Free Head Injury Foundations and Clinics
National: will update site
Local: will update site
Testing
brain imaging diagnostic tool called SPECT (Single Photon Emission Computed Tomography) accurately identify underlying brain issues that can contribute to symptoms.
Available at https://www.amenclinics.com
Address 350 N. Wiget Lane, Suite 105
Walnut Creek, CA 94598
Phone 650-416-7830
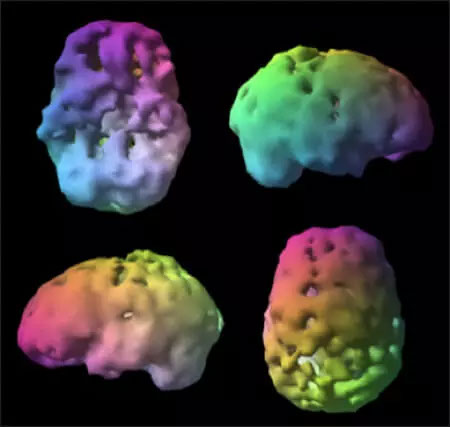 Example of unhealthy SPECT Brain Scan
Example of unhealthy SPECT Brain Scan
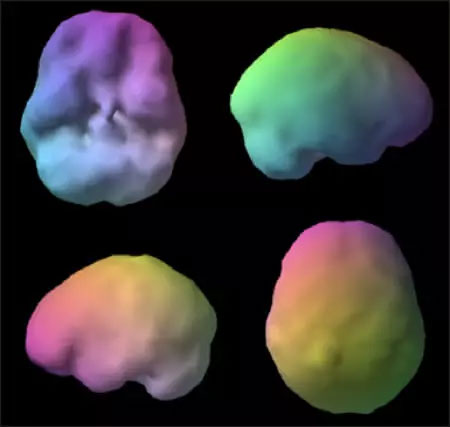 Example of healthy SPECT Brain Scan
Example of healthy SPECT Brain Scan
'The Injured Brain: TBI, mTBI, the Immune System, and Infection: Connecting the Dots'
Brain injury or trauma causes immune system suppression. Infection is a serious consequence of these events and is present in both open and closed TBI, mTBI, and with stroke. CD4 T-lymphocyte count may be a marker to determine emergence of infection after brain trauma, including stroke
From: Phoenix rising user 'MishMash' http://forums.phoenixrising.me/index.php?threads/head-injury-and-hypopituitarism.22717
Head injuries can cause collapse or damage to the pituitary gland. Which can be seen in a scan (sometimes). This usually correlates, but not always, to symptoms of low pituitary function.
But the number of people who have collapsed pituitary gland, and hence low pituitary function, due to accidents, head injuries is tiny compared to the number who get it idiopathically. Collapsed, or disappearing, pituitary gland is known as "empty sella syndrome," because the gland sits naturally in a bone cavity called "the sella."
ESS is very common among CFS patients BTW. Before he left, Cort did an interesting feature on this for PR. A number of members posted they had ESS. Cort himself said the radiologist noted that his pituitary gland had disaappeared. One of the things he was recommending as a CFS spokesman was further research into this.
The chances for getting ESS go up markedly as age increases. Intracranial hypertension (too much brain fluid pressure) is usually cited as the reason for young people getting it. Too much brain fluid pressure has been associated with connective tissue weakness (or Ehlers-Danlos) since the cerebral ducts are weak and floppy, and get kinked and clogged easily. So the fluid just keeps building up in your cranium. Which leads to lower blood flow to the brain, if the theory is correct.
Some people go as far as putting in shunts. I've done quite a bit of research on this, and the shunts rarely result in reduction in symptoms, from what I've read. The doctor at "prettyill.com" has recommended taking diuretics to reduce cerebral brain fluid amounts; hence reducing pressure on the brains, and lowering frequency of headaches.
