites.google.com/site/cfstestingandtreatmentroadmap/home
Note that Th2 to Th1 shifting immunomodulators can make you feel worse for the first few months, but benefits accrue after that initial period. Dr Paul Cheney believes that the immunomodulator Imunovir will lose it's effect if you do not "pulse" it. Pulsing means taking regular breaks Imunovir, using an on/off regimen such as taking Imunovir for 5 days, then stopping for 2 days. Oxymatrine however should not be pulsed. Note that several ME/CFS doctors say that the supplement inosine is just as effective as Imunovir, but much cheaper (Imunovir is based on inosine).
multifacet approach. if start bottom up would start with aderol. looking top down which regions affected, x and y complement multiregions. also instead of 2 drugs different side effects, 1 drug 1 set of side effects.
More on Amandinine
Dr David Bell found amantadine 25 mg to 50 mg twice daily helps ME/CFS, but says higher doses can exacerbate symptoms.1
![]()
From: Drug Speeds Recovery After Traumatic Brain Injury - MedicineNet
A drug that's typically used to treat the flu and Parkinson's disease appears to speed recovery in traumatic brain injury patients, a new study indicates.
Traumatic brain injury (TBI) victim who weren't fully conscious and were discharged to rehabilitation facilities after hospitalization were given amantadine hydrochloride. The drug is already given "off-label" to such patients, but if and how much it helps has remained unclear.
While taking the drug, the patients given amantadine scored better on behavioral tests that measure how well the brain is functioning compared to a group of patients given a placebo, researchers report in the March 1 issue of The New England Journal of Medicine.
"Amantadine appeared to increase the rate of recovery compared to placebo. Patients got better faster while they were on the drug," said study co-author Joseph Giacino, director of rehabilitation neuropsychology at the Spaulding Rehabilitation Hospital, in Boston, and an associate professor in the department of physical medicine and rehabilitation at Harvard Medical School.
Study co-author Dr. John Whyte, director of the Moss Rehabilitation Research Institute at Albert Einstein Healthcare Network, in the Philadelphia area, said previous observational studies had suggested amantadine improved the rate of recovery. While the medicine is already commonly prescribed off-label to treat people suffering from prolonged disorders of consciousness, he said this is the first placebo-controlled trial of the drug in patients who were either in a vegetative state (wakeful but not aware) or a minimally conscious state (able to track with their eyes).
"There were many hypotheses out there about what this drug should do, but there was very little data to support or refute those hypotheses," Whyte explained.
For the study, 184 patients from 11 medical centers in three countries were enrolled. They had all suffered a TBI within the previous one to four months. Half received amantadine while the other half were given a placebo for the first four weeks of the six-week study. Both groups were followed up for two additional weeks, Whyte said.
The researchers used the Disability Rating Scale (DRS) to monitor patients' progress during the treatment and follow-up period. The test measures eye opening, verbal ability and motor response, among other functions, Giacino said.
"During the four-week treatment period, recovery was significantly faster in the amantadine group than the placebo group," said Giacino.
Whyte said during his 25-year career as a brain trauma rehabilitation physician there have been no groundbreaking treatments for these patients. TBI rehabilitation can take months, or years, and many patients do not have the health insurance or private funds to access good rehabilitative care, so a drug that could speed recovery would be a boon, he said.
The ability of patients in a vegetative state or those in the MCS "to access rehab has gotten less and less," Whyte said. "Many of these patients go straight to a nursing home or home with family." He noted that TBI remains the most common cause of death and disability in people between the ages of 15 and 30.
The new finding "is very exciting because we have a new tool to help improve these patients in their early outcome," said one expert, Dr. J. Javier Provencio, director of the Neurocritical Care Fellowship Program at the Cerebrovascular Center of the Cleveland Clinic Neurological Institute.
"The take-home message is that this medicine is promising for patients in a very certain setting. I think the results have to be taken very strictly and not extrapolated to other conditions," said Provencio.
He noted that the rate of improvement in the drug group slowed in weeks five and six. By the study's end, the overall improvement from baseline between the placebo group and the amantadine group was identical.
That means that, "it is still unclear whether the effects last," Provencio said. "In the study, by week six, the effect difference was getting smaller. I hope they follow these patients out to a year to see how they do."
Co-author Giacino said the researchers were surprised when they saw an immediate leveling off between the two groups in the final two weeks.
"But when I take a step back, it is even stronger evidence that this drug was doing something," he added.
Neurologist Dr. Daniel Labovitz, of Montefiore Medical Center in New York City, believes hope should remain in check despite the promising results. "It's not a home run. It's a small change and it was temporary, and I think that would be the message that has to come through."
Labovitz said the drug appears to be gently waking the patients. "If this trial holds up in larger, longer-term studies, maybe you can enhance the ability of rehabilitation therapists to interact with patients while they're on the drug."
Giacino said they researchers also aimed to look at side effects of amantadine.
"There was not a single category where the amantadine group had a higher rate of side effects than the placebo group," he said.
Whyte said that while this research may influence more rehabilitation experts to use amantadine for this type of patient, more challenges remain before the drug's impact is completely understood.
The non regenerating capacity of an injured adult brain has been challenged in the recent past and neural plasticity has been documented in both global and focal models of animal ischemia 1 the prospects of repairing an injured nervous system using putative restorative therapies seem promising.
Numerous pharmacological agents are under investigation since a decade which reflects developmental processes. Brain derived neuro trophic factor 2 (BDNF), hepatocyte growth factor 3 (HGF), granulocyte macrophage colony stimulating factor (FM-CSF) 4,5 and other agents such as minocycline has proved to be efficacious in restoring neuro-functional benefits in preclinical and clinical studies.
Phosphodiesterase 5 inhibitors, statins and agents that increase high density lipoproteins and hormones that pioneered the use of thymosin beta 4 and carbamylated erythropoietin for the treatment of stroke and neural injury have been in use extensively. Chopp et al. 6 published literature recently on the use of multifactor restorative agent cerebrolysin for stroke therapy.
Pathophysiology of ischemic stroke 7 The degree and duration of impaired blood flow determines the extent and pattern of cerebrovascular damage. Ischemia causes loss of membrane potentials leading to anoxic depolarization and kills uniquely vulnerable neurons such as pyramidal neurons in the CA1 and CA4 zones of the hippocampus while sparing other neurons and glial cells. Deprivation of oxygen supply to the brain tissue leads to activation of the ischemic cascade with a series of molecular mechanisms being activated. There is depletion of adenosine triphosphate and consequent high levels of lactate and unbuffered hydrogen ions.
Failure of energy dependent mechanisms lead to deterioration of membrane ion gradients, opening of selective ion channels and equilibration of most intracellular and extracellular ions. Thus potassium ions leave the cell, sodium, chlorine and calcium enter and many excitatory neurotransmitters (glutamate, aspartate) are released in potentially toxic concentrations. The intracellular entry of calcium is made largely possible by the activation of two types of receptors, Voltage gated (L-type) and/or several N-methyl-d-aspartate (NMDA) and quisqualate (Q) post synaptic receptor/channel complexes by glutamate. Agents that prevent white blood cells from adhering to vessel walls, limit formation of free radicals, or promote neuronal repair may protect the brain from additional injury during reperfusion.
Neuroprotective agents that work primarily during reperfusion may have a longer window of therapeutic effect than drugs that work earlier in the ischemic cascade.
Agents for neuroprotection NMDA receptor modulation 8: The most commonly studied neuroprotective agents for acute stroke which block N-methyl-d-aspartate (NMDA) receptors. Dextromethorphan, a noncompetitive NMDA antagonist was the first NMDA antagonist studied in human stroke patients with a large efficacy trial using GV150526 with 1367 patients completed in 2000.
Although the drug was reported to be safe and well tolerated, no improvement was observed in any of the 3-month outcome measures. Magnesium is another agent with actions on the NMDA which reduce ischemic injury by increasing regional blood flow, antagonizing voltage-sensitive calcium channels and blocking the NMDA receptor with Magnesium Phase III (FAST-MAG) Trial currently under run.
Non NMDA receptor modulation: Clomethiazole, a g-amino butyric acid agonist, decreases excitatory neurotransmission by increasing activity of inhibitory pathways. In Europe, clomethiazole’s central nervous system inhibitory properties have been used for anticonvulsant and sedative effects. The potential efficacy of Clomethiazole as a neuroprotective agent in ischemia was first investigated in Europe as part of the Clomethiazole Acute Stroke Study. Patients received a 24-h IV infusion of Clomethiazole or placebo within 12 h of symptom onset. Nalmefene (Convene) is a narcotic receptor antagonist that reduces levels of excitatory neurotransmitters contributing to cellular injury in early ischemia. Post hoc analyses of early studies suggest that the drug may have more benefit in patients younger than 70 years. However, a later clinical trial in which the drug was administered intravenously (IV) within 6 h of symptom onset showed no benefit. The exact mechanism of action of lubeluzole, a drug effective in animal models, is unclear. The drug may block sodium channels in cells. In addition, it may reduce the release of nitric oxide, a neurotransmitter generated by activation of the NMDA receptors. Free radical agents like NXY059 are under investigation in Stroke trials 9.
