Vitamin D Supplements Review (Including Calcium,
Vitamin K, Magnesium, and Boron)
Find the Best Vitamin D
Supplement. Tests and Reviews of Popular Vitamin D Supplements & CL's Top
Picks.
Medically reviewed and
edited by Tod Cooperman, M.D. 
Last Updated![]() : 12/06/2021 | Initially Posted:
11/23/2019Latest Update: Vitamin D Affected by Medication
: 12/06/2021 | Initially Posted:
11/23/2019Latest Update: Vitamin D Affected by Medication

Table of Contents
Summary
·
What does vitamin D do? There are many reasons to make sure
you're getting sufficient vitamin D: These include improved bone health,
reduced risk of heart attack and stroke, reduced risk of asthma and allergy,
reduced inflammation, and perhaps others. Not surprisingly, over given periods
of time there are fewer deaths among people who have the right amount of
vitamin D compared to those who have too little or too much. For details,
see What It Does >>
·
How much vitamin D do I need? You may already get enough vitamin D
from the sun (about 15 minutes to the face, arms,
and hands at least twice a week without sunscreen) and the foods you normally eat. If you're not
sure, get your blood level checked by your doctor. A total serum
25-hydroxyvitamin D level of at least 20 ng/mL is considered
"sufficient," although there may be additional benefit to being in
the 25 to 35 ng/mL range. Don't exceed 39 ng/mL. Be aware that people who are
Black generally have lower total vitamin D levels than whites, but new research
suggests these lower levels may be sufficient for Blacks. For details see How Much Do You Need and How Much is Too Much? >>
·
What form of vitamin D is best? Vitamin D2 or D3 will raise your vitamin D level, but D3 is preferable as it may raise levels
more effectively over time and is less likely to cause erroneously low vitamin D blood test
results.
·
How much vitamin D should I take? For every 1 ng/mL
increase, you'll need to get an additional 100 IU of vitamin D per day (obese
individuals may require double the amount). For example, if your blood level is
18 ng/mL, taking 400 IU of vitamin D daily (or 800 IU if you are obese) should
get you to about 22 ng/mL. It can take 6 weeks to reach the peak. Keep taking
the vitamin D to stay at that level. For details, see What to Consider When Using >>
·
When to take vitamin D: Take vitamin D supplements with your
biggest meal of the day (the one that contains most fats and oils) as this can
increase absorption by as much as 50%! For details, see Take Vitamin D with Food >>
·
Top Picks for vitamin D: Choose a supplement
that has been Approved by ConsumerLab.com in the table below because not all supplements
live up to their ingredient claims (See What CL Found). Also, see CL's Top Picks for
those offering the best value, dose, and convenience.
·
Don't overdo it! Vitamin D safety and side effects: Studies show that
people with the highest levels of vitamin D actually tend to have more bone
fractures, fall more frequently, sleep less well, and die sooner than those
with lower, but sufficient, levels. If your level is over 20 ng/mL, you
probably don't need a supplement. If your level is above 35 ng/mL, taking a
supplement may be doing more harm than good, so consider cutting back. For
details see How Much Do You Need and How Much is Too Much? >>
What It Is:
Vitamin
D is a fat-soluble vitamin. There are two major forms of vitamin D found in
food and supplements: D2 (ergocalciferol)
and D3 (cholecalciferol).
Both vitamin D2 and D3 appear to be absorbed with equal
efficiency, and both can raise levels of 25-hydroxyvitamin D (also known as
calcifediol or calcidiol), which is the prehormone form of vitamin D and a
clinical measure of vitamin D status. However, there is evidence that D3 may be more efficient at raising
25-hydroxyvitamin D levels than D2 (see "D2 or D3?").
There is also evidence that calcifediol can raise 25-hydroxyvitamin D levels
more efficiently than D3 (see "D3 or calcifediol?"). Be aware,
however, that calcifediol is only sold as a prescription drug in the U.S., as
is also the case with the active hormone form of vitamin D, calcitriol.
However, calcifediol can be found in animal-based foods, as it is present in animal
muscle and adipose (fat) tissue.
Vitamin D3 is produced
naturally in human skin exposed to ultraviolet B light and occurs in some
animal products, such as cod liver oil, and, in smaller amounts, in other fatty
(oily) fish such as herrings, mackerel, sardines, and salmon. Vitamin D3 is the most common form used in dietary
supplements and is the form generally used to fortify foods such as milk (which
naturally contains a small amount of vitamin D3). Vitamin D3 is made by the conversion of cholesterol
compounds, such as 7-dehydroxycholesterol from lanolin found in sheep's wool.
Vitamin D2 is made by the
conversion of a sterol found in plants and yeast. Vitamin D2 is used in some dietary supplements.
See ConsumerTips™ for more information about
the two forms of vitamin D and dosing.
(See separate reviews of Calcium and Vitamin K, which are
also used in bone health).
