Skill Level 4
Relevance:5 Technical Level:5
Pregnenolone on it's own will likely yield significant improvements but must be incorporated as part of a multi faceted approach for radical healing
Page Synopsis: Very low cholesterol levels are often seen in CFS (sometimes high levels are seen, but these are usually due to low thyroid function) as well as dramatically low levels of pregnenolone. Medicating with Pregnenolone is very attractive. I will update the site when and if I decide to supplement with it. If you would like site update notifications email me with the subject line 'newsletter'
page 28 CFS > ALLOPATHIC MEDICINES > STEROIDS > PREGNENOLONE
page 27
page 28b
Pregnenolone is the main precursor of various steroid hormones, including progesterone, is the very first steroid hormone made directly from cholesterol, and its formation is the first step to a complex process that produces all “steroid” hormones. Common steroid hormones include estrogens, progesterones, androgens (testosterone) and glucocorticoids (cortisol). Therefore, a decline in pregnenolone can create a generalized decline in all of the steroid hormones.
Pregnenolone also functions as a neurotransmitter in the brain and it works particularly in the area of the brain responsible with memory. Many patients report an improvement in memory when taking pregnenolone
Neurosteroids are endogenous steroids synthesized within the central nervous system that rapidly alter neuronal excitability through interactions with receptors at the neuronal membrane. Neurosteroids are also called neuroactive steroids and are synthesized from cholesterol, independently of the peripheral steroidogenic endocrine glands. Cholesterol and circulating steroid hormones serve as precursors for the synthesis of neurosteroids, which are produced locally in the hippocampus and other brain structures (Baulieu and Robel, 1990). Allopregnanolone (AP), allotetrahydrodeoxycorticosterone (THDOC), and androstanediol (AD) are examples of some of the most widely studied neurosteroids (Table 4.1). These neurosteroids do not directly interact with steroid hormone receptors, but their metabolites can bind to intracellular steroid receptors. Neurosteroids and neurosteroid-based compounds offer a vast therapeutic potential for treatment of conditions such as epilepsy, anxiety, and psychiatric disorders
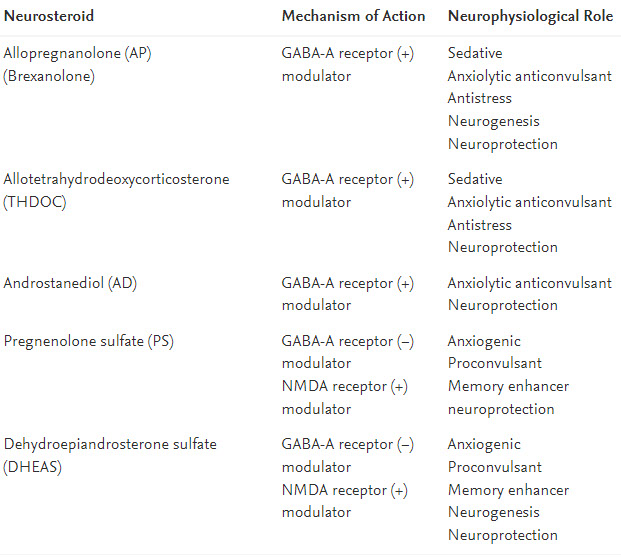
Neurosteroids exert a large array of biological activities in the brain, either through a conventional genomic action or through interaction with the membrane receptor. In particular, neurosteroids act as allosteric modulators of the GABAA receptor (Fig. 124.2); the N-methyl-d-aspartic acid (NMDA) receptor (Fig. 124.2); the kainate receptor; the α-amino-3-hydroxy-5-methyl-4-isoxazolepropionate acid (AMPA) receptor; the σ receptor; the glycine receptor; the serotonin receptor; the nicotinic receptor; and the muscarinic receptor.6 Neurosteroids may directly activate the G protein-coupled membrane receptor or indirectly modulate the binding of neuropeptides to their receptor
Neurosteroids are classified into three classes based on their structure (Fig. 4.1): (1) pregnane neurosteroids, such as AP and THDOC; (2) androstane neurosteroids, such as androstanediol and etiocholanone; and (3) sulfated neurosteroids, such as pregnenolone sulfate (PS) and dehydroepiandrosterone sulfate (DHEAS) (Aird and Gordan, 1951; Gyermek, 1967; Green et al., 1978; Reddy, 2003, 2010). Neurosteroids and neurosteroid sulfates interact with a wide variety of neurotransmitter receptors in the brain. Pregnane and androstane neurosteroids are positive allosteric modulators of γ-aminobutyric acid type A (GABA-A) receptors, the primary mediators of inhibitory neurotransmission. Neurosteroid sulfates are known to interact with a wider variety of receptors including N-methyl-d-aspartate (NMDA) receptors and sigma receptors (Bowlby, 1993; Reddy, 2010). This chapter describes current knowledge of neurosteroids, with an emphasis on their biosynthesis, molecular mechanisms of action, and their neurophysiological functions in brain conditions such as epilepsy, anxiety, and psychiatric disorders 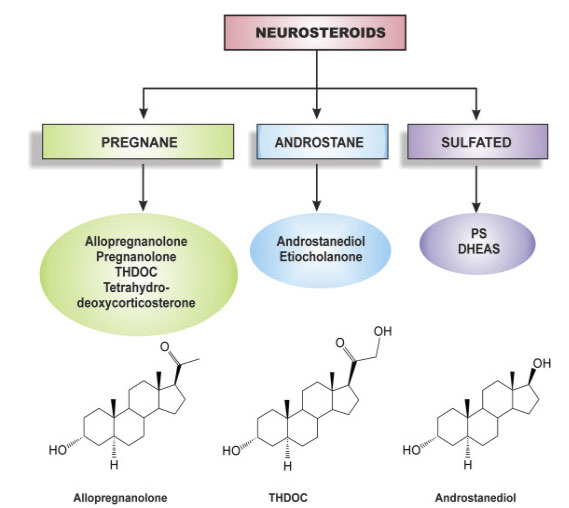
Mitochondria are involved in steroid hormone (glucocorticoids, mineralocorticoids, estrogens, progesterons, androgens, and neurosteroids) biosynthesis of which cholesterol is the precursor. For the synthesis of steroid hormones (Fig. 1), cholesterol must be transported from the cytosol to the inner membrane of the mitochondria via a series of protein-protein interactions involving cytosolic and mitochondrial proteins located at both the outer and inner mitochondrial membranes.1,2 This transfer is provided mainly by the StAR (steroidogenic acute regulatory) proteins later renamed STARD1. Full-length StAR is a 37 kDa protein with a C-terminal cholesterol-binding domain and an N-terminal mitochondrial targeting sequence common to matrix proteins. StAR is a big cholesterol transporter that is synthesized just after hormonal stimulation and contributes to steroidogenesis. StAR, however, does not act in every tissue, such as in the nervous system and the placenta, involved in steroid synthesis. Thus, in these steroidogenic tissues, the transfer of cholesterol from the cytosol to the mitochondria is done by other means 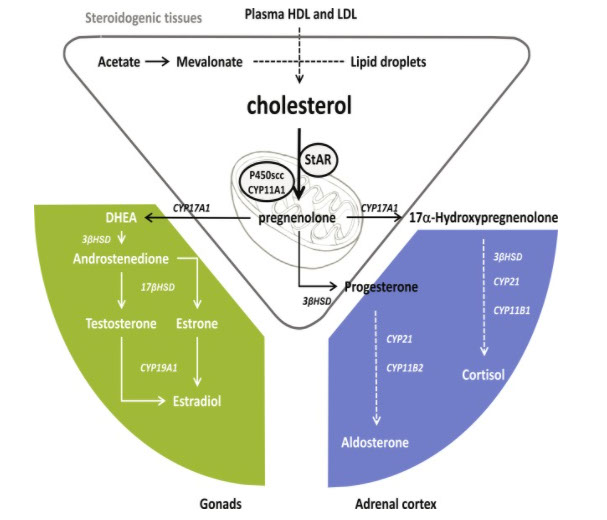
Dehydroepiandrosterone sulfate
Considered a “neurosteroid,” DHEA and dehydroepiandrosterone sulfate (DHEAs) are molecules produced by the adrenal gland. Low DHEA levels are related to symptoms and severity of depression and anxiety.68 DHEA may protect against the adverse effects of stress, especially with regard to the brain atrophy caused by chronically high levels of cortisol. Like exercise, DHEA can increase neuronal growth in the hippocampus and will protect new nervous tissue from being destroyed by stress hormones. Higher levels are likely present in bipolar disorder.69 Generally, supplementation when low is helpful. A 2014 literature review looked at 22 studies, finding DHEA supplementation is helpful for depressive symptoms overall.70 One case in the literature suggested 150 to 200 mg per day of DHEA may have contributed to acute mania onset in a patient with a history of these episodes