Tetracycline derivatives: Minocycline: Minocycline is the second generation tetracycline derivative known to have antiinflammatory effects independent of its antimicrobial action.
Recent studies have shown that minocycline prevents microglial activation, and also has notable beneficial effects in animal models of global and transient focal cerebral ischemia and other brain injuries 10. The proposed mechanisms of minocycline include anti-inflammatory effects, reduction of microglial activation, MMP reduction, nitric oxide production and inhibition of apoptotic cell death 11. In a randomized single blinded study, Padma et al. 12 studied the effects of oral Minocycline (200 mg/ day for 5 days) post stroke versus placebo. Out of 50 patients included in the trial, patients who received minocycline had significant improvement in stroke outcome as noted on NIHSS, mBI and mRS scores. Larger trials are needed to confirm the above findings.
Agents for Neurorestoration
Augmentation of nitric oxide cascade Nitric Oxide is an integral molecule involved with maintaining endothelial cell integrity, as well as participating in hemodynamic homeostasis 13. NO is produced by a variety of cells, including vascular smooth muscle cells and neurons suggesting its role in neurogenesis by an increased expression of neuronal NO synthase within the sub ventricular zone (SVZ) during embryogenesis. It has been reported that treatment with NO 24 hours post stroke in rat models augmented neurogenesis and improvement in functional outcome despite no change in infarct volume. NO is also a potent activator of soluble guanylate cyclase, which converts GTP to cGMP 14. Delivery of NO donor increases cGMP levels in both ischemic and non-ischemic rats, suggesting a putative role of NO in neuro-angiogenesis and a downstream mediator of cGMP whose action is increased by inhibiting Phosphodiesterase 5 (PDE5) enzyme. The strategy of increasing the downstream mediator cGMP without affecting NO levels may be preferred due to the mixed outcomes in stroke reported in animal models following alterations in NO levels. A major PDE5 inhibitor is sildenafil. Animals treated with sildenafil post stroke achieved significant and substantial increase in neurological functional recovery. Phase I trials in humans with acute stroke are currently on going. An improved cerebral blood flow (CBF), neurogenesis and synaptogenesis following experimental stroke, even when therapy is with Sildenafil up to 1 caged animal is delayed 15.
Studies have reported the improvements in functional outcomes occurred despite no change in infract volume, nevertheless these functional improvement will need to be demonstrated in clinical trials. Functional MRI or diffusion tensor imaging (DTI) may assist in answering these questions which demonstrate improvements in structure, organization and functional connectivity via acting as bio surrogate markers. Other agents such as statins, also greatly enhance neurological recovery post stroke. Drugs which increase high density lipoproteins (HDL) such as slow release niacin have also been employed to treat stroke and have shown substantial neurological benefit when treatment is initiated days after stroke. Other Neurorestorative agents under investigation are erythropoietin (EPO), carbamylated EPO (CEPO) and Thymosin B4. Current physical rehabilitation therapies could be enhanced using pharmacological approach thereby helping to re establish lost neuronal connections. It has been elegantly established by Clarkson et al. 16 that inhibiting tonic GABA (gamma amino butyric acid) signaling days improves locomotors function after stroke, suggesting that therapeutic approaches are less time sensitive than acute reperfusion therapies. P13k/Act and sonic hedgehog (Shh) pathways are activated by molecular and signal transduction genes which promote brain plasticity.
Various pharmacological agents by means of signal transduction pathways can induce CNS plasticity that enhances functional recovery from stroke and neural injury.
Neurotrophic agents and growth factors
Basic fibroblast growth factor (FGF) was shown to protect against excitatory amino acid toxicity In vitro, basic FGF chimeric peptide was highly effective in reducing infarct volume in a rodent model of permanent focal ischemia 17. FGF has been investigated in phase II/III trials. The results of the Clinical Safety Trial of Intravenous Basic Fibroblast Growth Factor in Acute Stroke did not report any serious adverse events 18. The European-Australian phase II/II safety and efficacy trials were terminated in the middle as no significant improvement was noted, although there was a trend towards treatment advantage19.
Recombinant erythropoietin (Epo) was reported to be safe and efficacious in a proof-of-concept study 20. A phase II/III study (522 patients) was negative and showed a higher death rate and complications in patients receiving Epo; possible interaction with rTPA was cited as a likely cause of increased mortality 21. Intravenous granulocyte colony stimulating factor (G-CSF) has also been investigated in a dose escalation phase II a study 22 (AXIS: 44 subjects, drug administered within 12 hours). The authors reported good tolerability and suggest further investigation.
Cerebrolysin, a peptide-based rug is another candidate with potential for approval to be used as a restorative agent. Multiple laboratories have demonstrated the safety and efficacy of this drug in the treatment of experimental stroke. Cerebrolysin, is another potential agent used as a restorative agent, which is a peptide-based rug used in multiple laboratories studying its safety and efficacy in the treatment of experimental stroke. This drug induces neurogenesis and angiogenesis in animal models of stroke and concomitantly enhances brain plasticity and recovery from stroke.
Clinical trials on autologous bone marrow derived stem cells therapy in chronic stroke
This unblinded, non randomized case control study dealt with the safety and efficacy of intravenous autologous bone marrow derived mononuclear and culture expanded mesenchymal stem cells in stroke 17. Adult patients were recruited with the inclusion criteria as: 3 months to 2 years after stroke,
power of hand muscles of at least 2;
Brunnstrom stage 2-5;
NIHSS of 4-15, conscious and cooperative with assessments done for strength, tone (modified Ashworth),
Fugl Meyer (FM) scale for upper limb, Edinburgh handedness inventory, modified Barthel Index (mBI) and functional MRI including DTI was performed at baseline, 8 and 24 weeks of stem cell infusion. Patients were screened and educated about stem cells and bone marrow aspiration technique prior to stem cell infusion 23. Forty stroke patients were recruited with the above inclusion criteria. Twenty were given stem cells followed by 8 weeks of physiotherapy, serving as experimental/stem cell group and 20 patients were administered physiotherapy regime alone. 50 \-60 million cells in 250 ml of saline was infused intravenously over 2-3 hours. The baseline clinical and radiological scores between the experimental and control groups were statistically insignificant. The safety profile was normal with no mortality or cell related adverse reactions in stem cell patients. On comparison between experimental and control groups, mBI was statistically significant on follow up at 24 weeks (p = 0.05). Laterality Index (LI) of BA 4 and BA 6 was insignificant at 8 and 24 weeks follow up, as also in the FA ratio, fiber length and fiber number ratio between the two groups. An increased number of cluster activation in Brodmann areas BA 4, BA 6 was observed post stem cell infusion indicating neural plasticity. The study was conclusive for safety and feasibility of intravenous autologous stem cell infusion 24,25. Stem cells may act as “scaffolds” for neural transplantation and may aid in repair mechanism 26.
Enhancing recovery with special reference to walking and aphasia after stroke Motor weakness and the inability to walk have been the primary targets for testing interventions that may improve after stroke. Physical therapeutic interventions enhance recovery after stroke; however, the timing, duration and type of intervention require clarification and further trials.
Pharmacotherapy, in articular with dopaminergic and selective serotonin-reuptake nhibitors, shows promise in enhancing motor recovery after stroke; however, further large scale trials are required 27.
The complex activity of walking requires the integration of sensory, visual, perceptual and cognitive inputs 28. Many varied strategies and techniques are undergoing assessment including pharmacological therapy for aphasia, transcranial magnetic stimulation for motor recovery and cognitive rehabilitation for attention deficits 29. It is possible that when used in combination these techniques may be symbiotic and synergistic. Much of the research in the area of stroke has focused on recovery of walking.
Walking is a basic human function, often affected by stroke, more easily observed, more easily measured and potentially more easily rehabilitated than other functional deficits 30. Besides loss of power in lower limb, walking also relies on the integrity of the trunk for balance, and the upper extremity for associated walking movements.
Currently the only pharmacological agent that has been shown to alter the natural history and recovery after stroke is issue plasminogen activator given within 4.5 hours after stroke onset. However, a novel era in pharmacotherapeutics for stroke recovery may be in the horizon. Another study 31 randomized patients of severe traumatic brain injury (4-16 weeks) to amantadine (for 4 weeks), or placebo and then assessed at 6 eeks. It was observed that Amantadine, a dopamine agonist increased the speed of recovery during the active treatment phase. Disability Rating Scale (DRS) between baseline and at 6 eeks was similar in both groups, a post hoc analysis at the end f 4 weeks showed that more patients on amantadine had an improvement in their Disability Rating Scale scores.