What It Does:
Bone and fractures
Vitamin D regulates the amount of calcium and phosphorus in the body, partly by
controlling their levels of absorption. Vitamin D treats and prevents rickets
in children and osteomalacia (bone softening) in adults. However, as discussed
below, benefits of vitamin D supplementation on bone appear generally limited
to people deficient in vitamin D, i.e., having blood levels below 20
ng/mL. A study of 81 vitamin D trials went so far as
to conclude that "vitamin D supplementation does not prevent fractures or
falls, or have clinically meaningful effects on bone mineral density" --
but this study did not analyze results according to the vitamin D status of
trial participants and the study authors acknowledged that "trials in
individuals with marked vitamin D deficiency... might produce different
results." (Bolland, Lancet Diab & Endocrin
2018).
In children:
Given to breast-fed infants, vitamin D may help increase bone density.
In girls ages 9 to 13, regular supplementation with
calcium and vitamin D has been shown to significantly increase bone density and
bone strength (measured in arms and legs) compared to placebo (Greene, Osteoporosis Int 2011). Similarly, in
girls ages 10 to 17, supplementation with vitamin D for one year significantly
improved bone mineral density in their hips. This effect was not seen among
boys of the same age (Al-Shaar, Bone 2013). It
is notable, however, that 83% of the girls and 80% of the boys in this study in
Lebanon were deficient in vitamin D (below 20 ng/mL) to start. In fact, 34% of
the girls started with levels below 10 ng/mL. Two different doses of vitamin D3 were used in the study, a low dose
(1,400 IU) or a high dose (14,000 IU), each given weekly. Interestingly,
greater improvements were seen with the lower dose, although the differences
were not statistically significant.
One study suggests that children whose mothers supplement with high-dose
vitamin D during pregnancy may have a reduced risk of tooth enamel
defects (but not dental carries, i.e., cavities) (see the Pregnancy section for details).
In adults:
Taken with calcium, vitamin D can help decrease
post-menopausal bone loss and prevent osteoporosis (loss of bone
density), as well as improve tooth retention in the
elderly. However, if a person's blood level of vitamin D is already
close to or above 20 ng/mL, taking a vitamin D supplement provides no further
bone benefit. This was demonstrated in a placebo-controlled study of a
group of white, postmenopausal women in New York with an average vitamin D
level above 20 ng/mL (but below 30 ng/mL). Taking 4,000 IU of vitamin D3 daily for 6 months did not reduce bone
loss in these women (based on measurements of bone turnover markers which occur
in the blood) (Aloia, J Clin Endocrin Metab 2013).
In the same study, some of the women were given high-dose calcium
supplementation (1,200 mg from calcium carbonate, as 600 mg twice a day). Those
who received the calcium showed signs of reduced bone loss during the study --
regardless of whether they received the vitamin D supplement. This benefit is
likely due to the fact that the women, on average, were not getting the
recommended daily intake of calcium before supplementation (their average
intake was 900 mg, while the recommended daily intake for women their age is
1,200 mg). It is possible that a lower dose of calcium would also have been beneficial,
as well as safer: Too much calcium from supplements has been associated with a
higher risk of kidney stones and stroke (see Calcium Review -- Concerns and
Cautions).
In a study among older women (average age 67) with blood
levels of vitamin D averaging 19 mg/mL, daily doses of vitamin D ranging from
400 IU to 4,800 IU were not associated with a significant effect on bone
mineral density compared to placebo. During the study, all of the women
maintained a total calcium intake of 1,200 mg per day from food and/or calcium
supplements (Smith, J Intern Med 2018).
(Another analysis of the same study, discussed in the Muscle, Balance and Falls section below,
found that the rate of falls was lowest in women who achieved vitamin D blood
levels of 32-38 ng/mL after supplementation — but women with higher blood
levels had the highest rate of falls.)
Another placebo-controlled study in post-menopausal women
compared the effectiveness of 800 IU of vitamin D3 daily (400 IU twice a day) to the same
daily dose plus an additional 20,000 IU twice a week. Both groups also received
1,000 mg of calcium daily (500 mg twice a day from calcium carbonate). After
one year, bone mineral density was unchanged or slightly improved in both
groups. Markers of bone turnover (bone loss) in blood serum were also reduced
in both groups, but the higher dose was actually less efficient at
reducing bone turnover, contrary to what the researchers had expected (Grimnes, Osteoporos Int 2012).
Similarly, a study of postmenopausal women in Wisconsin
found no beneficial effect on bone mineral density from giving vitamin D at
low-dose (800 IU daily) or high-dose (800 IU daily plus 50,000 IU twice
monthly) for 1 year, compared to placebo. There was also no beneficial effect
on muscle function, muscle mass, or falls, and only a small effect on calcium
absorption. Women in the study started with a median vitamin D blood level of
21 ng/mL and, during the study, averaged 19, 28, and 56 ng/mL, respectively, in
the placebo, low-, and high-dose groups. The women in this study had adequate
calcium intake. The researchers concluded that the findings did not support
"experts' recommendations" to maintain levels of 30 ng/mL or higher in
postmenopausal women, but did support the Institute of Medicine's recommended
level of at least 20 ng/mL (Hansen, JAMA 2015).
A study in the U.S. among 687 older men and women (average age 63) with
sufficient blood levels of vitamin D, most of whom had some degree of bone
loss, showed that taking 2,000 IU of vitamin D3 daily for two years did not
increase bone mineral density or improve bone structure compared to placebo.