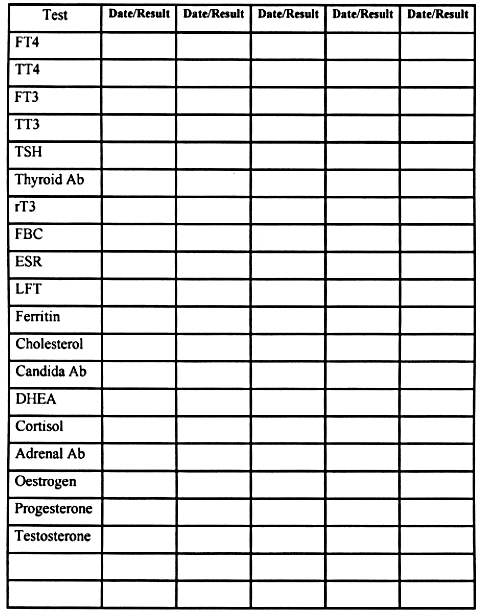
Thyroid and Adrenals
A lab test for identifying adrenal fatigue is a saliva test. It s important to take samples of the saliva at different times of the day in order to establish the true cortisol rhythm and DHEA levels. Samples are taken in the morning (6am-8am), midday (12pm-1pm), late afternoon (4pm-5pm) and nighttime (10pm-midnight). Cortisol should be at the highest in the morning and the lowest at night.
Taking your body temperature when you wake up in the morning and finding that your temperature is below 97.8 degrees Fahrenheit can help to detect adrenal and/or thyroid problems
Please note that adrenal fatigue (exhaustion) has three different stages before it reaches failure. People in stage one of adrenal fatigue have a high amount of cortisol overall and at least one cortisol reading that is higher than it should be. An overall high count and a spike at an inappropriate time of the day indicates there is a problem. Cortisol must be kept under control because it eats muscle when at an excessively high level.
Stage two of adrenal fatigue is commonly misdiagnosed and can even go undiagnosed entirely. This primarily happens because a person s total cortisol level is normal in stage two! The key indicators in this stage are the DHEA level and a low level of cortisol in the morning, midday, or afternoon. The trouble with properly identifying adrenal fatigue in stage two is that cortisol levels are often normal at night and the overall reading usually averages in the normal range as well. Again, cortisol should be at the highest in the morning and lowest at night. If a client is experiencing low cortisol levels when it should be at its peak, there is a problem.
Stage three of adrenal fatigue is the easiest to identify. The DHEA level is low and most cortisol levels are borderline low or low throughout the day. And of course, the total cortisol level is low as well. Low nighttime cortisol is a major marker for late stage three adrenal fatigue.
There are some tests that can be taken at home which tell you if adrenal fatigue is part of your problem. For example, go into an indoor room that is away from the natural sunlight (a room with no windows or, at the very least, with the shades lowered) with a small flashlight. Shine the light at a 45-degree angle towards your eye and you will see your pupil shrink (the pupil is the black center of your eye). The light of the flashlight will cause the pupil to shrink and it should remain constricted while the light is being pointed at your eye. You likely have adrenal problems if you see your pupil pulsing (alternating between being bigger and smaller). While this simple test shouldn t replace an actual diagnosis, it does point to what could be the source of your issues and it would be something to further investigate with a health professional.
Another test is I recommend involves an electronic blood pressure cuff (the Omron® blood pressure cuff can be purchased online for around $50-60). Place the blood pressure cuff on your arm as you normally would when measuring your blood pressure but lay down on your back for 5-10 minutes before taking the measurement. Have someone write down what the measurement is. Then stand up as fast as you can, take your blood pressure again, and write down that number. You are looking for the difference in blood pressure numbers between lying down and standing. This is called an orthostatic measurement.