Dopaminergic agents and selective serotonin-reuptake nhibitors (SSRIs) are known in the in altering the natural history f recovery after stroke 32. Dopamine is a neurotransmitter that may promote neuroplasticity in the cerebral cortex through chemas in brain, via memory and learning principles 33,34 A ingle oral dose of 100 mg of levodopa and 25 mg of carbidopa an enhance the ability of patients with chronic stroke to ncode an elementary motor function. Scheidtmann et al. 35
randomized patients (3 weeks and 6 months post stroke) to ither 3 weeks of 100 mg of levodopa with carbidopa or placebo aily. Patients receiving levodopa had significant improvement n motor recovery and independent ambulation. Subsequent mall studies using levodopa with or without methylphenidate 36 or levodopa with or without amphetamine 37 could ot show a difference in motor recovery or improvement in unctional outcomes with treatment. An ongoing study which ommenced in 2010, has enrolled 572 patients are to receive 100 g of levodopa and 25 mg of carbidopa, or placebo, 1 hour before hysiotherapy. The primary outcome will assess the number of atients walking independently at 8 weeks after randomization.
Animal studies suggest that SSRIs may be involved in eurogenesis and activation of cortical motor areas modulating euronal plasticity 38. These drugs are essential in maintaining leep rhythm, and neurotransmitters levels within the brain and ave been tried in stroke rehabilitation trials. A single dose of italopram can normalize the balance in cortical excitability, as easured by transmagnetic stimulation. Patients more than 6 onths after stroke, in a single dose cross over experiment with italopram, showed improvement in hand dexterity as measured y the nine-hole peg test 39. A single dose of fluoxetine given to atients, 2 to 3 weeks after stroke showed improved motor skills n the none-hole peg test, and increased activation of the affected ide on functional resonance imaging 40.
Chollet et al. 41 randomized 118 acute ischemic stroke atients (5-10 days of event) into two arms: one group was dministered with fluoxetine (20 mg/day by mouth) and another roup placebo. Patients were assessed using the Fugl-Meyer otor scale (motor score varies from 0 to 100, 66 points upper imb, 34 points lower limb; movements measured as none, artial or full) at the end of three months (90 days). The mean mprovement in the total Fugl-Meyer motor scale and functional independence measure from baseline to 90 days was significantly higher in those patients treated with fluoxetine. A recent metaanalysis of randomized controlled trials that recruited stroke patients treated with an SSRI compared to usual care or sham identified 52 trials for analysis. The use of SSRIs is associated with an improvement in functionality, disability status, neurological impairment and depression; more large randomized trials are needed to derive definitive conclusions 42.
Amphetamines and motor rehabilitation
Amphetamines are potent CNS stimulators of phenethylamine class which increase biogenic amines acting as excitatory neurotransmitter. Robust animal and human literature suggest that amphetamines coupled with physiotherapy aid in functional recovery via modulation of noradrenergic system. Brain is malleable to external and internal inputs, which has been credence through various reports. Changes in catecholaminergic, particularly nor epinephrine, functioning after brain injury have been correlated with changes in the rate of recovery after injury 43. Another trial reported that a single dose of AMPH given first day of treatment initiated 10 days after cortical infarct facilitated the rate of recovery (AMPH 68%) compared to saline (27%) treated animals. The cochraine review 44 of amphetamines off late has suggested that 10 trials with 106 stroke patients underwent AMPH therapy and it was found that AM PH did not prove to be beneficial in reducing mortality (Pero OR 1.5, 95% CI0.6 to 3.3). Other 6 studies suggested that there was an evidence of a better relative change from baseline to follow up in motor function (WMD\- 6.1 points, 95% CI \-10.4 to \-1.9). Schuster et al 2011 have recently reported increased performance in ADL and arm function in 8 patients who were administered with 10 mg of AMPH per day 45.
Neurorestorative Therapy using Pharmacotherapy: Is there a Hope?
Is pharmacological restorative therapy post stroke merely a chimera? A perusal of clinical trials of neurorestorative agents certainly seems depressing at first glance. Nevertheless, if experimental evidence of neurorestoration is definite, why then has it not been replicated in clinical domains?
Translating restorative agents from bench to bed has to be performed with caution and care, as the failure is evidenced from clinical trials on several previous occasions. For eg; erythropoietin (EPO) demonstrated in potent therapeutic benefits in multiple clinical studies for the treatment of stroke, and appeared to be a strong candidate for translational research. The phase III clinical trial was terminated because of high mortality and adverse events. Of the stroke patients in the reported trial, 63.4% were administered rTPA, EPO was not tested in the laboratory in conjunction with rTPA. Another subsequent study clearly demonstrated adverse events in animals when treated with combination of EPO with rTPA which was observed in the clinicaltrial.
Criticisms of animal studies include the following
1) Small sample size (underpowered), 2) Lack of randomization, 3) Variable injury levels, 4) Inter-species variations, 5) Confounding variables (hypothermia, use of anesthetic agents), 6) Lack of evaluation of the dose-response relationship and side-effects (therapeutic index), 7) Inadequate outcome measures or biomarker end-points and 8) Flawed statistical analysis. On the basis of these observations, the Stroke Therapy Academic Industry Roundtable (STAIR) recommendations were developed for providing a stronger preclinical database for potential therapeutic agents.
Biomarkers of Restorative Therapy Induced Stroke Recovery
A biomarker is an indicator of disease state that is useful clinically as a substitute measure, reflecting underlying molecular/cellular events that are difficult to measure directly 46. A relevant biomarker for stroke recovery is the one that reflects a brain event relates to recovery and that correlates with behavioral state. Neurorestoration is a concept that has been proven emphatically in several experimental models of stroke. The lack of proof in clinical settings will continue to be discouraging until the reasons for failure in this endeavor are examined. The trials of the past cannot be termed as failures as they definitely have contributed to our understanding of the complex biology of brain injury. This knowledge must provide an impetus for the development of superior candidate molecules and methodological interventions that will enhance drug development as well as clinical testing.
![]()
From: https://journals.sagepub.com/doi/full/10.1177/0963689717714102
Traumatic Brain Injury: Current Treatment Strategies and Future Endeavors
Amantadine
Amantadine is a dopamine agonist used for Parkinson’s disease. Amantadine can distribute in frontal lobes and acts as an N-methyl-D-Aspartate (NMDA) receptor antagonist. It has been proposed that amantadine may protect the neurons against glutamate excitotoxicity in the acute phase of TBI. Many studies have demonstrated that amantadine in dose of 100–400 mg/d may increase the arousal and improve cognitive function when given within 12 wk after the TBI.37,42
Erythropoietin (EPO)
EPO is a secreted glycoprotein with a molecular weight of 30-kD. The role of EPO in the regulation of erythropoiesis has been initially identified in the hematopoietic system.43 EPO may also play a role in the central nervous system as the expression of both EPO and its receptor, EpoR, are widespread in the brain.44,45
Although the molecular weight of EPO is larger than the molecular threshold of the BBB, exogenous EPO has been found in the brain parenchyma where it may play a role in neuroprotection after brain injury.46Several studies have demonstrated that EPO shows antiexcitotoxic, antioxidant, antiedematous, and antiinflammatory effects in TBI.47–50 Brain injury causes upregulation of EpoR expression.45 Reduced number of neural progenitor cells (NPCs) and increased apoptosis has been found in the mice lacking the EPO receptor.51
EPO/EpoR signal pathway has been shown to be involved in neuroprotection in pathological conditions.50,52Expression of the receptors for EPO is significantly increased in neurons, glia, and endothelial cells after TBI.41 EPO appears to promote neuroprotection through binding to EpoR and activating JAK-2/NF-kB and PI3K signaling pathway.41,53 Additionally, JAK-2 phosphorylation activates PI3K/AKT and Ras/MAPK pathways and promotes STAT-5 homodimerization, which has been shown to have antiapoptotic and neurotrophic effects.54–56 However, a recent double-blind randomized controlled clinical trial has revealed that EPO does not reduce the number of patients with severe neurological dysfunction and that the effect of EPO on mortality remains uncertain in moderate or severe TBI.57 Clearly, more clinical trials need to be performed to confirm the results collected from the experimental studies.