Supplementation increased average blood levels of vitamin D from 27 ng/mL to 39
ng/mL. Calcium intakes were not reported, but 17% of the participants reported
using a calcium supplement and, among these, there was less bone mineral density
loss in the neck of the femur if they were taking vitamin D versus placebo but
there was no benefit in whole body bone mineral density (LeBoff, J Bone Miner Res 2020).
Although not all studies have shown a benefit of vitamin D supplementation in
reducing fractures, a review of several studies concluded that
supplementation with 800 IU or more of vitamin D was "somewhat
favorable" in the prevention of hip fracture and any nonvertebral fracture
in people 65 years of age or older.39 Most notably, it found a 30% reduction in hip fracture
among people taking 792 to 2,000 IU of vitamin D per day compared to those
taking no vitamin D or small amounts (up to 360 IU per day). The review also
suggested that vitamin D blood levels above 24 ng/mL are most beneficial for
reducing the risk of both hip and nonvertebral fractures, and frequent dosing
of vitamin D (such as daily or weekly) is more beneficial than annual
dosing. Similarly, a large study of men aged 70 to 97 years in Sydney,
Australia found that those with vitamin D levels between 24 and 29 ng/mL were
least likely to suffer bone fractures. In comparison to this group, men with
lower levels (at or below 14.4 ng/mL) and higher levels (above 29.2 ng/mL)
were, respectively, 3.5 and 2.7 times as likely to experience a fracture —
suggesting a potential risk from too little, as well as too much, vitamin D in
the body (Bleicher, J Bone and Min Res 2014).
Middle-aged and older women who follow a vegan diet and do
not supplement with calcium and vitamin D were found to have three
times the risk of hip fracture compared to women who
are not vegetarians, while women who follow a vegan diet but take supplemental
calcium and vitamin D did not have an increased risk, according to a large
study of men and women age 42 or older. No association between calcium and
vitamin D supplementation and hip fracture risk was found in men who follow a
vegan diet (Thorpe, Am J Clin Nutr 2021). (See the Calcium Supplements Review for more
details.)
Be aware that vitamin D deficiency may impede healing
from fractures, as was reported in a 44-year-old man in the Netherlands
whose femoral (thighbone) fracture failed to heal four years after the initial
injury despite multiple surgeries to properly set the bone. He was found to
have severe vitamin D deficiency (25(OH)D of 4 ng/mL) and diagnosed with
hyperparathyroidism due to vitamin D deficiency and low dietary calcium intake.
He was given weekly injections of 50,000 IU of vitamin D for six weeks, after
which he took 400 IU of oral vitamin D and 500 mg of calcium daily. Eight
months after supplementation began, his vitamin D levels were sufficient (24
ng/mL) and his fracture healed (Moonen, Nutrition 2021).
In healing fractures, improving one's vitamin D level alone
is insufficient if calcium intake is inadequate, as shown in a study in the
Netherlands of 32 postmenopausal women (average age 65) with wrist fractures
who had low levels of vitamin D (average 25(OH)D of 17 ng/mL) and inadequate
intake of calcium (average 715 mg per day, compared to the 1,200 mg per day
recommended for women in this age group). They were divided into three groups
and given one oral dose of either 30,000 IU or 75,000 IU of vitamin D, which
was repeated six weeks later, or no vitamin supplementation. None of the groups
received calcium supplementation. Despite increasing their levels to 20 ng/mL
and 23 ng/mL, respectively, their fractures healed no better than those in
women who did not receive vitamin D. In fact, the higher dose of vitamin D
(equivalent to 1,800 IU per day) resulted in poorer bone
healing than in the control group. (As noted elsewhere in this Review, large
single doses of vitamin D have been shown to be detrimental.) There were no
differences in self-reported pain or function between the lower and higher dose
groups or the control group. (Heyer, J Bone Miner Res 2021).
Vitamin D may reduce aging of bones. Compared to bone samples from
the hips of people with vitamin D blood levels of 20 ng/mL or higher, bone from
those with levels below 20 ng/mL (i.e., deficient in vitamin D) were found to
be more brittle (over-mineralized) on the inside while thicker and
under-mineralized on the outside. When physically tested, bone from vitamin
D-deficient people was 22% more likely to crack and the cracks were longer
compared to bone from people not deficient in vitamin D. The researchers
believe that osteoclast cells, which normally keep bone healthy, cannot get
through the thick, under-mineralized outer layer of bone formed in vitamin
D-deficient people and, as a result, areas of bone under this layer continue to
age and over-mineralize even as the overall bone mineral content progressively
decreases (Busse, Sci Transl Med 2013).
Vitamin D levels below 10 ng/mL (severe deficiency) were associated with more
severe lumbosacral disc degeneration and low back pain among
232 postmenopausal women in China compared to those with levels of 30 ng/mL.
There was no significant difference in disc degeneration between those with
levels of 10 - 30 ng/mL versus levels above 30 ng/mL, leading the researchers to
speculate that only extremely low vitamin D levels affect disc degeneration.
However, those with levels between 10 - 30 ng/mL were more likely to have
moderate to severe low back pain, and other predictors of back pain were
smoking, higher BMI (body mass index), lack of vitamin D supplementation, and
osteoporosis (Xu, Menopause 2020).