To illustrate, let s say someone s measurement is 120/80 when laying down and jumps to 130/85 immediately after standing. That s good! The body naturally increases blood pressure when standing because gravity places more demands on our bodies. It is normal and healthy to see both the systolic rate (the top number) and the diastolic rate (the bottom number) increase 5-10 mmHg when going from laying down to standing. What if the rate doesn t go up? For example, let s say a person s lying down blood pressure rate is 120/80 but it goes down to 110/80 immediately after standing. That s bad. When this occurs, I often find the person has adrenal dysfunction and toxicity issues. Similarly, people who become light headed or dizzy when rising from a lying or sitting position also tend to have adrenal dysfunction and toxicity issues.
Conventional practitioners generally determine if a patient has thyroid problems by testing their TSH level. What I find interesting is that TSH (thyroid stimulating hormone) is not even manufactured by the thyroid! It s actually manufactured by the pituitary gland and is meant to communicate with the thyroid. Low TSH indicates hyperthyroidism (overactive) and high TSH suggests hypothyroidism (low functioning).
Conventional testing says that normal values for TSH are typically .5 to 5 /mL. I believe that is too big of a range. I would not use the conventional bell curve that is used to determine the normal range. Instead, I recommend all practitioners and those who suspect they have thyroid dysfunction to use the optimal values that are between 1.8 and 3 /mL. The bell curve used to show the normal range is established by sick people! Think about it: who has their TSH tested? People who are displaying symptoms of having a dysfunctioning thyroid! To be on the edges of what is considered normal in that group is not optimal.
Like I said earlier, TSH communicates and works with the thyroid. The pituitary gland in the brain releases TSH which then stimulates the thyroid gland. The thyroid gland then produces its T4 hormone (and a small amount of T3), which is then converted to the T3 hormone primarily in the liver. T3 is the active form of the thyroid hormone and is the most important.
To take it to another level, there is a difference between Total T4 and Total T3 vs. Free T4 and Free T3. The body s cells can only use the free forms of the hormone and Free T3 is the most important. Your body uses proteins to transport T4 & T3 hormones in the blood stream. Your body breaks up the proteins and allows the T3 to be absorbed at the cellular level (which makes it Free T3).
T4 is converted to T3 primarily in the liver and this is typically a problem for most people with hypothyroidism. During times of stress the body converts T4 into Reverse T3 (RT3) instead of T3. This is a normal process that typically is very short lived. When the body is under extreme physical, chemical and/or emotional stress this conversion of T4 into Reverse T3 becomes chronic and is very dangerous.
The leading cause of hypothyroidism is caused by an autoimmune condition called Hashimoto s Disease, which was the first to be recognized as an autoimmune condition in 1912. Hashimoto s Disease causes the body to attack its own thyroid gland tissues. Testing thyroid antibody levels (TPO and TG) reveal this problem. The most common symptom of the disease is feeling worse even with thyroid replacement hormone treatment. Another symptom is when lab tests show both hypothyroid and hyperthyroid levels at different times.58 When diagnosing a client with potential thyroid problems I always recommend a complete thyroid panel that includes at least: TSH, Free T4, Free T3, Reverse T3 and Thyroid Antibodies. Depending on what is found in the lab tests, there are different protocols we could follow to heal the thyroid.
Most doctors don t run Reverse T3 or Antibody testing because their treatment would be the same regardless of the results. They typically give a prescription synthroid (or generic Levothyroxine), which is a T4 hormone replacement. If the patient is seeing an alternative medicine practitioner they will typically be switched to Armour thyroid, which is a bio-identical T3/T4 hormone from pigs, not just T4. A recent issue that has emerged is that the manufacturers of Armour thyroid are reducing their production costs by adding gluten as a filler. If you need a bio-identical T3/T4 hormone, I recommend that you find a compound pharmacy to specifically make it for you and eliminate the gluten
Skill Level 1
Relevance:5 Technical Level:1
Get your testing done
page 52 PTBICF > TESTING, TESTING LABORATORIES, TREATMENT CENTERS, SPECIALISTS and CLINICS
page 51
page 53
page 52 PTBICF > TESTING, TESTING LABORATORIES, TREATMENT CENTERS, SPECIALISTS and CLINICS
page 51
page 53