S100B protein
S100B protein is a calcium-binding protein produced by glial cells. S100B protein has been detected in serum after the opening of the BBB after brain injury. S100B shows a dose-dependent dual effect in neurons. In small doses, S100B acts as a neurotrophic factor for neuroprotection. However, in high doses, S100B increases neuroinflammation and worsens the neural survival.41
Hypothermia
In 1945, Fay reported possible benefits of hypothermia on severe cerebral trauma.58 Since then, many studies have shown that hypothermia improves outcome in animal models of TBI.59–64 Temperature management in the brain is very important after cerebral injury.65,66 Deep hypothermia (below 30 °C) appears to show no benefits for TBI while mild to moderate hypothermia (32 to 35 °C) displays neuroprotective effects.67,68 However, the neuroprotective mechanisms of hypothermia after TBI remain poorly understood. Several beneficial effects of hypothermia have been determined, including the effects on regulation of metabolism, excitotoxicity, inflammatory mediators, or autophagy.68–74 Neuroprotective effects of hypothermia have been proposed to be associated with the reduction of brain oxygen consumption and glucose metabolic rate, preservation of high-energy phosphate compounds, and maintaining of tissue pH in the brain.75 Recent studies have shown that therapeutic hypothermia significantly alters genomic transcripts and microRNA responses and regulates protein synthesis and translation in rat models of TBI.76–78 The hypothermia-induced changes in gene, microRNA, and protein responses following TBI may target the delayed responses that regulate the secondary brain damage. Although the robust neuroprotective effects of therapeutic cooling have been demonstrated in animal models of TBI, it still remains controversial whether hypothermia treatment could really provide permanent protection or delay the injury processes.69
DC
DC is a neurosurgical procedure, which allows a swelling brain to expand without being compressed. DC has been used to reduce ICP in the conditions of brain tumor, stroke, and severe TBI.79 DC as a treatment of TBI was originally reported by Emil Theodor Kocher.80 However, due to the controversial findings in both clinical and experimental studies, DC is recommended as a third-tier therapy for the treatment of elevated ICP by most national and international guidelines.80,81 The role of DC on brain edema formation and secondary injury after TBI has been examined in animal models of TBI. Using a controlled cortical impact model of TBI in mice, Zweckberger and coworkers reported that early craniectomy prevented secondary brain damage and significantly reduced brain edema formation.82 A recent study suggested that DC might affect AQP4 expression and reduce brain edema formation after TBI.83 However, Szczygielski and coworkers reported opposite findings. They found that surgical decompression promoted brain edema formation and contusional blossoming and exacerbated functional impairments in mice with closed head injury.84 The different results may be attributed to different injury severity from different TBI models. The outcomes of craniectomy application are highly correlated with the severity of the initial injury.79 Although the results of experimental studies are controversial, DC still exhibits an important role to save the lives of patients with TBI and improve neural functional outcomes. Further studies need to be performed to confirm which kind of TBI is suitable for DC and which physiological and pathological mechanisms are related to functional outcomes after DC in TBI patients.
Neurovascular Regeneration
Neuronal and vascular regeneration have been proposed to play a role in brain recovery after brain injury. Neurogenesis in adult brain has been shown to occur in the subgranular zone in the dentate gyrus (DG) of the hippocampus and subventricular zone. In animal models, it has been described that TBI induces the neurogenesis in cerebral cortex, DG, and CA3. Thymosin β 4 (Tβ4) is an important G-actin-sequestering molecule in cells. In animal models, Tβ4 injection increases proliferation of NPCs. Moreover, Tβ4 also enhances angiogenesis and promotes NPC differentiation.35
In the subventricular zone and subgranular zone, there is a particular group of astrocytes that can go through division and differentiation into new neurons. These newborn neurons have been proposed to play a role in replacing the neurons in the olfactory bulb or in the cortex and hippocampus after TBI. In animal models, it has been shown that the number of regenerated neurons in young animals is greater than those of aged animals. The process of NPC proliferation and differentiation has a peak at 2 to 5 d after TBI, while some studies extend this time frame to 14 d.85
TBI causes changes in vascular density in the cortex, DG, and CA3 in animal models. Tβ4 treatment increases the vascular density in the cortex, DG, and CA3. This increased vascular density is associated with neurogenesis and synaptogenesis. The entire process of angiogenesis, neurogenesis, and synaptogenesis may contribute to TBI recovery.35 Recently, Zhang et al.86 reported that a Tβ4 active peptide fragment, N-acetyl-seryl-aspartyl-lysyl-proline (AcSDKP), enhanced angiogenesis and neurogenesis, and increased the number of dendritic spines in the injured brain.
S100B appears to be a stimulator for neurogenesis after TBI. Using animal models of TBI, a number of studies have shown that intraventricular administration of S100B in the acute or subacute phase of TBI promotes neurogenesis in the hippocampus and subventricular area and improves cognitive function and spatial learning.41,87 It has been shown that nitric oxide enhances neurogenesis and angiogenesis through the mediation of guanylyl cyclase and formation of guanylate cyclase.88 Induced neurovascular regeneration lays the foundations for neural plasticity and functional recovery.
Neurorestoration
Cell-based therapy for TBI recovery
In the past few decades, stem cell-based therapy opened a new therapeutic avenue for neurological disorders and Central Nervous System (CNS) injuries. Preclinical studies utilizing stem cells and progenitor cells as treatment for spinal cord injury,89–91 stroke,92,93 and brain injury94,95 have shown beneficial effects in improving recovery. Currently, different cell types have been used as putative therapies for TBI recovery. It has been revealed that enhancing neurogenesis, angiogenesis, and immunoregulation by secreting chemokine and growth factors are involved in the functional recovery induced by stem cell/progenitor cell-based interventions.96–99 Several clinical trials in cell-based treatment for TBI recovery have demonstrated safety of this therapeutic approach.100,101 However, the administration route, dose, and time window still remain controversial.
The therapeutic effects of mesenchymal stem cell (MSC) transplantation in TBI recovery have been demonstrated in animal models. MSCs were mainly isolated from the bone marrow, umbilical cord, and adipose tissue.99,101,102 The administration dose of MSCs ranges from 0.1 to 20 million cells per kg body weight.96 The approaches of lateral ventricle and intravenous injection have been utilized.96 The timing for MSC transplantation in experimental animal models has been intensively studied within 24 h after TBI. Recently, a clinical study has showed significant improvements in neurological function of patients with sequelae of TBI after umbilical cord MSC transplantation.101 Although it remains to be fully understood how MSCs transplantation improves functional recovery after TBI, emerging evidence has suggested that neurorestoration is most likely the mechanism underlying the MSCs transplantation-induced TBI recovery rather than neuroreplacement. It has been shown that MSCs release growth factors such as Fibroblast growth factor 2 (FGF-2), Vascular endothelial growth factor (VEGF), Brain-derived neurotrophic factor (BDNF). These growth factors enhance neurogenesis, angiogenesis, and synaptogenesis.41,103 The efficacy of MSCs transplantation in the acute phase of TBI is contradictory. Extensive studies are needed to further validate the therapeutic effects of MSCs transplantation in the acute phase of TBI in animal models before this approach is translated into clinical trials.
Neural stem cells (NSCs)/NPCs are also most frequently used in experimental TBI. NSCs/NPCs reside in the mammalian brain at the ependymal lining, subventricular zone, and hippocampus.104 Recently, promoting endogenous NSCs or NPCs proliferation and differentiation have been shown to stabilize the cortical microenvironment and enhance post-TBI functional recovery.105–108 Exogenous NSC transplantation also promotes neuroprotection, enhances hippocampal neurogenesis, and improves functional outcomes.109 In animal models, the number of cells for transplantation ranges from 0.15 to 25 million cells per kg body weight.96 The most common delivery method used for NSC transplantation is stereotactic injection to the brain. Although the timing for transplantation ranges from immediately after TBI to a few weeks later,110–112Shear et al.113 reported that NSC transplantation at 2 d after TBI showed better outcome than at 2 wk after TBI. It has been shown that the benefits of NSC/NPC transplantation may attribute to differentiating into functional neurons and replacing lost neurons.114,115 Recent studies have shed new light on the interaction between NSCs/NPCs and immune system. The cross-talk between immune cells and transplanted NSCs/NPCs not only enhances endogenous regenerative responses, but it also promotes functional integration of grafted NSCs/NPCs.116 Gao et al. reported that grafted human NSCs promoted the switch of microglia/macrophages into an anti-inflammation phenotype which may contribute to stem cell-mediated neuroprotective effects after severe TBI in mice.117 Although there is no clinical trial concerning NSC transplantation for TBI recovery, the clinical study in traumatic cervical spinal cord injury has shown the safe outcomes.118
Transplantation of embryonic stem cells (ESCs) in TBI has also been studied. Molcanyi et al.119 reported that post-traumatic inflammatory response inhibited the survival and integration of transplanted ESCs after TBI. Riess et al.120 revealed that ESC transplantation improved neurological outcomes but it had the risk of tumorigenesis.
Although preclinical studies indicate stem cell-based interventions may be a promising approach for TBI, long-term risks and benefits of this approach still need to be further investigated.
Enriched environment (EE) intervention for TBI recovery
Neurorehabilitation plays a crucial role in integrating TBI patients into a functional lifestyle. TBI survivors are often left with long-term depression. Exposure to positive environments plays a significant role in improving emotional well-being for TBI patients.
Numerous studies have examined the effects of exposing animals to EEs after neurological insults. An EE consists of housing animals in a larger cage and allowing animals to have more opportunities for social interaction, sensory stimulation, and exploratory behavior.121 Rats exposed to an EE have shown benefits in both neurobehavior and neuroanatomy.121–131 Using animal models of TBI, multimodal interventions including exposure to an EE have yielded positive results.132,133 It has been shown that EE exposure improves spatial memory recovery after cerebral ischemia.134 In olfactory bulbectomized rats, exposure to an EE results in antidepressant effects.135 In rats with striatal lesion, EE has also proven beneficial for neural graft function and morphology.136 It has also been reported that visually defected rats may regain some degree of visual acuity after exposure to an EE.17 The prophylactic effects of EE exposure prior to undergoing a TBI has also shown positive results.137 Spinal cord-injured rats also display functional recovery once exposed to an EE.126
Translating the research on EEs to the clinical arena in humans has significantly positive implications in neurorehabilitation. Individuals sustaining TBIs are known to have a high incidence of depression. EE intervention plays a key role in rehabilitative motivation for the individuals.