7α-hydroxypregnenolone was identified as a novel bioactive neurosteroid stimulating locomotor activity in the brain through activation of the dopaminergic system in newts and quail. In the brain, 7α-hydroxypregnenolone is synthesized from pregnenolone by the action of cytochrome P450 7α-hydroxylase (P4507α) in vertebrates. Interestingly, melatonin derived from the pineal gland and eyes regulates 7α-hydroxypregnenolone synthesis in the brain, thus inducing diurnal locomotor changes. Prolactin, an adenohypophyseal hormone, regulates 7α-hydroxypregnenolone synthesis in the brain, and may also induce seasonal locomotor changes. Acute stress increases the synthesis of 7α-hydroxypregnenolone via corticosterone action in the diencephalon, and 7α-hydroxypregnenolone activates serotonergic neurons in the diencephalon that may coordinate behavioral responses to stress
According to current knowledge, neurosteroids are synthesized throughout the central and peripheral nervous systems by both glial cells and neurons. It is important to determine in which part of the nervous system and in which cell type a particular neurosteroid is synthesized. However, regarding the question of which steroids can be synthesized within the nervous system, it is necessary to be careful of making excessive generalizations because of the regulated expression of steroidogenic enzymes. Some examples illustrate the complexity of the problem. First, in the adult rat brain, aromatase is exclusively expressed in neurons. However, in response to an excitotoxic or traumatic injury, the enzyme becomes strongly expressed in astrocytes. Second, when cultured at low density, astrocytes preferentially convert pregnenolone into progesterone, whereas pregnenolone is nearly exclusively metabolized to 7α-OH-pregnenolone at confluency. Third, cell culture experiments have provided evidence that the neuroactive progesterone metabolite allopregnanolone is mainly synthesized by glial cells and acts on GABAA receptors of nearby neurons by a paracrine mechanism. This finding is supported by in vivo experiments showing that 3α-HSOR activity in the rat olfactory bulbs is unchanged after the infusion of kainic acid, which destroys neurons but lets glia intact. Conversely, other results have shown that 3α-HSOR is present in the principal glutamatergic neurons of the cerebral cortex, the hippocampus, and the olfactory bulbs and is co-localized with 5α-reductase type 1. Fourth, in peripheral nerves, Schwann cells only express 3β-HSD and synthesize progesterone when in contact with axons. Therefore, these examples indicate that the description of neurosteroid biosynthetic pathways needs to be interpreted according to the experimental context
Neurosteroids are synthesized in astrocytes, oligodendrocytes, Schwann cells, Purkinje cells, hippocampal neurons, and retinal amacrine and ganglion cells.33–36 Cholesterol is transported to glial mitochondria, where it is converted to pregnenolone. In the cytosol, pregnenolone is then converted to different neurosteroids such as allopregnanolone and dehydroepiandrosterone (DHEA). DHEA is a precursor of testosterone, which is converted to estradiol by an aromatase.34,36 Vitamin D is also an important neurosteroid.37 Synthesis of neurosteroids is regulated by interactions between neurons and glial cells.
Neurosteroids have many important actions. Allopregnanolone activates neuronal GABAA receptors having anxiolytic, sedative, sleep-inducing, and anticonvulsant effects. Benzodiazepines, alcohol, and γ-hydroxybutyrate increase brain levels of allopregnanolone. Thus these drugs may potentiate GABAergic transmission directly and also by increasing allopregnanolone. Pregnenolone sulfate, DHEA, and DHEA sulfate (DHEA-S) are inhibitory, noncompetitive modulators of GABAA and positive modulators of N-methyl-d-aspartate (NMDA) receptors by facilitating calcium influx. Estradiol inhibits NMDA receptors. Neurosteroids acting on NMDA are implicated in cognition, neuroprotection, and neurotoxicity. While pregnenolone sulfate is excitotoxic to cortical and retinal cells, DHEA and DHEA-S have neuroprotective effects against glutamate toxicity. However, the exact mechanisms of such neuroprotective effects are not clear.
Neurosteroids have been implicated in many neurologic and psychiatric disorders, including epilepsy, neurodegenerative diseases, schizophrenia, and depression. For example, depression is associated with reduced levels of allopregnanolone in cerebrospinal fluid. Antidepressant treatment with fluoxetine increases allopregnanolone levels.38 There is also some evidence that DHEA helps in the treatment of depression. The beneficial effect of DHEA correlates with a decrease of glucocorticoids, which are increased in depression.
There is increasing evidence about many important roles of neurosteroids in regulation of vigilance as well. It remains to be studied whether nutritional factors could also play some role in this. DHEA is marketed in pharmacies and health shops. Little is known about possible positive (and, perhaps, also negative) long-term neuropsychiatric effects of nutritional factors that may cause changes in brain neurosteroids
Neurosteroids have been reported to modulate learning and memory processes in young, aged rodents and in pharmacological models of amnesia. PS infused into the basai magnocellular nucleus enhanced memory performance, whereas AP disrupted memory 167, Pregnenolone, PS, DHEA, and DHEAS increased memory when injected systemically 168, 169, centrally 170, 171 or into the amygdala 172, PS has also been reported to enhance learning in the Morris water maze 173 and improves acquisition and retention in a food search task 174, In contrast to this, post-training administration of AP reduced retention of memory in a conditioned odour task in rat pups 175, PS and DHEAS produced attenuating effects on the muscarinic receptor antagonist, scopolamine 176 and non-competitive NMDA receptor antagonist, dizocilpine 113, 177, competitive NMDA receptor antagonist, 3-(+)-2-(carboxypiperazin-4-yl)-propyl-1-phosphonic acid (CPP) 178, and ethanol 179 induced amnesia in various cognitive paradigms in rodents. Although the precise mechanism by which neurosteroids affect learning and memory is unknown, it is interesting to hypothesize that memory loss associated with many neurological diseases and normal developmental processes in humans, including ageing, may be a resuit of altered neurosteroidogenesis.