Muscle, balance, and falls
In older adults:
A review of 13 studies found that vitamin D supplements (800 to 1,000 IU daily)
may improve balance and muscle strength, but not gait, among older adults.30 The benefits of taking vitamin D,
however, may depend on whether or not a person has insufficient levels to
start. Too much vitamin D may even have negative effects, including increasing
the risk of falls that result in fractures.
A placebo-controlled, six-month study among older men
and women (average age 73) in Lebanon with low skeletal muscle mass who also
had very low blood levels of vitamin D (averaging 10 ng/mL) found that
increasing blood levels of vitamin D to 28 ng/mL (by giving 10,000 IU of
vitamin D three times a week -- a high dose) significantly increased muscle
mass in the arms and legs, although it did not increase hand-grip strength. The
increase in muscle mass was greater in normal-weight individuals than in those
who were obese (Hajj, Arch Osteoporos 2018).
One of the best studies of vitamin D and falls focused on
women with insufficient levels of vitamin D (blood levels less than 20 ng/mL)
who had not taken vitamin D supplements and were getting only about 120 IU
daily of vitamin D from their diets. They were divided into groups given 400
IU, 800 IU, 1,600 IU, 3,200 IU, 4,000 IU, or 4,800 IU of vitamin D3 or a placebo. Over the course of one
year, 58% of those given the placebo had fallen, but those given 1,600 to 3,200
IU of vitamin D3 had the lowest rate
of falls — just 30%. Those given lower or higher doses did not fall
significantly less than the placebo group. Women ending with blood levels of
32-38 ng/mL had the lowest rate of falls (21%), while the highest rate of falls
(72%) was among those with levels of 38 to 46 ng/mL. In short, those who
received enough vitamin D to correct insufficiencies but remained under 40
ng/mL fared best (Smith, J Steroid Biochem Mol Biol
2017). The researchers suggested that the current upper limit on
vitamin D intake of 4,000 IU daily should be lowered to 2,000 IU to reduce the
risk of falls. Similarly, a study in Denmark among
women with hyperparathyroidism and low vitamin D levels (averaging 12.4 ng/mL)
found that giving 2,800 IU of vitamin D3 daily for 3 months increased vitamin D levels to 36 ng/mL
and lowered the elevated parathyroid hormone levels but reduced maximal
handgrip strength by 9%, knee flexion strength by 13%, and slowed
performance on a "Timed Up and Go" test as compared to
results for women given placebo. The researchers cautioned against relatively
high daily doses of vitamin D in treating vitamin D insufficiency (Bislev, Calcif Tissue Int 2018). Additional
analysis of data from this study suggested that the loss in muscle strength
could be due to a "direct detrimental effect" of moderately high
doses of vitamin D on skeletal muscles. In contrast to women given placebo, the
women supplemented with vitamin D developed increased blood levels of several
compounds associated with muscle breakdown (carnitine, choline, and urea), as
well as a tendency towards increased serum levels of TMAO and urinary
creatinine, which can also occur with muscle breakdown (Bislev, Nutrients 2020).
A study among 688 older men and women (average age 77) with
elevated fall risk (e.g., balance or walking problems or a history of falls)
and 25(OH) vitamin D blood levels averaging 22 ng/mL found that doses of 1,000
IU or higher (2,000 or 4,000 IU) taken daily for two years did not prevent
falls compared with 200 IU. In fact, those who took 1,000 IU or more had an 87%
increased risk of a serious fall (resulting in fracture or dislocation) and
148% increased risk of a fall requiring hospitalization compared to those who
took just 200 IU per day (whose blood levels rose, on average, to 27 ng/mL vs
32, 35, and 48 6 ng/mL, respectively, for the 1,000, 2,000, and 4,000 IU
groups). A major contributor to the findings was an unusually high rate of
adverse events in the 2,000 and 4,000 IU groups during the first year of the
study (Appel, Ann Intern Med 2020). Further
analysis of data from the same study showed that participants who took 1,000 IU
or more of vitamin D were also 166% more likely to have a first-time fall
resulting in a fracture, although not more likely to have a greater number of
falls, compared to those taking 200 IU per day or not taking vitamin D at all (Wanigatunga, J Am Geriatr Soc 2021).
A small study of women aged 65 years and older with somewhat limited mobility
found that those given a capsule of 4,000 IU of vitamin D3 daily after breakfast for 4 months
experienced a 10% increase in muscle fiber size (measured at the thigh)
compared to those given placebo (Ceglia, J Clin Endocrin Metab 2013). The
supplemented group also experienced a 30% increase in vitamin D receptors in
muscle cells, suggesting an effect on muscle metabolism and/or function. There
was no effect, however, on physical functioning (balance, walking, rising) or
knee extension power — although the study did not involve increased exercise.
The women chosen for the study had moderately low vitamin D levels (mean of
18.5 ng/mL) which rose in the supplemented group to 32 ng/mL. (Note: 4,000 IU
per day is a large dose at the upper tolerable intake limit; however,
absorption was probably somewhat reduced as the vitamin was taken after
breakfast rather than with a larger meal).