Conclusive Remarks
Although there is lack of effective treatment for TBI recovery today, the efforts for developing therapeutic strategies on TBI recovery have been continuously made over the past several decades. Standard medical and surgical interventions always play a significant role in the acute management for TBI patients. Given increased population of TBI survivors due to the advent of better acute management guidelines in the acute phase of TBI, the number of TBI survivors with various disabilities has risen. This calls for major research of TBI to be shifted into the area of neurorestoration and neurorehabilitation.
Traumatic brain injury (TBI) is commonly defined as an insult to the brain from an external force that causes temporary or permanent impairment in functional, psychosocial, or physical abilities.1 It is a significant cause of morbidity and mortality, and the leading cause of death and disability among young adults.
Common causes of TBI include motor vehicle accidents, falls, sports injuries, and violence,1 and it is recognized increasingly in war zone injury.2 In the US, approximately 2 million people will sustain a TBI each year, one-quarter of whom will require hospitalization, leading to a conservative estimate of direct and indirect costs of $50 billion to $100 billion annually.3
With advances in the management of head trauma, an increasing number of patients are surviving with residual neurological impairments. A National Institute of Health panel estimates that 2.5 to 6.5 million Americans currently live with TBI-related disabilities.4
The effective treatment of TBI requires input from multiple disciplines and professions starting at the time of injury and continuing through the rehabilitation phase.
Despite the prevalence and cost of TBI-related disabilities there is a paucity of literature reviewing modern approaches to pharmacotherapy. There is, however, growing evidence that medications may speed recovery by enhancing some neurological functions without impacting others.
Pharmacotherapy is increasingly being used in both the subacute (less than 1 month post-TBI) and chronic (more than 1 month post-TBI) phases.
Disabilities arising from TBI that have a direct impact on functioning and rehabilitative potential can be broadly classified into four main categories: decreased level of consciousness (LOC), and neuropsychiatric, neurocognitive, and neurobehavioral sequelae.5-8 Decreased level of consciousness refers to a diverse range of clinical states including coma, vegetative states, akinetic mutism, and locked-in states.
Neuropsychiatric symptoms may present as mood disorders, posttraumatic stress disorder, and personality changes characterized by disinhibition and egocentricity. Neurocognitive injuries vary, but most frequently involve impaired attention, memory, and executive functioning.
Neurobehavioral deficits distinct from neuropsychiatric sequelae may take the form of irritability, hyperexcitability, nervousness, disinhibition, poor impulse control, restlessness, and aggression, with aggression and agitation seen in as many as 30% of brain-injured patients.5-8
Depending on the location of injury, damage can occur to a variety of neurotransmitter networks critical to cognitive processes. Investigation has focused on the loss of dopaminergic neurons that regulate executive functioning, as well as deficits in norepinephrine and acetylcholine, which limit attention—a critical function for effective rehabilitation.9
Fortunately, a number of pharmacological interventions show promise in helping patients cope with these losses and deficits.
Although insufficient evidence exists to establish guidelines for optimal pharmocotherapy, medications may be used to support recovery. Examples are shown in the accompanying Table, which summarizes the pharmacological approaches discussed in more detail below.
When problematic TBI symptoms are identified, clinicians can use this information to determine pharmacological options and integrate them with nonpharmacological options such as physical therapy, occupational therapy, physiatry, and the patient’s support network.
Planning a pharmacological intervention strategy
The decision to use pharmacological intervention should be the result of multidisciplinary collaboration and made with the patient or his or her substitute decision maker. Goals of therapy should be clarified, and outcomes and adverse events should be reliably tracked, particularly so medications that are ineffective or cause adverse events can be discontinued and unnecessary polypharmacy can be avoided.
Selecting the most appropriate agent requires careful analysis of the neurological disabilities present, the nature of the underlying lesion, and the time elapsed since the injury.
Psychostimulants
Psychostimulants such as methylphenidate are most commonly used to treat attention deficit hyperactivity disorder (ADHD), a condition that involves problems with executive functioning and can be characterized as similar to brain injury both in terms of symptoms and neurotransmitter aberrations.10
Although the complete mechanism of action of methylphenidate remains unknown, this agent is thought to bind dopamine transporters, thereby blocking reuptake and increasing extracellular dopamine levels, particularly in the frontal cortex.11 It is also thought to increase norepinephrine and serotonin levels.
In the majority of studies, methylphenidate has been administered twice daily, either at a fixed dose of 10 to 15 mg or at a dose of 0.3 mg/kg.12-15
In the acute phase after a TBI, methylphenidate-treated patients demonstrated better attention, concentration, and performance on motor memory tasks at 1 month, but these benefits did not persist at 3 months. Thus, it has been suggested that while methylphenidate may shorten recovery time, it does not change morbidity.12
In the chronic phase after a TBI, patients have reported improvements in mood, work performance, and alertness, with more limited evidence suggesting an improvement of fluency and selective attention.
The impact of methylphenidate on chronic attention is more ambiguous: one study suggests improvement in long-term processing speed and attention to tasks but not increased sustained attention or decreased susceptibility to distraction.12
Two separate studies have suggested methylphenidate is effective in the treatment of agitation and seizures,16,17 while another demonstrated no neurobehavioral benefit.18
Despite the accumulation of controlled clinical trials, there is no consensus on the use of stimulants in treating TBI-induced impairments in arousal and motor activity.
It should be noted that one recent review concluded “at present there is insufficient evidence to support routine use of methylphenidate or other amphetamines to promote recovery from TBI,”19 while another review noted that at least 10 clinical trials have demonstrated a role for methylphenidate in both adult and pediatric brain injury patients suffering from neurocognitive deficits, particularly in attention, memory, cognitive processing, and speech.20
Methylphenidate has a quick onset of action and relatively benign side effect profile, and we believe it to be useful in both the acute and chronic phase of TBI.
Antidepressants
Despite potentially severe consequences, post-TBI psychiatric sequelae are underdiagnosed and undertreated. Fortunately, current evidence suggests that antidepressants can be used to manage both neuropsychiatric and additional neurological deficits persisting from brain injury.
Selective serotonin reuptake inhibitors (SSRIs) have been found useful in treating behavioral syndromes in TBI patients, particularly in the subacute stages of recovery21 but also in chronic settings.
The majority of studies suggest that SSRIs improve neurobehavioral, neurocognitive, and neuropsychiatric deficits, specifically agitation, depression, psychomotor retardation, and recent memory loss; however, most data originates from nonrandomized trials.
Sertraline administered at an average dose of 100 mg daily for 8 weeks has been found to be beneficial for agitation, depressed mood, and deficits in psychomotor speed and recent memory; shorter treatment durations have demonstrated no benefit.21
Similarly, 60 mg daily of fluoxetine for 3 months was shown to be effective in the treatment of obsessive-compulsive disorder caused by brain injury.22 Finally, paroxetine or citalopram, at a dose of 10 to 40 mg daily, was shown by another study to be equally effective in the treatment of pathological crying.23 None of the reviewed studies addressed neurocognitive deficits.
The highest concentration of serotonergic and adrenergic fibres is located near the frontal lobes, the most common site of traumatic contusion.24
Consequently, these fibres are commonly injured in TBI, suggesting that newer antidepressants with effects on both norepinephrine and serotonin, such as mirtazapine and venlafaxine, may also be effective in the treatment of TBI sequelae; however, clinical data with these agents in TBI is lacking.
Similarly, bupropion increases both dopamine and norepinephrine levels and is a weak inhibitor of serotonin reuptake. At 150 mg daily, this agent has been useful in treating restlessness.25
Antiparkinsonian drugs
The antiparkinsonian drugs amantadine, bromocriptine, and levodopa combined with carbidopa (e.g., Sinemet) have varied mechanisms of action, but all ultimately serve to increase dopamine levels in the brain.
Amantadine acts presynaptically to enhance dopamine release or inhibit its reuptake, and can act postsynaptically to increase the number, or alter the configuration of, dopamine receptors.26 It is also a noncompetitive NMDA receptor antagonist and may provide protection against possible glutamate-mediated excitotoxicity in the context of TBI.27
Bromocriptine is a dopamine receptor agonist affecting primarily D2 receptors and to a lesser extent D1 receptors.28 The use of levodopa and carbidopa in combination directly increases dopamine levels: levodopa becomes dopamine once decarboxylated, while carbidopa inhibits L-amino decarboxylase, allowing levodopa to reach the central nervous system.28
Multiple studies of amantadine at a dose of 100 to 300 mg daily have suggested its effectiveness in both the acute and chronic care phases after TBI, particularly in diffuse, frontal, or right-sided brain injury.
Currently, the evidence suggests neurocognitive or neurobehavioral deficits, particularly cognition difficulties and agitation, are primary indications for amantadine use.26,29,30
Amantadine-treated patients demonstrated improvements in motivation; decreased level of apathy; increased attention, concentration, and alertness; improved executive functioning; decreased processing time; reduced agitation, distractibility, fatigue, aggression, and anxiety.