Normal ageing is associated with a decline in cognitive and other brain functions. Apart from the degeneration of cholinergic neurons, there is evidence to suggest that the cognitive dysfunction associated with ageing is characterized by decreased levels of DHEA and DHEAS 90, 180. Neurosteroids are also implicated in Alzheimer’s disease 90, 181. Administration of DHEA and DHEAS improved performance in the retention of memory in aged animais 182, indicating a possible pathological role for neurosteroids in dementia related cognitive disorders. Pregnenolone, dehydroepiandrosterone, and their sulphate esters, dose-dependently attenuated the memory deficits induced by β25–35 peptide, a protein implicated in Alzheimer’s disease and the effects of the neurosteroids were blocked by the a receptor antagonist haloperidol and by progesterone 183, In a modified passive-avoidance paradigm, neurosteroids PS or DHEAS facilitate acquisition and consolidation rather than retrieval of memory processes, independent of state-dependent effects on learning 184.
Inhibitors of steroid sulphatase, an enzyme which converts sulphated steroids into free steroids, may alter the metabolism of neurosteroids and may modulate brain function. The steroid sulphatase inhibitor estrone-3-O-sulphamate and p-O-(sulphamoyl)-N-tetradecanoyl tyramine 185, 186 potentiated the antiamnesic effect of DHEAS, suggesting that increasing the levels of endogenous sulphated neurosteroids via the inhibition of steroid sulphatase activity may enhance learning and memory function. Further developments in this field would augment the therapeutic potential of sulphatase inhibitors in the treatment of cognitive disorders.
The exact mechanism and even specificity of the memory enhancing effect of neurosteroids is currently not known. It is thought that steroid hormones bind to specifie receptors in the cytoplasm, which translocate into the nucleus and finally regulate gene transcription or affect translational efficiency and protein stability. These effects are postulated to be involved in long-lasting learning and memory storage. Alternately, it has been hypothesized that a cell membrane receptor mechanism(s) may also be involved in the effects of neurosteroids in learning and memory processes. Neurosteroids have been shown to affect the activity of neurotransmitter systems which are involved in the learning and memory processes. PS and DHEAS are negative allosteric modulators of the GABA-A receptor 2, 88 and positive modulators of NMDA receptor-mediated responses 101, 102, Recently, increasing evidence indicates that the neurosteroids PS and DHEAS act as agonists at central σ receptors and exert a facilitatory action on NMDA-mediated glutamatergic neurotransmission 106. DHEAS attenuates dizocilpine-induced learning impairment via σ1 receptors 113, which would further support our argument for a receptor-mediated signalling mechanism in the nootropic and antiamnesic effect of neurosteroids. On the basis of these studies it is speculated that a direct interaction between neurosteroids and σ1 receptors could constitute a possible mechanism for the neurosteroidal non-genomic effects in learning and memory processes. The effects of neurosteroids on learning and memory processes may involve, at least in part, an interaction with central σ receptors, since they could be significantly blocked by concurrent administration of haloperidol, a prototypical a receptor antagonist, or NE-100, a selective σ1 receptor antagonist 113, 184.
In view of the importance of nitric oxide (NO) as a critical mediator in learning and memory processes and long-term potentiation, we studied the possible involvement of a neuronal NO mechanism in the nootropic and antiamnesic effects of neurosteroids PS and DHEAS on ageing- and dizocilpine-induced cognitive dysfunction in mice 187. The allosteric agonist actions of neurosteroids PS and DHEAS at NMDA receptors play an important role in the cognitive process. PS and DHEAS, at doses of 1–20 mg/kg, significantly attenuated the amnesia induced in mice by systemic administration of dizocilpine in a step-down type of passive-avoidance paradigm, and did not themselves affect mnemonic capacity. Preadministration of l-NAME, a NO synthase inhibitor, significantly blocked the PS- and DHEAS-induced attenuation of dizocilpine-induced amnesia 187, Furthermore, this effect of l-NAME was completely reversed by l-arginine, a competitive substrate for NO synthase, confirming that it was a specifie effect mediated through inhibition of central NO synthase. In addition, the learning impairment observed in aged (16 months old) mice could be significantly ameliorated by PS and DHEAS. These ameliorative effects of neurosteroids may involve at least partly a NO mechanism, since they could be significantly prevented by preadministration of l-NAME, and the effect of l-NAME was reversed by l-arginine 187, Taken together, these results strongly indicate a NO-dependent mechanism in the nootropic and antiamnesic activity of neurosteroids, particularly in the long-term memory processes.
Despite their possible involvement with NO, neurosteroids such as progesterone or its metabolite allopregnanolone, however, do not significantly affect blood pressure. Acute administration of progesterone (1 mg/kg i.p.) 224a or allopregnanolone (0.5 mg/kg i.p.) 224b had no effect on arterial blood pressure. However, neurosteroids may produce transient marginal changes in arterial pressure by indirect mechanisms by acting at central nuclei involved in cardiovascular regulation. For example, allosteric potentiation of GABA-A receptor function by allopregnanolone in nuclei involved in the baroreflex pathways may modulate autonomie regulation of blood pressure in conditions such as during pregnancy. Similarly, both threshold pressure and saturation pressure for inhibition of rostral ventrolateral medulla neurones were decreased after administration of allopregnanolone
Neurosteroids also modulate N- and L-type calcium channels. Pregnenolone, THDOC, and PS, but not progesterone, all depress the maximal current up to 60%, as well as slow activation and deactivation of these calcium channels in hippocampal CA1 neurons. This effect may be mediated by an extracellular receptor because intracellular dialysis with PS has no effect. Furthermore, neurosteroids may work through action of G-protein-coupled receptors because pretreatment with toxin from Bordetella pertussis (pertussis toxin), an inhibitor of Gαi,o, or intracellular dialysis with GDPβS blocks the effects of PS. The neurosteroid binding site mediating these effects is pharmacologically distinct from the GABAA modulatory site. Unlike PS actions at GABAA receptors, both the neurosteroids and their sulfated derivative have similar effects. The replacement of the sulfated group with acetate abolishes the physiological activity of PS, and progesterone has no effect.