A 9-month study in younger postmenopausal Brazilian women
(ages 50 to 65) known to be deficient in vitamin D (averaging 15 ng/mL) and
with a history of falls found that a daily dose of 1,000 IU (given as liquid
drops) increased the average level to 27.5 ng/mL and was associated with a
25.3% increase in muscle strength of the lower limbs, as demonstrated by chair
rising test, but no increase in handgrip strength. Although there was no
exercise component of the study, women receiving the vitamin D maintained lean
mass (muscle) while women in the placebo group lost lean mass (Cangussu, Osteoporos Int 2015). It was separately reported that the rate of falls during the study
was 46% higher for those receiving placebo rather than vitamin D, and the
researchers calculated that, after adjusting for variables, the risk of a fall
was actually 90% greater in the placebo group and the risk of recurrent falls
was 180% greater (Cangussu, N Am Menopause Soc
Meeting Abstract 2015, p. 67). Similarly,
giving 800 IU of vitamin D daily to postmenopausal women in Turkey who were
deficient in vitamin D (average level of 10 ng/mL) resulted in small but
statistically significant increases in muscle strength in the hamstring and
quadriceps. In contrast, women in the study who were, instead, given a single,
very high dose (300,000 IU) of vitamin D did not have a statistically
significant improvement despite a greater rise in their vitamin D levels even
through the end of the 12 week study (Apaydin, BMC Endocr Disor 2018).
In contrast, a study in women aged 70 and older who were at risk for bone
fracture showed an increase in falls and fractures among those
given an extremely high, single, annual dose (500,000 IU) of vitamin D3.10 This unexpected finding may have
resulted from unusual effects of the extreme dose.11 A higher rate of falls
with higher-dose vitamin D3 was also found in a study of community-dwelling men
and women 70 years of age and older with a prior fall -- 58% of whom were
vitamin D deficient (i.e., blood levels under 20 ng/mL) (Bischoff-Ferrari, 2016).
The study compared a monthly dose of 24,000 IU of vitamin D (equivalent to 800
IU per day) to two higher doses: 60,000 IU or 24,000 IU with 300 mcg of
calcifediol — a vitamin D metabolite which is 2 to 3 times more potent than
vitamin D3 (Jetter, Bone 2014).
Although the higher-doses raised vitamin D levels more than the lower dose,
they had no benefit on lower extremity function and were each associated with
an increased risk of falls over the course of a year (about
66% fell) compared with the lower dose (47.9% fell). Seniors who were not
deficient in vitamin D but were given 60,000 IU per month experienced the most
falls, and people whose levels reached 44.7 - 98.9 ng/mL had nearly twice
as many falls as those whose levels reached 21.3 to 30.3 ng/mL.
Too high a dose of vitamin D may actually weaken leg muscles,
as shown in a one-year study of overweight and obese women (with a mean vitamin
D blood levels of 21.4 ng/mL) given 2,000 IU of vitamin D3 per day or placebo
in conjunction with a reduced calorie diet and moderate to vigorous aerobic
activity. Over the course of the year, leg strength significantly
decreased in the vitamin D group (-2.5 pounds decrease in lifting
weight) while it increased slightly in the placebo group (+1.8 pounds). There
were no significant differences between the groups in changes in lean body mass
or bone mineral density of the spine and femoral neck (Mason, JAGS 2016). The same study found no
benefit on weight loss between the groups, as reported earlier (see
"Weight loss control" below). Mean vitamin D levels in the treated
group rose by 13.6 ng/mL to 35 ng/mL while it fell in the untreated group b 1.3
ng/mL to 20.1 ng/mL -- which is still above the cut-off for insufficiency
(under 20 ng/mL).
In a study among homebound older adults, more than half of
whom had insufficient (< 20 ng/mL) blood levels of vitamin D and had
reported having fallen in the previous year, a monthly dose of 100,000 IU
vitamin D3 taken for 5 months increased vitamin D blood levels to sufficient
levels in all but one person, and reduced the number of falls over the 5 months
by approximately half, compared to placebo. One weakness of the study, however,
is that the researchers knew who received the vitamin D3 and who received a
placebo (Houston, J Am Geriatrics Soc 2015).
A large observational study among older men in England
suggests that having very low blood levels of vitamin D may increase the risk
of orthostatic hypotension (low blood pressure when standing), a
condition that is associated with an increased risk of falls and fractures (Mol, J Am Med Dir Assoc 2019; Hamrefors, PLoS One 2016).
The study, among 3,620 men (average age 69), found that vitamin D deficiency
(< 10 ng/mL) was associated with a 51% increased risk of orthostatic
hypotension. Vitamin D levels were measured as total vitamin D (25OHD2 plus
25OHD3) (Gilani, Age Ageing 2020). However,
giving vitamin D (1,000, 2,000, or 4,000 IU daily) to older adults with
orthostatic hypotension did not help reduce orthostatic symptoms (such as
lightheadedness, dizziness, seeing spots, imbalance, headache, etc.) compared
to taking 200 IU of vitamin D3 daily. The study participants had vitamin D
levels ranging from 10 to 29 ng/mL (Juraschek, Circulation 2021).
Interestingly, a preliminary study in teenage girls with orthostatic instability
suggested a possible benefit of vitamin D supplementation.