In addition, patients treated with amantadine demonstrated changes in outcome LOC, specifically improved arousal and LOC as measured by the Glasgow Coma Scale. Interestingly, one study also suggested decreased mortality.31 To date, no study has shown an improvement in memory.
Three case reports using 5 to 45 mg of bromocriptine daily,32 and one study using a combination of 100 mg of bromocriptine with 100 mg of ephedrine,33 showed improvement in akinetic mutism, while another study using 5 mg of bromocriptine combined with sensory stimulation led to improvements in patients with vegetative or minimal consciousness.34
The evidence is similarly limited for levidopa and carbidopa medications where nonrandomized studies suggest that they might be useful in the chronic phase of TBI with diffuse injury and persistent vegetative state.35
Combining agents has also been tried in one study that found improvements in neuropsychiatric deficits with the daily administration of 25 mg/200 mg of levodopa/carbidopa three times daily, 250 mg of amantadine, and 5 mg of bromocriptine twice daily.36
Anticonvulsants
Anticonvulsants have been used with varying results for treating symptoms of TBI. Valproic acid, for example, enhances inhibitory control mediated by the neurotransmitter GABA, thereby promoting general central nervous system stabilization, but findings thus far have been mixed.
Investigations utilizing 600 to 2250 mg of valproic acid daily (resulting in serum levels of 40 to 100 µg/mL), have demonstrated positive neurocognitive effects, including improved recent memory and problem-solving, as well as ameliorating neuropsychiatric and neurobehavioral symptoms such as depression, mania, destructive and aggressive behavior, restlessness, disinhibition, impulsivity, lability, and alertness.37-41
Conversely, one controlled trial found valproic acid negatively impacted decision-making speed, and another suggested an increased mortality rate with valproic acid use.37-41
Other agents
Modafinil is a vigilance-promoting drug commonly used to treat narcolepsy and idiopathic hypersomnia, illnesses that can present with symptoms similar to those seen in TBI: excessive daytime sleepiness, inattention, and decreased ability to perform social activities.
The precise mechanism of action remains unknown, although it is believed that modafinil can inhibit GABA or increase glutamate levels in the nondopaminergic anterior hypothalamus, hippocampus, and amygdale.42,43
Two studies that investigated the role of modafinil in chronic TBI showed an improvement in neurocognitive deficits, specifically memory and attention, as well as improving daytime somnolence at doses between 100 and 400 mg.44,45
Four randomized control trials examining the use of beta-blockers, specifically propranolol and pindolol, have demonstrated beneficial effects on neurobehavioral symptoms of aggression and agitation in both the chronic and subacute phase. This class of drugs deserves further attention for the management of both neuropsychiatric and neurobehavioral sequelae of TBI.46
Neuroleptics are being used increasingly in the setting of delirium, and one might consider using them in an attempt to allow the brain to recalibrate neurotransmitter levels. However, it should be noted that there is some evidence that dopamine blockade may negatively affect recovery.47,48
There are also a number of animal studies examining drugs that have the potential to adversely affect brain recovery following TBI. These studies typically use a stroke model, so generalizing to TBI may not be possible.
Nevertheless, the evidence currently does not support the use of neuroleptics, benzodiazepines, phenytoin, prazosin, trazodone, and similar agents because of their potential adverse effect on recovery, presumably through the impacts they have on neurotransmitters such as dopamine, norepinephrine, or GABA.49-51
Preliminary evidence suggests cholinesterase inhibitors such as donepezil may improve long-term cognitive outcomes, particularly in domains such as memory and attention when administered early, and further investigation with these agents is also warranted.52,53
Finally, antiandrogenic medications, such as estrogen and medroxyprogesterone, may have a role to play in reducing inappropriate sexual behavior in patients with TBI. In a case study and one small trial, these drugs demonstrated effectiveness.54
Summary
The nature of TBI sequelae, whether psychiatric, cognitive, or behavioral, is poorly understood. Likewise, the use of pharmacological interventions to improve symptoms, function, and outcome is still under development.
There are, however, a number of agents that inspire optimism. When treating neurological deficits medically, there is evidence to support the tailored use of these agents for particular TBI clinical scenarios. The timing and nature of symptoms, along with whether agents are administered in the acute or chronic phase after TBI, are all relevant factors for determining proper use.
With insufficient evidence to establish guidelines for optimal treatment, care must be taken when choosing pharmacological interventions for TBI.
If the decision is made to use medications to promote TBI recovery or treat its attendant disabilities, clinicians should thoroughly document the goals of pharmacotherapy and closely monitor for side effects. Future studies
will undoubtedly add to the clinician’s armamentarium for the care of TBI patients.
![]()
Hello Dr Nandipati, thank you for reading the links and your reply. I understand your concern regarding possible side effects of various medicines, and in focusing on the most relevant symptoms in order - of which post stroke apathy the primary concern.
As you suggested (and as she is already taking Venlafaxine and well tollerating it), it appears at first advisable to increase the dosage of Venlafaxine (to perhaps 100-175mg - by less than 75mg increments over 4 day periods) from her current 75mg, as to help with post stroke apathy. As you know, she takes Venlafaxine for anxiety and depression - there is a history of depression in my family (including my grandmother, my eldest sister, my mother and myself), and had been taking it previous to her Subarachnoid Hemmorhage.
Now, after the stroke her depressive/anxious states seem well contained by the Venlafaxine. What is new from the post stroke damage is presentation of apathy, not of a depressive type, but one seemingly specific to conditions of post stroke/post head injury.
For instance, patients experiencing minor depression/Dysthemia/major depression do not want to get off the couch and are experiencing both flat/devoid states as well as negative emotions and thoughts.
In post stroke apathy, as in the case of my mother, patients are content and she agrees to all manner of things and wants to do things, makes goals, enjoys outings and also staying in readingtvyada) yet the cognitive and executive function are different and describe. same with my chooseto thi yet lack both fog and etc.
From this qualitative/empirical/experiential observations of my mother, as well as my own experiences with anxiety/mood disorders (both pre and post head injury), the type of apathy associated with depression appears to differ from post stroke (asnd post head injury) apathy (and other chronic changes of 'character' that can occur resultant of stroke).
These are not only qualitatively different, but evidence points to to differing etiologies, structural differences between these two 'apathies' (perhaps post stroke apathy can be renamed to something more suiting).
Approximately 30% of patients exhibiting changes in executive function, cognition and 'mental states' (mood/anxiety disorders and other character changes) in post brain injury (stroke/p-TBI, etc.) and are often prescribed psychiatric/psychotropic pharmaceuticals (Venlafaxine being one of them) for such.
As you know there are no pharmaceutical agents prescribed for (post) brain injuries such as stroke, head trauma etc. itself, (nor for post stroke apathy specifically). No effective medication-mediated intervention to accelerate rehabilitation has been established.
Seeing as she is already on venlafaxine and has been before the injury, and that we were able to identify a qualitatively different kind of apasthy emerge (different by attitude), and different by being tied to changes in executive function (and possibly hypometabolism?), and aside from psychotoprics targeting and altering specific neurotransmiter systems (hence aleviating symptoms) there are no pharmaceutical agents prescribed for (post) brain injuries such as stroke, head trauma etc. itself, nor for post stroke apathy specifically, and that this different kind of apathy appeared while she was taking venlafaxine and continues radically though she is taking Venlafaxine, Venlafaxine does not appear to be helping sufficiently with her post stroke apathy (as it's a different kind of apathy).
Pharmacological research in developing medicinal therapy to treat post stroke conditions/etiologies must include the currently prescribed medicines for more remote neurological conditions such as Parkinsons, Dementia, (and possibly Anti-Convulsant/Seizure/Epileptic medicines as well), as well as other medical fields including Cardiology, Endocrinology, Lymphology, Immunology, Gastroenterology, etc. as stroke affects and is affected by these interconnected/related systems (and areas of discipline/study). It is interesting that many of the drugs that may be helpful for post stroke treatment (some studied for post stroke treatment) are used for these different classes of illness and systems/fields of study. For instance, curreently treated in certain clinics and offices are
Our hope then is in seeking drugs outside of the psychiactric pharmaceutical class, as our experience shows that these drugs (though supremely helpful in addressing anxiety/mood disorders) fail to address the symptoms of head injuries (whether resultant from stroke or head trauma).
This research centers largely on possible medications for treating her display of post stroke apathy following the subarachnoid hemorrhage incident, (and likely secondary damage) this non-depressive post stroke apathy appears to be tied to damage affecting executive function, hippocampus (personality changes) and possibly, metabolic states as well). As no official medicines are prescribed post stroke, many of the treatments detailed in the report are studied with small sample sizes, are offlabel treatment studies or have not been frequently tested.
one that addresses systemized dysfunction executive function, cognition and focus, metabolism boost, attitude, distractability and focus as a whole, and as not doing anything and the side effect risks are low then logical accumuilate boosts, without cheerleader syndrome, but ones we can examine post therpeutic with scans mri and that etc
The only ones available then are offlabel. furthermore of those studied examined most are multifactorial. typically limited by small sample sizes et yet in certain subsets of patients pos effects and sc.