In an independent series of experiments, picomolar concentrations of estrogen were shown to inhibit rapidly (within seconds) L-type calcium channels in acutely dissociated striatal neurons. Unlike estrogenic modulation of glutamate receptors, E2 coupled to bovine serum albumin (E2–BSA) readily mimicked the effect of free E2, suggesting an extracellular binding site. As with the other neurosteroids, the effects of estradiol may involve activation of G-proteins. Those cells that were dialyzed with 5′-O-(3-thiotriphosphate) (GTP-γ), which is a G-protein-activating GTP analogue that is more resistant to hydrolysis than GTP, had an irreversible suppression of Ca2+ channels. Interestingly, a similar inhibition of L-type calcium current by estrogen, but not progesterone, has been demonstrated in vascular smooth muscle
![]()
Exciting New Discovery in Treating CFS & Fibromyalgia
New research suggests that statins might have a very helpful antiviral effect at high dose, and they may even hold promise as an effective new treatment for CFS & fibromyalgia if special (and simple) natural precautions are added in. The new theory I will present today also offers new possibilities for helpful and easy testing and treatment, while offering an understanding of a large new piece of the CFS/FMS puzzle.
Although time will tell how big a role this new concept will play in CFS, it offers simple testing and treatment that can be helpful NOW!
An Important Cautionary Note
I usually prefer to have broader research and more direct clinical and personal experience exploring new treatment theories before I start reporting on them (which would take 1-2 years). I have chosen instead to put the theory out there to invite discussion. Bringing many expert perspectives to bear will help it get tempered closer to the truth more quickly. Much of what I discuss below is new, controversial and hypothetical, and should be discussed with your holistic practitioner or CFS specialist before attempting a trial of the statin prescriptions.
Background
Many infections have been implicated in CFS, including the recent reporting of XMRV. As part of their reproductive cycle, many viruses require cholesterol-related molecules for many different functions, including making their protective coat. As part of your body's defensive functioning, your cells make an important family of immune molecules called interferon, which seems to work in part by decreasing the cholesterol production pathway and starving the virus.
Interferon levels (there are 27 different types) can be both high or low in CFS. In CFS patients, interferon alpha tends to be low while interferon beta is elevated. Interestingly, interferon injections can trigger symptoms that feel like CFS. Paradoxically, in a small subset of CFS patients interferon treatment helped (though not a lot).3-4
So what to do? You might be able to "eat your cake, and have it too" by starving the virus while giving your body the natural support it needs. This new research opens possible ways to suppress the many viral infections in CFS, even retroviruses such as XMRV!
Found - A Key Missing Piece of the CFS Puzzle!
Although the energy crisis and associated hypothalamic dysfunction, along with direct gland failure (e.g., low thyroid adrenal exhaustion) explained most of the abnormalities we see in CFS and fibromyalgia, there have been a few missing pieces over the years that were not explained by these - which frankly left us puzzled. Here are a couple items I've scratched my head over in CFS:
article continues after advertisement
Very low cholesterol levels are often seen in CFS (sometimes high levels are seen, but these are usually due to low thyroid function).
Dramatically low levels of a hormone called pregnenolone (made from cholesterol, pregnenolone is the critical building block for steroid hormones such as estrogen and testosterone).
This new study now explains why cholesterol and pregnenolone are sometimes very low in CFS. Viral infections cause your body to make interferon, which suppresses the mevalonic acid pathway that makes cholesterol and pregnenolone.
This is likely another key reason - along with the hypothalamic dysfunction, gland dysfunction and receptor resistance - for the widespread hormonal disorders we see in CFS/FMS.
This finding is significant in that it not only suggests that low cholesterol or pregnenolone in CFS may be caused by a viral infection, it also suggests new possible treatments!
Key Points
This work uncovers a potential novel cause of CFS involving the process your body uses to make cholesterol. Here are the key points to this:
The production of cholesterol, coenzyme Q10 (CoQ10, a key energy metabolite), and other key hormones relies on your body's mevalonate pathway. The new research suggests that viral infections "hijack" this pathway to make their protective outer coats. In response, your body makes interferon, which suppresses the mevalonate pathway, which in turn suppresses the virus.
Acute infections respond well to this, as the interferon production is helpful short term. But long term, this can lead to starving your body of CoQ10 and key hormones. This appears to be part of what happens in CFS.
Cholesterol blockers mildly block the same pathway and can actually have a mild antiviral effect at low dose (and a strong effect at high dose). These medications are used long term to treat high cholesterol. But this may starve the body of CoQ10 and pregnenolone and can, therefore, flare CFS/FMS. So I recommend against statins unless you also give the body the CoQ10 and pregnenolone it is being starved of at the same time.
article continues after advertisement
Implications for Diagnosis
The presence of a low or low-normal pregnenolone level in someone not taking statins suggests your body is making elevated levels of interferon to fight a chronic viral infection, which also uggests a high risk of inadequate hormone production and CoQ10 deficiency. Low cholesterol levels may suggest the same thing.
Implication for Treatments
Have the pregnenolone and cholesterol blood tests performed. If either is low or low normal, add CoQ10 and pregnenolone supplementation to your diet. Also add an Omega 3 fish oil to help give your cell walls what they need while your body is blocking cholesterol production.
I also suspect the low pregnenolone is a marker for a viral infection. Though it does not identify which infection, it does offer a potentially powerful new way to stop the virus from growing. It might not kill them, but it will make it hard for them to reproduce.
So here is an overall treatment regimen to consider - especially if your CFS began with flu-like symptoms and has not improved adequately with other treatments:
Take zinc 25 mg a day for 3 months, then 15 mg daily from then on, as chronic infections will routinely cause zinc deficiency and immune dysfunction.
For 4-6 weeks, also take the pregnenolone, CoQ10 and fish oil as described above. Continue these for at least 3 months after taking the medication described below. These by themselves may leave you feeling a lot better at 6 weeks.
Here is the more experimental part that you will need to discuss with your physician Your physician may consider adding a statin medication. Take 20 mg a day for 2-4 weeks (to make sure it does not cause side effects - it usually will not, but if it does, stop it), then 40 mg a day for 3-4 weeks. If you feel OK on the medication, they can raise the dose to 80 mg a day. Continue for 3-4 months more and check or recheck your lab numbers. If this is not helping after 4-5 months, stop taking the statin - statins can cause liver and muscle inflammation. This is unusual, but it is why the testing is important.
article continues after advertisement
Which Viruses Have Been Shown to Be Suppressed by Statins?
Many different families of viruses, suggesting a broad antiviral effect. These include:
Epstein Barr Virus (inhibits its triggering lymphoma)6
West Nile Virus7 - An RNA Virus
Rotavirus - In this FDA "test tube" study, the authors noted an approximately 99% drop in some viral tests, and a bunch of deformed inactive viruses8
Polio9
Hepatitis C - but effects were mixed10-12
HIV 1 (a cousin to the AIDS and XMRV viruses)13
RSV - Respiratory syncytial virus14
And perhaps even the flu virus15
Does This Mean I Need to Avoid Cholesterol in Food?
No. The studies I've seen suggest that the branch of the chemical pathway that needs to be blocked for the antiviral effects occur before the cholesterol step, and adding cholesterol did not impact the statins antiviral activity. In fact, adding an egg or two a day (a good cholesterol source along with other nutrients) may be helpful to protect your cell membrane production.