Several studies have shown that vitamin D supplementation in older women who
already have sufficient levels of vitamin D (at least 20 ng/mL) does not
improve balance or strength:
·
A study of women aged 70 to 80 in Finland who generally had
sufficient vitamin D levels (averaging 25 ng/mL), showed that taking vitamin D3
(800 IU daily) for 2 years did not reduce falls, injuries from falls, or
physical functioning. In fact, compared to those given placebo, the women who
received vitamin D actually showed a decline in a "get up and go"
test. Average blood levels of vitamin D rose to 37 ng/mL among those receiving
vitamin D. In the study, some of the women were enrolled in physical training
classes once or twice week and performed exercises at home (5 to 15 minutes) on
the other days. Compared to women who did not train, the exercisers experienced
less than half the number of injurious falls and injured fallers, although
there was no decrease in the number of falls. The exercisers also showed
improved muscle strength, balance and mobility, although exercisers treated
with vitamin D showed smaller benefits than exercisers receiving placebo.
Vitamin D did have a small effect on reducing bone loss in the hip and
increasing bone density in the lower leg, but this did not translate into other
benefits (Uusi-Rasi, JAMA Intern Med 2015).
·
A year-long study in Norway among postmenopausal women (ages 50
to 80) with generally sufficient blood levels of vitamin D (averaging about 25
ng/mL) and osteopenia (reduced bone density) or osteoporosis, found that
neither high-dose vitamin D supplementation (800 IU D3 daily + 20,000 IU twice
weekly) nor supplementation with a lower dose (800 IU D3 daily + placebo),
improved muscular strength, balance or quality of life (Grimnes, Clin Endocrinol (Oxf) 2017). Women in
both the high and lower-dose groups also took 1,000 mg of calcium daily.
·
A 3-year study among older African-American women (average age
68) who were generally not vitamin D deficient found that increasing blood
levels of vitamin D to an average of 47 ng/mL with high-dose vitamin D
supplementation (3,600 IU median daily dose) did not decrease
the risk of falls compared to women who took a placebo and maintained an
average blood level of 21 ng/mL (Aloia, J Am Geriatr Soc 2019).
·
A large, 5-year, placebo-controlled study in Australia found
that monthly, high-dose (60,000 IU) vitamin D3 did not reduce
the risk and incidence of falls among men and women ages 60 to 84, most of whom
already had more than adequate blood levels of vitamin D at the beginning of
study. If fact, there was a 25% increased risk of falls among
normal-weight participants (BMI < 25 kg/m2) given vitamin compared to those who were overweight or obese
(BMI > 25 kg/m2). The researchers
speculated that people with less body fat (where vitamin can be stored) may
have higher circulating levels of vitamin D when taking high doses compared to
those with more body fat (Waterhouse, J Cachexia Sarcopenia
Muscle 2021).
The bottom line from
these studies appears to be that vitamin D may increase muscle mass in older
individuals with very low levels of vitamin D. It may also help may help with
balance and reduce falls in women with insufficient levels of vitamin D (below
20 ng/mL), but may do little or have negative effects in women with already
sufficient levels. In older men, vitamin D deficiency may increase the risk of
orthostatic hypotension, which is a risk factor for falls and fractures, but it
is not known if vitamin D supplementation helps prevent falls due to this
condition. Not surprisingly, exercise can be extremely effective in reducing
the risk of injury from falls.
In younger adults:
A review of seven clinical trials (from 2010 to 2013) in
healthy adults aged 18 to 40 concluded that vitamin D supplementation increased
upper and lower limb strength. It is important to note that the vast majority
of subjects in these studies were deficient in vitamin D (average blood level
was only 12.3 ng/mL), many of whom were in India, where deficiency is more
common than in the U.S. High doses (2,000 IU per day to 60,000 IU per week)
were used in the studies, which lasted 4 weeks to 6 months. It is not clear whether
these results are relevant to a population with adequate levels of vitamin D.
As noted in the review, vitamin D receptors are found on skeletal muscle and
these receptors are involved in protein synthesis within the muscle, possibly
explaining these findings (and those for older individuals -- discussed above)
(Tomlinson, J Sci and Med in Sport 2015).
However, not all studies have found a benefit in younger
adults with low or deficient blood levels of vitamin D. A study in Estonia
among 39 previously untrained men (average age 23) with low blood levels of
vitamin D (averaging 14 ng/mL as 25(OH)D) who began a strength training program
(3 sessions per week, supplementing with 20 grams of whey protein after each
session), taking 8,000 IU (200 mcg) of vitamin D3 daily for three months did
not increase training-induced gains in muscle strength or lean body mass
compared to strength training plus placebo, despite raising average blood
levels to 57 ng/mL 25(OH)D. In fact, men who took the placebo (and had low
blood levels of vitamin D throughout training) had greater gains in muscle
strength in two of the seven strength exercises performed (chest press and
seated row) compared to those who took vitamin D. The researchers suggested
that benefits might only occur in people with severe deficiency (< 10 ng/mL)
and the very high dose vitamin D given may actually block the
activity of vitamin D receptors (as pointed out by other researchers) (Savolainen, Eur J Appl Physiol 2021).
No increase in muscle strength occurred in a
placebo-controlled study of slightly older, active adults (average age 44) in
Japan, although lean body mass (i.e., muscle) increased by 1 lb. Participants
were initially deficient in vitamin D and were given 420 IU (10.5 mcg) of
vitamin D3 daily, raising blood levels from an average of 13 ng/mL to 24 ng/mL
(Sun, Ann Nutr Metab 2019).