In light of this, and remaining cognizant of the necessity to weigh side effect risks against possible bennificial outcomes, our position in this delicate balance is less conservative and more willing and asking for treatments such as rhopinole. trying a drug with low side effects that doesn't work is better than not trying.
![]()
Amantadine 200mg/day/placebo given in first 6 weeks or 2nd 6 weeks
Diketopiperazines are cyclized dipeptides that were developed through a rational drug design program based on the tripeptide thyrotropin-releasing hormone (TRH) 74. TRH and TRH analogs inhibit multiple secondary injury factors and processes 74. They were shown to be highly neuroprotective in experimental neurotrauma across many laboratories and a small clinical randomized study of TRH in human SCI was promising 75. Four structurally different diketopiperazines demonstrated significant neuroprotective properties both in vitro and in animal TBI studies 76. One of these (35b) showed effectiveness across TBI models and species. In neuronal cell cultures, 35b provided neuroprotection in multiple models of necrotic and apoptotic cell death 77. Intravenous administration of 35b reduced both lesion volume and improved functional recovery after fluid percussion injury (FPI) in rats and CCI in mice 77,78. The therapeutic window was at least 8 hours. Treatment also significantly reduced apoptotic cell death 77. Effects appeared to be pleiotropic, with treatment reducing multiple potential secondary injury factors (cyclins, calpains, cathepsin), while upregulating various endogenous neuroprotective and neurotrophic factors (BDNF, HSP-70, HIF-1) 76,79. In addition, data are available regarding pharmacokinetics, brain penetration after systemic administration and preclinical toxicology in the rat. Similar pleiotropic neuroprotective effects were reported with another diketopiperazine - cyclo-L-glycyl-L
Treatment improved functional recovery and long-term histological outcomes, and reduced caspase-3 mediated apoptosis and microglial activation 80. Given their multipotential neuroprotective effects in experimental TBI models, their clinically relevant therapeutic window, and their safety profile, the diketopiperazines are attractive candidates for further clinical investigation.
In traumatic brain injury (TBI), severe disruptions occur in the choroid plexus (CP)–cerebrospinal fluid (CSF) nexus that destabilize the nearby hippocampal and subventricular neurogenic regions.
Following invasive and non-invasive injuries to cortex, several adverse sequelae harm the brain interior:
(i) structural damage to CP epithelium that opens the blood–CSF barrier (BCSFB) to protein,
(ii) altered CSF dynamics and intracranial pressure (ICP),
(iii) augmentation of leukocyte traffic across CP into the CSF–brain,
(iv) reduction in CSF sink action and clearance of debris from ventricles, and
(v) less efficient provision of micronutritional and hormonal support for the CNS. However, gradual post-TBI restitution of the injured CP epithelium and ependyma, and CSF homeostatic mechanisms, help to restore subventricular/subgranular neurogenesis and the cognitive abilities diminished by CNS damage. Recovery from TBI is faciltated by upregulated choroidal/ependymal growth factors and neurotrophins, and their secretion into ventricular CSF. There, by an endocrine-like mechanism, CSF bulk flow convects the neuropeptides to target cells in injured cortex for aiding repair processes; and to neurogenic niches for enhancing conversion of stem cells to new neurons. In the recovery from TBI and associated ischemia, the modulating neuropeptides include FGF2, EGF, VEGF, NGF, IGF, GDNF, BDNF, and PACAP. Homeostatic correction of TBI-induced neuropathology can be accelerated or amplified by exogenously boosting the CSF concentration of these growth factors and neurotrophins. Such intraventricular supplementation via the CSF route promotes neural restoration through enhanced neurogenesis, angiogenesis, and neuroprotective effects. CSF translational research presents opportunities that involve CP and ependymal manipulations to expedite recovery from TBI.
Edonerpic maleate, a neural plasticity enhancer, could be a clinically potent small compound with which to accelerate rehabilitation after brain damage.
Dopaminergic agents and selective serotonin-reuptake nhibitors (SSRIs) are known in the in altering the natural history f recovery after stroke 32. Dopamine is a neurotransmitter hat may promote neuroplasticity in the cerebral cortex through chemas in brain, via memory and learning principles 33,34 A ingle oral dose of 100 mg of levodopa and 25 mg of carbidopa an enhance the ability of patients with chronic stroke to ncode an elementary motor function. Scheidtmann et al.
35 randomized patients (3 weeks and 6 months post stroke) to ither 3 weeks of 100 mg of levodopa with carbidopa or placebo aily. Patients receiving levodopa had significant improvement n motor recovery and independent ambulation. Subsequent mall studies using levodopa with or without methylphenidate 36 or levodopa with or without amphetamine 37 could ot show a difference in motor recovery or improvement in unctional outcomes with treatment. An ongoing study which ommenced in 2010, has enrolled 572 patients are to receive 100 g of levodopa and 25 mg of carbidopa, or placebo, 1 hour before hysiotherapy. The primary outcome will assess the number of atients walking independently at 8 weeks after randomization.
In addition, patients treated with amantadine demonstrated changes in outcome LOC, specifically improved arousal and LOC as measured by the Glasgow Coma Scale. Interestingly, one study also suggested decreased mortality.31 To date, no study has shown an improvement in memory.
If the decision is made to use medications to promote TBI recovery or treat its attendant disabilities, clinicians should thoroughly document the goals of pharmacotherapy and closely monitor for side effects. Future studies will undoubtedly add to the clinician’s armamentarium for the care of TBI patients.
Concern with aderol is prescription stimulants increase the risk of adverse cardiovascular events https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3405448
![]()
From: Diagnosing and Treating Apathy in Dementia https://www.caringfortheages.com/article/S1526-4114(18)30291-9/fulltext#cesec40
Potential Treatments
There is no one-size-fits-all approach and no defined guidelines for treatment, Dr. Curtis said. She suggested first ruling out depression and any underlying illnesses, then once apathy is diagnosed, target the source — in this case, dementia. Treatment can involve pharmacologic and nonpharmacologic solutions.
Nonpharmacological treatments have shown poor evidence of success, Dr. Curtis said, but some stimulating activities may be helpful, such as cooking and arts and crafts.
The pharmacological treatments target three neurotransmitters: acetylcholine (ACh), dopamine with and without norepinephrine, and serotonin.
Specifically, in patients with Alzheimer’s dementia, apathy responds best to increased ACh via improved goal-directed behavior. In patients with apathy and other types of dementia, increased ACh improves motor and executive function.
Given the existing data for pharmacologic treatment of apathy, psychostimulants have the most evidence of effectiveness, Dr. Curtis said. Amphetamine/dextroamphetamine (Adderall) and methylphenidate (Ritalin) both increase levels of dopamine and norepinephrine. Modafinil (Provigil), a eugeroic (a class of drugs that promote wakefulness and alertness), may increase dopamine, and it also is thought to inhibit gamma-aminobutyric acid, a neurotransmitter that slows brain activity.
Stimulants allow the release of a burst of neurotransmitters, Dr. Curtis said. How intense and how long that burst lasts will help determine how long a patient with apathy should continue on the medication. “Stimulants have a variable reaction for everyone,” Dr. Curtis said. “If you’re giving a damaged brain stimulants, you’re going to get an even higher range of variable response.”
Using stimulants in the elderly is not without risk, however. Those risks are higher in individuals with uncontrolled hypertension, structural cardiac problems, and myocardial infarction in the previous 6 to 12 months, Dr. Curtis said.
Other pharmacologic options — such as memantine, antipsychotics, antidepressants, and amantadine — also have shown benefit.
Any pharmacologic treatment for apathy should “start low and go slow,” Dr. Curtis said. She recommended an intermediate-release methylphenidate at 5 mg daily or twice daily, with an increase every 1 to 2 weeks until reaching a maximum dosage of 10 mg twice a day.
Treatment of post stroke etiologies include off label usage of medicines assigned to different classes of illness such as Parkinsons medicines, Anti-Convulsant/Seizure/Epileptic,
Current research includes investigating approaches to enhance glutamate transporter function and expression https://onlinelibrary.wiley.com/doi/full/10.1111/jnc.13200 and focus on role of Dysfunction of EAAT2 as it correlates with various pathologies such as traumatic brain injury, stroke, amyotrophic lateral sclerosis, Alzheimer's disease, among others. Therefore, activators of the function or enhancers of the expression of EAAT2/GLT‐1 could serve as a potential therapy for these conditions.