Still to Be Answered
A lot. For example, with this theory if cholesterol levels are high, pregnenolone should not be low. But in real life, we often see a mismatch. So there are other pathways and issues going on here, and this is reflected in the studies referenced below. In addition, there are many members of the interferon family, and some are low while others are high in CFS. Also, dozens of other immune chemicals may be altered in CFS - though interferon may be a key "conductor of the cytokine orchestra," and the theory I am discussing today is meant to be an oversimplification. In addition, normal pregnenolone and cholesterol do not mean there is no virus or that the treatment above won't help. But low levels are suggestive of a viral issue.
But we do know CoQ10 helps. We know pregnenolone is often low (and is very important). And we know that statins show antiviral effects in many studies
![]()
Pregnenolone For Adrenal Fatigue?https://fatiguetoflourish.com/pregnenolone-for-adrenal-fatigue Here’s a common remedy for adrenal fatigue – take some pregnenolone.Ah, if only it were that simple Pregnenolone for adrenal fatigue is not the cure-all you think it is. Pregnenolone may actually make your adrenal fatigue worse! The theory known as the pregnenolone steal is not one supported by evidence. Even though most practitioners claim this to be the cause of your symptoms. Pregnenolone supplementation might actually make your adrenal fatigue worse. Today, you’ll learn everything to know about pregnenolone and adrenal fatigue. By the end of the article, you’ll know more than your practitioner! Let’s get going! Your HPA axis in actionAdrenal fatigue known today as Hypothalamic-Pituitary-Adrenal Axis dysfunction (HPA-D). When you’re stressed, who do you think interprets that signal? Your brain. Not your adrenal glands. Your brain then sends signals to your body through two distinct pathways: Through your nervesThis is known as the sympatho-adrenomedulary system. This system is used in response to periods of short-term stress. Through your HPA axisCommunication is done through a cascade of hormones. This system is used in response to periods of long-term stress.The theory of your adrenal glands fatiguing due to stress isn’t supported by the evidence. Adrenal fatigue was a simplified theory used to explain a complex series of events your body undergoes when exposed to stress. It’s your brain that’s in charge of your body’s stress response. More specifically, the HPA axis. That fatigue of yours, it’s not an adrenal problem. It’s a brain problem. Let’s see how that affects the use of pregnenolone for adrenal fatigue! Pregnena-what?Pregnenolone. Many refer to it as the mother hormone. This label comes from pregnenolone’s ability to be synthesized into so many different hormones. In order to make hormones, your body takes cholesterol and synthesizes it. The first hormone synthesized from cholesterol is often pregnenolone. To make other hormones like DHEA or testosterone, your body synthesizes the pregnenolone. Here’s a quick look at some other hormones given birth to by pregnenolone: CortisolProgesteroneDHEAAldosteroneNotice how all of the above hormones are known players in adrenal fatigue. And they all need pregnenolone in order to be synthesized. Thus, if you’re low in cortisol, it makes sense why you might think increasing pregnenolone will improve your adrenal fatigue! Pregnenolone for adrenal fatigueIf you’ve got adrenal fatigue, you probably also have low levels of DHEA. If you run the DUTCH test, you might also notice that your sex hormones are low. Hormones like progesterone or testosterone. A lot of practitioners conclude that low levels of hormones come about by way of a process known as the pregnenolone steal. Their thinking is this: All steroid hormones need pregnenolone in order to get synthesized. The high-stress situation common in adrenal fatigue will inevitably create a situation of lowered pregnenolone because it’s all being used to make cortisol. Low pregnenolone means there is less available resources to create other hormones like DHEA, testosterone, or progesterone. Said another way, in response to stress, your body needs to produce a lot of cortisol. Pregnenolone is the hormone needed to synthesize cortisol. In adrenal fatigue, your body is stealing pregnenolone in order to make more and more cortisol. This results in little pregnenolone left over for making other hormones like DHEA, progesterone, and testosterone. This is what is known as the pregnenolone steal. It’s commonly discussed in practitioner circles as a consequence of adrenal fatigue. This is why many practitioners prescribe pregnenolone. Adding more pregnenolone to your system should give more resources for other hormones, right? Nope. The pregnenolone steal isn’t a real phenomenon… Debunking the pregnenolone steal in adrenal fatigueAdrenal fatigue is a simplification of an incredibly complex process. The pregnenolone steal follows in the same vein. It’s a complex process oversimplified by the notion of simply stealing pregnenolone. Here’s why the pregnenolone steal doesn’t stand up to scientific scrutiny: Your adrenal gland consists of 3 different layers. Each of the three layers is composed of different cell types. The different cell types are responsible for secreting and synthesizing different hormones. Zona GlomerulosaThis is where the aldosterone hormone is synthesized. Zona FasciculataThis is where the cortisol hormone is synthesized. Zona ReticularisThis is where the DHEA hormone is synthesized. Cells of the Zona Glomerulosa are using cholesterol and pregnenolone to make aldosterone. Cells of the Zona Fasciculata are using cholesterol and pregnenolone to make cortisol. Cells of the Zona Reticularis are using cholesterol and pregnenolone to make DHEA. There is no known pregnenolone storage system that cells can steal from. Pregnenolone is made within the mitochondria of each cell by using cholesterol. There is also no known mechanism that allows one cell to take pregnenolone from another cell. The pregnenolone steal is an oversimplification of an incredibly complex process. It is not the way your cells operate. Consider the pregnenolone steal officially debunked. Just in case I haven’t swayed your opinion yet, allow me one more opportunity… Yet another reason why the pregnenolone steal is bogusCortisol follows something known as a diurnal rhythm. Meaning that cortisol levels fluctuate based on the natural light-dark cycle found on planet Earth. In a properly functioning HPA axis, cortisol levels surge to their highest levels shortly after waking. Cortisol then slowly declines as the day progresses. Cortisol levels should reach their lowest point of the day shortly before bed. As you sleep, cortisol levels rise and the cycle begins again the next morning. There’s a massive change in cortisol levels between when you wake up and when you go to bed. (1, 2) Levels of cortisol can decrease by almost 80%. All within a 24-hour period. If the pregnenolone steal phenomenon existed, there would be plenty of time each day with low cortisol levels. Which would allow plenty of pregnenolone to be used in synthesizing other hormones like DHEA. But that’s not what you see happening! This further illustrates that adrenal fatigue is not an adrenal problem. You cannot fix adrenal fatigue by supplementing adrenal hormones. Adrenal fatigue is a brain problem. To fix adrenal fatigue, you need to fix the brain. Next, let’s see if pregnenolone supplementation improves adrenal fatigue Does pregnenolone supplementation improve adrenal fatigue?Prescribing pregnenolone is predicated on the pregnenolone steal being an actual phenomenon. If you’re bought into the pregnenolone steal theory, then giving the body more pregnenolone makes sense. More pregnenolone means more available resources for your cells to synthesize other adrenal hormones like DHEA. But since that’s been officially debunked, does pregnenolone supplementation help adrenal fatigue patients? You need to stop thinking about adrenal fatigue as an adrenal problem. This way of thinking is furthering the issue. The interplay between your HPA axis and hormones is an incredibly complex network of events. Your HPA axis communicates via feedback inhibitions, receptor signaling, genomic regulation, heat shock