Two small studies of U.S. professional football players
found associations between lower levels of vitamin D and injuries. A study of
players on the Pittsburgh Steelers found that the mean vitamin D level among
players who suffered a muscle injury was 19.9 ng/mL, while players with no
muscle injury had a mean level of 24.7 ng/mL (Shindle, AOSSM 2011 abstract p. 56).
A study of players on the New York Giants found vitamin D levels significantly
lower in those with at least one bone fracture when compared with levels in
those with no fractures after accounting for the number of seasons played. In
addition, players who were released during the preseason because of either
injury or poor performance had significantly lower vitamin D levels (62% were
below 20 ng/mL) than did players who played in the regular season (11% were
below 20 ng/mL) (Maroon, Am J Sports Med 2015).
(The team names were not disclosed in the studies, but were identified in
a Wall Street Journal article).
In children and adolescents:
Orthostatic intolerance (OI), which can cause dizziness or
fainting upon standing, can affect children and adolescents. OI includes
conditions such as orthostatic hypotension, vasovagal syndrome, and postural
tachycardia syndrome (POTS). A small study among teenage girls (average age 16)
with OI and vitamin D levels averaging 22 ng/mL (i.e., at the lower end of
adequate) found that taking 2,000 to 5,000 IU of vitamin D daily for two months
increased vitamin D levels to 41 ng/mL on average and increased the amount of
time the girls could tolerate standing on head-up tilt by about 15 minutes.
Heart rate variability when standing on tilt was also increased after vitamin D
treatment, which suggests the body was under less stress. Baroreflex
sensitivity, a measure of how well the heart rate adapts to changes in blood
pressure, also improved after supplementation with vitamin D. However, the
study did not include a control group, so it's not possible to conclude that
vitamin D supplementation improves OI (Shaltout, Hypertension 2020).
As noted earlier, very low levels of vitamin D have been associated with
orthostatic hypotension (a form of OI) in older men.
Benign Paroxysmal Positional Vertigo (BPPV)
BPPV is a common form of vertigo that is caused by
displacement of calcium carbonate crystals (otoliths) within the inner ear.
There is a hypothesis that vitamin D deficiency may reduce the density of these
crystals, increasing the risk of their displacement, and a study in England
found that BPPV was more common in months when levels of vitamin D (measured as
25-hydroxyvitamin D) are lower (March, April and May). A preliminary study
among 10 women in Portugal with a history of BPPV and generally low vitamin D
blood levels evaluated the effect of giving vitamin D on BPPV episodes. Half
the women were given 5,000 IU of vitamin D daily if their starting levels were
below 20 ng/mL, or 800 IU per day (given as a single monthly dose) if their
levels were 20 ng/mL or higher. Over 12 months, the vitamin D blood levels in
these women rose to an average of 32.1 ng/mL and none experienced BPPV. The
other women did not receive vitamin D and each experienced 1 to 3 episodes of
BPPV, suggesting a possible protective role of vitamin D supplementation
against recurrence of BPPV (Matos Carniero de Sousa, Hear Bal
Comm 2019).
Further
evidence of a protective role of supplementation was provided by a larger study
among 957 people in South Korea (average age 62) recently treated (with a
repositioning maneuver) for BPPV. In the study, people in the intervention
group were evaluated for serum levels of vitamin D at baseline, and those with
levels less than 20 ng/mL were given 400 IU of vitamin D and 500 mg of calcium
carbonate twice daily for 12 months. People in the observation group were not
evaluated for vitamin D status or given supplementation. Both groups were
followed for about one year, although data was considered for any person who
had been followed up for at least one month. People in the intervention group
had a 24% lower rate of BPPV recurrence compared to those in the observation
group, with greatest benefit seen for patients in the treatment group who had
been vitamin D deficient (25-hydroxyvitamin D levels <10 ng/mL) (Jeong, Neurology 2020). It
appears that supplementation with vitamin D, with or without calcium, may
reduce recurrent episodes of BPPV in people who have low levels of vitamin D.
Overactive bladder and
urinary incontinence
Low blood levels of vitamin D have been associated with higher risk of
overactive bladder (OAB) (i.e., suffering from urinary urgency or frequency
with or without incontinence) (Yoo, BJU Int 2018), possibly explained by the
role of vitamin D in muscle function (Parker-Autry, Int Urogynecol J 2012). A small
study in Jordan, for example, found that people with severe vitamin D
deficiency (below 10 ng/mL) were 32 times more likely to have
overactive bladder symptoms than people with levels above 30 ng/mL. No rigorous
studies have been conducted to determine if vitamin D is beneficial in OAB, but
the same Jordanian researchers gave vitamin D (50,000 IU weekly for 4 to 8
weeks) with encouragement to increase dietary calcium intake to 13 people with
OAB (11 of whom had vitamin D levels below 20 ng/mL) in whom drug therapies had
not been successful. The vast majority of these patients reported improvements
in nighttime and daytime urinary symptoms, although it is impossible to
evaluate the clinical significance of these results as there was no placebo or
other scientific control (Abdul-Razzak, Neurourology and
Urodynamic, 2019). A study among 56 women
(average age 60) with urgency urinary incontinence found that, overall, vitamin
D supplementation (50,000 IU weekly for three months) did not improve
bladder symptoms, pelvic floor muscle function, or functional status compared
to placebo, although it should be noted that most of the women who took vitamin
D had sufficient blood levels before supplementation. A sub-group analysis
found a significant decrease in the number of incontinence episodes per day
among Black women who took vitamin D compared to placebo (-63% vs. -22%).