Click for further researchTraumatic Brain Injury Rehabilitation, Treatment, and Case Management, Fourth EditionPromise of ISR Inhibitors In Treating Age-Related Cognitive Declinehttps://www.bio-itworld.com/news/2021/01/27/promise-of-isr-inhibitors-in-treating-age-related-cognitive-declineFirst hint that body’s ‘biological age’ can be reversedhttps://www.nature.com/articles/d41586-019-02638-w SCIENTISTS MAY HAVE FINALLY FIGURED OUT HOW TO REVERSE AGING IN THE BRAINhttps://www.inverse.com/mind-body/cognitive-decline-can-be-reversed-in-mice-what-the-new-study-means Probiotics and phytonutrients reverse age by three years, researchers claimhttps://www.nutraingredients.com/Article/2021/05/28/Probiotics-and-phytonutrients-reverse-age-by-three-years-researchers-claim Aging reversed: Study says you can become 3 years ‘younger’ in just 8 weeks! https://www.studyfinds.org/aging-reversed-biological-age-3-years-younger-8-weeks Drug Reverses Memory Failure Caused by Traumatic Brain Injuryhttps://www.ucsf.edu/news/2017/07/407656/drug-reverses-memory-failure-caused-traumatic-brain-injury Experimental Drug Reverses Cognitive Declinehttps://forums.phoenixrising.me/threads/experimental-drug-reverses-cognitive-decline.82229 Interleukin 37 reverses the metabolic cost of inflammation, increases oxidative respiration, and improves exercise tolerancehttps://www.pnas.org/content/114/9/2313 Chronic Fatigue Syndrome - Directions for Immunotherapyhttps://hbot.com/chronic-fatigue-syndrome-directions-for-immunotherapy/?fbclid=IwAR1HSk7Y_JJm-nkkUp4eXsQzgDPZC4RsxVHuZyHNbVLN7dVTjsTd7jl7_zEYoung Blood Reverses Some of the Effects of Age-Related Cognitive Declinehttps://scitechdaily.com/young-blood-reverses-some-of-the-effects-of-age-related-cognitive-decline SCIENTISTS DISCOVER A “MIND-BLOWING” LINK BETWEEN GUT HEALTH AND AGE REVERSALhttps://www.inverse.com/science/gut-aging Microbes Turn Back the Clock: New Research Discovers Their Potential To Reverse Aging in the Brainhttps://scitechdaily.com/microbes-turn-back-the-clock-new-research-discovers-their-potential-to-reverse-aging-in-the-brain Scientists Reversed Aging in Mouse Brains With Poo Transplants From Young Micehttps://www.sciencealert.com/scientists-rewound-ageing-in-mice-by-changing-their-gut-bacteria Researchers discover drug that reverses mental decline, aginghttps://wjla.com/news/nation-world/researchers-discover-drug-that-reverses-mental-decline-aging Coconut oil may be able to reverse the progression of Alzheimer's diseasehttps://www.naturalnews.com/035045_coconut_oil_Alzheimers_brain_function.html A Promising Molecule may reverse Brain Damagehttps://www.drshehadi.com/a-promising-molecule-may-reverse-brain-damage Rapid Mental Rejuvenation: Experimental Drug Reverses Age-Related Cognitive Decline Within Dayshttps://scitechdaily.com/rapid-mental-rejuvenation-experimental-drug-reverses-age-related-cognitive-decline-within-daysSmall molecule cognitive enhancer reverses age-related memory declinehttps://elifesciences.org/articles/62048 Drug Reverses Age-Related Mental Decline Within Dayshttps://www.ucsf.edu/news/2020/12/419201/drug-reverses-age-related-mental-decline-within-daysScientists Find Promising Avenue to Restore Cognitive Function Impaired by Alzheimer’s Diseasehttps://www.nyu.edu/about/news-publications/news/2021/february/scientists-find-promising-avenue-to-restore-cognitive-function-i.htmlThe drugs fighting memory losshttps://www.pharmaceutical-technology.com/features/memory-loss-drugs-reverseHow a Specific Synapse Type Regulates Anxiety-Like Behavior - Neuroscience NewsHigh Coffee Consumption Linked to Smaller Brain Volume and Increased Dementia Risk - Neuroscience News8 Weeks of Meditation Studies Can Make Your Brain Quicker - Neuroscience NewsMotivation Depends on How the Brain Processes Fatigue - Neuroscience NewsChemists Found an Effective Remedy for "Aged" Brain Diseases - Neuroscience NewsNutritional Supplements Could Help Treat PTSD - Neuroscience NewsFine Particulate Air Pollution Associated With Higher Risk of Dementia - Neuroscience News15 Novel Biomarkers for Diseases Predisposing to Dementia Identified - Neuroscience NewsStudy Yields Tiny Targets for Healing Human Memory - Neuroscience NewsDrug That Slows Progression of ALS May Provide the Same Benefit for People With Alzheimer’s - Neuroscience NewsHigh-Fat, High-Sugar Diets Causes Bacterial Changes Related to Loss of Cognitive FunctionMagnesium Supplements Could Improve Memory and Cognitive AbilityYoung Blood Reverses Some of the Effects of Age-Related Cognitive DeclineResearchers Use FDDNP–PET Scanning to Predict Cognitive DeclineMicrobes Turn Back the Clock: New Research Discovers Their Potential To Reverse Aging in the BrainAntibiotics in Early Life Could Lead to Brain DisordersResearchers Discover a Surprising Chemical Pathway That May Protect Against Alzheimer's DiseaseBlood Pressure-Lowering Medications Linked to Less Memory Decline in Older AdultsAnti-aging Protein in Red Blood Cells Helps Prevent Mental Decline, Poor Memory and Hearing DeficitsSimple Blood Test Can Accurately Reveal Underlying Neurodegeneration (Dementia, ALS)Scientists discover a “mind-blowing” link between gut health and age reversalYoung microbiota rejuvenates the aging brain | Nature AgingScientists Reversed Aging in Mouse Brains With Poo Transplants From Young MiceMicrobes Turn Back the Clock as Research Discovers Their Potential to Reverse Aging in the Brain - Neuroscience NewsGut bacteria rewind ageing brain in micefix peptide tbi medicine - Google SearchAcute secondary adrenal insufficiency after traumatic brain injury: a prospective study - PubMedA new way of thinking: hydrocortisone in traumatic brain-injured patientsCortisol-Replacement-Therapy-Booklet.pdfStress-dose hydrocortisone reduces critical illness-related corticosteroid insufficiency associated with severe traumatic brain injury in rats | Critical Care | Full TextLow Dose of Valproate Improves Motor Function after Traumatic Brain InjuryHigh-Dose Intravenous Ascorbic Acid: Ready for Prime Time in Traumatic Brain Injury? | SpringerLinkTrkB-enhancer facilitates functional recovery after traumatic brain injury | Scientific ReportsProspective, randomized, blinded, and placebo-controlled study of Cerebrolysin dose-response effects on long-term functional outcomes in a rat model of mild traumatic brain injury in: Journal of Neurosurgery Volume 129 Issue 5 (2018)IL-1ra Dose-range Study for Moderate-to-severe TBI Patients - Full Text View - ClinicalTrials.govA peptide for targeted, systemic delivery of imaging and therapeutic compounds into acute brain injuries | Nature CommunicationsPeptidergic Drugs for Treatment of Traumatic Brain Injuryinject trophic factors tbi medicine - Google SearchBrain-derived neurotrophic factor delivered to the brain using poly (lactide-co-glycolide) nanoparticles improves neurological and cognitive outcome in mice with traumatic brain injury - PubMedAdvance of Stem Cell Treatment for Traumatic Brain InjuryFull article: Brain-derived neurotrophic factor delivered to the brain using poly (lactide-co-glycolide) nanoparticles improves neurological and cognitive outcome in mice with traumatic brain injuryinject trophic factors cfs medicine - Google SearchResveratrol improves hippocampal atrophy in chronic fatigue mice by enhancing neurogenesis and inhibiting apoptosis of granular cells - PubMedHochu-ekki-to combined with interferon-gamma moderately enhances daily activity of chronic fatigue syndrome mice by increasing NK cell activity, but not neuroprotection - PubMedChronic Fatigue Syndrome - Medical Clinical Policy Bulletins | AetnaTreatment Avenues in Myalgic Encephalomyelitis/Chronic Fatigue Syndrome: A Split-gender Pharmacogenomic Study of Gene-expression Modules - Clinical TherapeuticsCentral adrenal insufficiency following traumatic brain injury: a missed diagnosis in the critically injured - PubMedJCM | Free Full-Text | Impaired Pituitary Axes Following Traumatic Brain Injury | HTML## Lisdexamfetamine cfs - Google SearchJust a moment...Efficacy and Safety of Lisdexamfetamine Dimesylate in Adults With Chronic Fatigue Syndrome - Full Text View - ClinicalTrials.govEfficacy and Safety of Lisdexamfetamine Dimesylate in Adults With Chronic Fatigue Syndrome outcome - Google SearchMedications Used To Treat Chronic Fatigue Syndrome (CFS)Lisdexamfetamine User Reviews for Chronic Fatigue Syndrome at Drugs.comlisdexamfetamine dimesylate - Google Search

back to top
back to top
back to top
back to top
back to top
back to top
back to top
back to top
back to top
back to top
back to top
back to top
back to top
back to top
back to top
back to top
back to top
back to top
back to top
back to top
back to top
back to top
back to top
back to top




Click 1
Click 2
Click 3
back to top