proteins, and many other hard to understand processes. Your adrenal fatigue condition is not caused by low pregnenolone levels. Low pregnenolone is a symptom, not a cause. Consider the following: The simple act of having high blood sugar (hyperglycemia) leads to a massive decrease in DHEA and pregnenolone leves. Massive! In one study, praticipants DHEA levels decreased by an average of 57% only eighty minutes after a glucose injection. Pregnenolone levels also dropping by a whopping 51%. All within eighty minutes! (3) 1 in 3 North Americans have high blood sugar by way of diabetes. And another 1 in 3 North Americans have high blood sugar from pre-diabetes. That’s 2 out of 3 people in North America that likely have symptoms of adrenal fatigue. No matter how much pregnenolone you give these people, they will not feel better. You need to address the root cause. And high blood sugar is clearly one such root cause! The bottom line is this – supplementing pregnenolone may help with some of your adrenal fatigue symptoms. But low pregnenolone is not the root cause of your adrenal fatigue. Supplementing pregnenolone will not cure adrenal fatigue. You still need to identify and treat the underlying issue affecting your adrenal health. Only then can you reach a cure. Adrenal fatigue could actually be helping you…I implore you to stop thinking about adrenal fatigue as a simple hormone deficiency. Taking this or that supplement to raise hormone levels is not the approach you should be taking. Low pregnenolone, low cortisol, and low DHEA are all symptoms. They are not causes. You cannot fix the root cause of adrenal fatigue by treating simply giving hormones. To actually fix adrenal fatigue, you have to identify the underlying source or cause. To further complicate matters, adrenal fatigue can be considered a healthy adaptation by your body. In these situations, the administration of hormone therapy could actually worsen your condition. Here’s why: Cortisol is a catabolic hormone. Meaning that it breaks down tissue. No bueno. In response to inflammation, let’s say a chronic infection due to mold, your body will release cortisol. In the short-term, this is a normal and healthy response to the stress of inflammation. Cortisol is anti-inflammatory after all. But chronically high cortisol levels will cause atrophy to a specific region of your brain known as the hippocampus. (4) Yep, that’s the same part of your brain that atrophies in alzheimers disesae. The hippocampus is absolutely essential for all things memory related. In an effort to protect itself, your brain lowers cortisol levels. Said another way, adrenal fatigue could actually be protective measure. When you get all high and mighty thinking you’re going to fix this adrenal fatigue by taking hormones and supplements, you might actually be making the situation worse. Much worse. You might be contributing to the shrinking of your hippocampus! If not pregnenolone, how do you fix adrenal fatigue?By this point, if you’re not questioning everything you thought you knew about adrenal fatigue, go back and re-read the previous section. It’s so important. Using pregnenolone and other hormones/supplements to treat your adrenal fatigue may actually worsen your underlying condition. What to do? You have to find the root cause. This is absolutely essential. Before you start pregnenolone or any other hormone therapy, find what caused the lowered levels to begin with. Some of the most common root causes I see are: Blood sugar abnormalitiesThis alone causes dramatic changes to DHEA levels. Hidden sources of inflammationThink stealth infections. Things like Lyme disease, mold illness, and Ebstein Barr Virus. Using pregnenolone or any other hormone therapy before addressing the hidden infection will make you feel so much worse! To be clear, I’m not suggesting pregnenolone never be used in the treatment of adrenal fatigue. Using hormones in treatment may still be necessary. Just be sure to use hormone therapy in the proper order. This means identifying the root cause of adrenal fatigue before throwing hormones at it! Ok, now you know as much as I do about pregnenolone for adrenal fatigue! It’s time for me to hear from you. How was your experience using pregnenolone for adrenal fatigue? Did pregnenolone make your fatigue symptoms better or worse? CommentsLisaDoes fruit sugar, I am mostly talking about low sugar fruits, react that same way on blood sugar as table sugar? I have a killer sweet tooth. It is my drug of choice and I have been trying to mitigate it some by doing smoothies with protein and fruit to deal with it. MarkHi, Lisa, Great question. It totally depends on what makes the fruit sweet – glucose or fructose. Glucose will most certainly alter your blood sugar. Fructose won’t alter your blood sugar, but it will have other unwanted effects when consumed in excess. More info on that here – https://fatiguetoflourish.com/fatty-liver-foods-to-avoid/ M Dan“There is no known pregnenolone storage system that cells can steal from. Pregnenolone is made within the mitochondria of each cell by using cholesterol. There is also no known mechanism that allows one cell to take pregnenolone from another cell. ” This statement doesn’t make any sense to me. I hope you don’t mind a little criticism of your article. Supplemental Pregnenolone reliably and dramatically increases circulating levels of Progesterone, Allopregnanolone, and to a much lesser degree DHEA. All of which are products of the Adrenal gland. That alone proves that theadrenal cells (and probably gonads and brain) use circulating hormones as hormone precursors to carry out their functions. I would argue that there is no evidence that the entire adrenal cascade happens in situ in a single pass. My understanding is that pregnenolone is moved out of the cell’s mitochondria after being synthesized in order to not inhibit future pregnenolone synthesis from circulating LDLs. Pregnenolone is the most abundant neurosteroid in the brain. While it can be made from directly from cholesterol locally, almost all of the steroids produced by the adrenal glands can independently cross the BBB and be used within the brain. They play a major role in all of the dynamic and so-called plastic functions of the brain. It is for that reason that people reasonably conclude that a lack of circulating hormones reflects a lack of available hormones in the brain and nervous system. While Pregnenolone alone may not cure CFS, anyone who is living with a deficiency of cholesterol and/or pregnenolone would be well advised to supplement and replace what they are lacking. When you understand the role that pregnenolone and it’s derivatives play in your brain’s ability to function, you’ll know that there is no virtue in living with an inadequate supply. I have personally never had any success getting a doctor to take my low total cholesterol levels seriously. I’ve been told that a total cholesterol of 120 mg/dl makes me the model of perfect health. And, that my fatigue, anxiety, depression, and cognitive problems are unrelated to my cholesterol. With that kind of thinking, there is no way that any knight in shining armor is going to launch an investigation into a mystery virus or a deeper cause of my symptoms. Years ago, I was sent to an endocrinologist to test my hormones and he said that my thyroid was fine and that while my sex hormones weren’t perfect, they didn’t explain my fatigue or my cognitive symptoms. My serum AM cortisol was mid to high but my 24-hour urine cortisol was in the bottom 20% of the range. He said I didn’t have Addison’s Disease so everything was fine with him. In regards to my cholesterol he just said eat more eggs. So I left thinking that my hormones were OK, even though my cholesterol was so low. Moving forward, here in the US I can order my own labs through a variety of sources so I recently decided to order my own Pregnenolone test and it came back at 52 ng/dl (range 22-237). No doctor every bothered to check my Pregnenolone. That means I’ve likely been living for over 10 years with 25% of the Pregnenolone my brain and body need to function optimally! I just started to supplement with Preg. I used too high a dose at first and my levels went up over 500 ng/dl in the first week so I backed it way down and now they’re stabilizing at around 190 ng/dl. I have no idea how much Pregnenolone will help or how much of my symptoms have been caused or exacerbated by it’s absence. Either way though, there is no way I’m not going to maintain optimal levels because it’s one of the few things that are within my power to do. Waiting for a viral diagnosis or a CFS “root cause” before I balance my hormones is just not an option. Even after the first week I’m feeling an improvement in stamina so I’ll take what I can get. Only time will tell. Maybe I’ll check in in a few months and update. BTW, I’m not defending the Pregnenolone Steal theory, I’m just commenting on your article. Looking back at my labs it seems that I can make Cortisol on demand but that my total daily output is woefully inadequate. I think it’s reasonable to at least consider that the low cholesterol, low pregnenolone, and low cortisol output are related to each other. Since I have found no dietary way under the sun to raise my cholesterol numbers, it makes sense to boost and support the Pregnenolone since it’s easy to do. After that I’ll be looking to optimize the other adrenal hormones as well. When you say that “Using pregnenolone and other hormones/supplements to treat your adrenal fatigue may actually worsen your underlying condition.”, you should also consider that allowing your brain to remain in a steroid deficient state may also worsen your underlying condition. Choosing to wait for a deeper diagnosis to treat a known hormone deficiency seems ill advised. Sorry for such a long-winded post. Mark VolmerHey, Dan! Thanks for the comment. I agree, frank deficiencies of pregnenolone are best remedied with medication. I’m happy to hear that your condition has improved with said remedy. You can, however, run into issue in the context of chronic fatigue syndrome. CFS results from cells entering hypometabolism – something much like the dauer state of nemotodes. This is an adaptive mechanism as ribotoxins are blocking the voltage-dependent anion channel into the mitochondrial matrix. As such, the cells are left relying solely on glycolysis for ATP production – a woefully inadequate means of energy production. By taking hormone replacement like pregnenolone, you may be working against the adaptive mechanisms of your body. The resulting effect can be increased lactic acid production and an overall worsening of symptoms. Now, this is all assuming your CFS is coming by way of biotoxins. If not, I completely agree with everything you said. Thanks for the comment! M KylaHi. I was diagnosed with Adrenal Fatigue when I was 21 years old and was weaning my first child. I had very low cortisol levels and high DHEA levels. At night my cortisol was below the lowest end of normal for night time. I experienced severe mood swings, anxiety, unexplained rapid weight loss, sickness with no symptoms but just severe fatigue and an “ill” feeling. I had been diagnosed in the past with PTSD since giving birth to my first child. I could not fall asleep well nor stay asleep. I had to eat before bed to stay asleep or get up to eat in order to go back to sleep. My doctor prescribed me pregnenolone compounded 10 mg nightly. I made marked improvements. About a year and half later I was back to my old self. Fast forward 8 years and a second child later, I had a car accident, a mild one. No injuries. A few small bruises. For the next three months I was very clumsy. Sliced my fingers a few times, tripped several times. I had such severe inflammation and fascia pain I had to get massage, acupuncture, and chiropractic care twice a week for two years after the accident. Two years later I was diagnosed with hypothyroidism, positive for EBV, and fibromyalgia. I’m taking pregnenolone sublingual drops as the pills don’t seem to do anything. I feel my nervous system has been damaged. I just don’t know where to turn to for proper advice. I grew up doing well in gymnastics and sports. I’m very in tune with my body. Yet somehow I have developed scoliosis and a weakness in my right side of my body. I get unexplainable random pain in my neck or shoulder leaving my arm and hand very very cold even blue. Yet my pulse ox is normal and X-rays showed no signs of dislocation, fracture, breaks, or tears. I do have trouble detoxing. My mitochondria, I think, don’t function properly. Then again, where does this leave me? Who will listen to me or know the first step to helping me? Rheumatology didn’t see these symptoms the very day I was in her office so she dismissed me like I made it all up. Endocrinology say I was misdiagnosed with my adrenals and my thyroid. Yet if I stop medication my hair falls out, my fatigue and depression are worse, etc. It’s so frustrating! I feel like I have no one who will listen
![]()
Pregnenolone
https://www.eurohealthproject.com/pregnenolone.html
For improved memory and mental energy! Pregnenolone is important for nerve and brain health, is a potent memory and learning skill enhancer, relieves arthritis, has anti-depressant effects, relieves stress, improves mood and sense of well being, stimulates clear thinking, influences the (physic) energy levels
The Superhormone for Your Brain
Potent memory enhancer, relieves arthritis, Anti-depressant; converts to progesterone and DHEA (dehydroepiandrosterone) in the body.
What is Pregnenolone?
Pregnenolone is a natural hormone, produced primarily by the adrenal glands, but also in the brain, liver, skin, testicles and ovaries. In the body Pregnenolone is used as Pregnenolone itself, or it is converted to DHEA (dehydroepian- drosterone), which in turn is converted into Androgens (e.g. Testosterone), Estrogens and other steroids, and through another pathway, it is converted into Progesterone. Totally over 150 different steroid hormones are made from Pregnenolone in the body - it generates a whole symphony of hormones - in short "The Symphony of Life". It is interesting to note, that there is a clear difference in the metabolism of Pregnenolone in human males and females - in males the metabolic pathway seems to favor conversion into Testosterone and in females the conversion into Estrogens.
About Pregnenolone
If DHEA is referred to as "The Mother Hormone", Pregnenolone will qualify to be called "The Grandmother Hormone". Pregnenolone was first prepared in a laboratory in 1934. It has been clearly established that with age, the natural secretion of related hormones, including Pregnenolone, enzymes and other important bodily substances, drastically goes down - substances that are vital in order to have a functioning body and mind - as well as all other bodily functions do. One may ask: "What is the chicken and what is the egg, in this case?"
What Does Pregnenolone Do?
Clinical research has shown Pregnenolone to be important for nerve and brain health, having also been found to be a potent memory and learning skill enhancer - maybe the most important so far discovered. It is also known to relieve arthritis. Pregnenolone has been used in treating depression, relieving stress, improving mood and sense of well-being. Additionally, it stimulates clear thinking, improves concentration, enhances alertness and promotes an overall better mental function/alertness, all supporting improved creativity, making you think clearer and faster, keeping the brain functions at peak capacity, increasing the desire to learn and try new things. Pregnenolone also possibly influences the (psychic) energy levels. In studies Pregnenolone has been found to have a positive effect on Alzheimer’s, Multiple Sclerosis, Parkinson’s, seizures, Chronic Fatigue Syndrome (CFS), Diabetes as well as on Autoimmune disorders, such as Lupus and Scleroderma, Heart Disease, Muscle Building, the Immune System, Cholesterol levels, vision and hearing, PMS, Benign Prostate Hyperplasia, skin quality and weight loss.
Pregnenolone has also been tested with promising results in spinal cord and nerve injuries, due to accidents or disease. It is only fair to assume, that shortly Pregnenolone will prove to be instrumental in the Aging Process and Longevity and play a very important role in over-all Quality of Life. In the body Pregnenolone synthesizes into Progesterone, and via DHEA (dehydroepiandrosterone) into Testosterone and Estrogen. Further human studies are required in order to know the exact and the extent of these effects on human beings.
What are the Benefits of Supplemental Pregnenolone?
Brain
Pregnenolone plays a significant role in brain health. Because of Pregnenolone’s proven biochemical effects on the brain and the brain chemistry, it is only a fair hypothesis to make, that it would be one solution to treating diseases like: Anxiety, Obsessive-Compulsive Disorder (OBD), Dementia, Depression, Manic-depression, Alzheimer’s, Parkinson’s and aging in general, resulting in better memory, mood, well-being; peacefulness, mild euphoria, clear thinking, mental alertness, (psychic) energy, creativity, speech and vision.
Stress
Stress - no matter the source - causes elevated cortisol levels, with increased blood sugar levels, inhibition of the immune system, calcium loss (leading to osteoporosis) as a result. Pregnenolone, especially in combination with Melatonin, has proven to be very effective in relieving stress and stress symptoms.
Energy
Pregnenolone has anti-fatigue effects, both physiologically ("more pep"), as well as psychically - more mental energy.
Vision & Hearing
There are proofs that Pregnenolone provides enhanced visual and auditory perception.
Estrogen/Hormone-Replacement Therapy (ERT-HRT)
Can Pregnenolone be a replacement for traditional ERT/HRT?! Research indicates that this may be the case, especially together with DHEA (dehydroepiandrosterone), and complemented with human female hormones. The trick is to find the individual right combination of the supplemental hormones (Pregnenolone, DHEA, Melatonin, etc.) and the replacement hormones (e.g. Estrone, Estriol, Estradiol) and the ratio of the two types. More research is no doubt needed, but we have after all come a long way and the general information given in the literature, presented in this brochure, must be considered as "safe and efficacious".
Arthritis & Autoimmune disorders
Treatment with Pregnenolone has shown marked clinical improvement in patients with Ankylosing Spondylitis, Lupus, Osteo- and Rheumatoid Arthritis and Scleroderma.
Neurological Help
Pregnenolone has also been used in treating Alzheimer’s Disease, Multiple Sclerosis (MS), nerve injuries, Parkinson’s Disease and seizures.
Depression
Pregnenolone has been successfully used in counteracting all types of depression.
Other Indications
Pregnenolone has been used in the treatment of Chronic Fatigue Syndrome/"CFS", Addison Disease, high cholesterol levels, Immune System-deficiencies and skin conditions.
Anti-Aging/General Health and Well Being/Quality of Life/Longevity
Regardless of whether Pregnenolone lengthens the lifespan, it is evident that it does have some important therapeutic application, and used wisely, it may improve the Quality of Life and postpone signs of aging or the aging process itself, while improving general health and sense of well-being. A great deal of research is underway and it will give us answers about the effects of long-term use.
Pregnenolone is Safe to Use
No serious side effects or risks have been reported in association with taking supplemental Pregnenolone in recommended doses (see below). Neither has any toxicity been seen even in dosages several times greater than the generally recommended dose, given over a long period of time.
Pregnenolone seems to be compatible with - and causes no negative (drug-) reactions whatsoever - all and any prescription drug, other dietary supplement, natural products and foods, when taken in recommended dosage.
Pregnenolone and DHEA in Combination
Although Pregnenolone is a precursor to Progesterone and DHEA, which in turn is a precursor to several other hormones, e.g. all of our sex hormones (Testosterone, Estrogen, only to name a few), it is important to understand, that the conversion rate of Pregnenolone to these hormones is slowed down even more with age, than the actual production in the body of the hormones themselves. When we age, the enzymes secreted by the body governing the conversion of Pregnenolone to DHEA, is secreted at an even slower rate, than the applicable hormone secretions themselves. Therefore a "Hormone Cocktail"/a mix of these hormones is preferable, as we age. Both Pregnenolone (mainly for "its own" function as Pregnenolone - memory/mental alertness, mood/well-being, arthritis and for nerve/spine cell stimulation/regeneration) and DHEA (for its many well known important and beneficial physiological functions) can - and in most cases should - be taken together in recommended dosages.
What is recommended Intake?
Unless otherwise prescribed by a physician, only individuals over the age of 40 should be taking this product, as the levels of Pregnenolone prior to that age are usually sufficient. Take 10-50 mg daily, or according to doctor’s prescription. Take capsule in the morning on an empty stomach. For long-term continuous usage a physician should be consulted to establish the correct daily dosage. For healthy adults, 10 mg is recommended for people of 40 years of age, 25 mg for people over 50 years of age and 50 mg for people over 60 years of age, as general guidelines. Blood levels of Pregnenolone should be measured regularly - especially in younger subjects - to determine if supplementation is appropriate and a physician should monitor the dosages
view detailed PDF
![]()
Pregnenolone sulfate to help with symptoms
https://www.healthrising.org/forums/threads/pregnenolone-sulfate-to-help-with-symptoms.6319
User Chfrazzle
I was reading about how Pregnenolone sulfate, which is an over the counter supplement, was being used in a ME/CFS study and it's reaction upon or in conjunction with Natural Killer cells. To be honest the study was far beyond my comprehension and the researchers did more than administer the Pregnenolone sulfate by itself. But the article made me curious if anyone has tried Pregnenolone Sulfate for their fatigue?
According to verywellmind.com:
"Pregnenolone is a steroid hormone that plays a key role in the production of other steroid hormones, including progesterone, DHEA, and estrogen. The substance is found naturally in the body, but some people also take it in supplement form to help
keep memory sharp through the years."
User jaminhealth
Many years ago when I started with an Integrative MD the first test he did was to test DHEA levels, I was about 60 at the time....they were LOW and this is true as we age, we decline/deplete DHEA. So I've been taking DHEA for over 20 yrs and it's changed my life and kept me VITAL and too too bad every doc doesn't go there with their patients... Pregnenolone is a precursor to DHEA...so I'm guessing you are low in DHEA so why not start taking say 10mg day, it's OTC and go from there...eventually get your DHEA level tested.
Allopathic MD's really short change Everyone in getting to the root of issues.
I knew I posted about DHEA, it's a favorite topic of mine...it's another supplement that has been life changing.
Reminder: DHEA Restoration Therapy
I know there are smatterings of DHEA info around here but here is a reminder: I know supplementing with this DHEA for about 20 yrs has kept this 81 yr body younger and healthier. https://www.lifeextension.com/Protocols/Metabolic-Health/Dhea-Restoration/
User Chfrazzle
I agree, we have been short changed and forced to be our own advocate. Hard to do when you feel like #$@! Thank goodness for groups like this. I see my primary dr in a few months. It would probably be a good idea to get tested. What changed for you when you added the DHEA? Did you have any side effects from taking it? I am prone to anxiety so don't like to rock the boat too much once I get it under control.
User jaminhealth
Read the benefits of getting DHEA levels optimal. I am plain and simple, more vital as I am aging. Work on your anxiety issues, do some talk therapy if need be, and look at Inositol which is of the B family of vitamins. Work on changing your mind, it can change your life

back to top
back to top
back to top
back to top
back to top
back to top
back to top
back to top