During the study, average blood levels of vitamin D increased from 21 ng/mL to
58 ng/mL among those who took vitamin D (Markland, J Am Geriatr Soc 2019).
Statin drugs and vitamin D
If you use a statin medication for cholesterol-lowering, it may very helpful
to maintain sufficient blood levels of vitamin D for the following reasons:
Statins may work better when vitamin D is adequate:
A 6-month, placebo-controlled study in China among people with high cholesterol
and treated with statin drugs found that taking 2,000 IU of vitamin D3 tablets significantly improved
cholesterol levels. Approximately half the people in the study began with
vitamin D blood levels below 20 ng/mL (i.e., vitamin D deficient) and about
another quarter had levels between 20 and 30 ng/mL. Mean vitamin D blood levels
increased by 17.1 ng/mL in the treated group and by 2.4 ng/mL in the placebo
group (due to increased sun exposure because the study ended in June). Compared
to the placebo group, which experienced slight improvements in cholesterol
levels, total cholesterol levels in the treated group fell by an additional
22.1 ng/mL, triglycerides fell by 28.2 mg/dL, LDL ("bad") cholesterol
fell by 20.2 mg/dL, and HDL ("good") cholesterol increased by 8.2
mg/dL. Improvements were greater when excluding those who began the study with
vitamin D levels of 30 ng/mL or higher (no analysis was reported of just those
who had been vitamin D deficient). The researchers noted that these results
with vitamin D may be limited to statin-treated patients (Qin, Clin Nutr 2015).
Note — Giving high-dose vitamin D to people who are not deficient
may slightly increase cholesterol levels (see Concerns and Cautions).
Statin-related muscle pain less likely with when
vitamin D is adequate:
The risk of developing muscle pain (myalgia) and inflammation (myositis) while
taking cholesterol-lowering statin drugs appears to be greater when people have
lower levels of vitamin D (and keep in mind that severe vitamin D deficiency
itself -- regardless of statin use -- can cause bone pain and muscle weakness).
A study found that, among statin users, the average vitamin D level among those
without myalgia was 34.9 ng/mL, while the average among those with myalgia was
28.4 ng/mL (Michalska-Kasiczak, Int J Cardiol
2015). A small study of people who suffered muscle pain while on
statins and had generally blood levels of vitamin D averaging 22 to 23 ng/mL
evaluated the effects of giving very large weekly doses of vitamin D2, ranging from 50,000 to 100,000 IU, with a
goal of boosting vitamin D levels to 50 to 80 ng/mL. The researchers concluded
that 88% to 95% of patients were able to tolerate statins without muscle pain
at various time points in the study, although these percentages ignore those
who had dropped out at earlier points due to renewed muscle pain. Over two
years, 44 of the 146 patients (30%) experienced myalgia-myositis and stopped
statin treatment, and 70% were symptom free. The study was not double-blind,
lower doses were not tried, and, likely for ethical reasons, there was no
control group (i.e., patients not given vitamin D but restarted on statins) (Khayznikov, N Am J Med Sci 2015). As noted in Concerns and Cautions, the dosage of vitamin D
used in this study is very high and could be associated long-term safety risks.
However, based on the evidence, it would seem worthwhile to make sure you have
adequate vitamin D levels if taking a statin.
Statin-related decline in exercise performance is blunted when vitamin D is
adequate:
While statins can lessen improvements in cardiorespiratory fitness that
normally occur with exercise as well as reduce the content of mitochondria
(i.e., the "energy powerhouses") in muscle cells, vitamin D adequacy
may lessen these negative effects. A study in India among 28 people with type 2
diabetes who were vitamin D deficient (averaging about 10 ng/mL) found that,
after 12 weeks of performing moderate aerobic exercise, those given simvastatin
(40 mg daily) had an 8.4% decrease in cardiovascular fitness, but if also given
vitamin D (60,000 IU weekly — which is a very high dose), the decrease was only
0.6%. Skeletal muscle mitochondrial content decreased 3.6% with simvastatin but
improved 12.1% if vitamin D was also given. Vitamin D alone, without
simvastatin, increased cardiovascular fitness and mitochondrial content by 7.1%
and 16.7%, respectively (Singla, J Diabetes 2017).
More vitamin D is needed to raise blood levels when taking a statin:
A review of clinical trials in which vitamin D was given to people aged 60 and
over with low vitamin D levels found that statin users had a 21.4% smaller
increase in vitamin D blood levels than people not using statins (Bischoff-Ferrari, JAGS 2017). It would seem
advisable to use a slightly higher than normal dose of vitamin D if you are
taking a statin.
Vitamin D levels may increase or decrease depending on the statin:
In small clinical trials, certain statin medications have been shown to
increase blood levels of vitamin D, while other stains have been shown to have
little effect or to slightly decrease blood levels of vitamin D — possibly due
to enzymes involved in metabolizing these drugs or whether the drugs are more
soluble in fats or water. Rosuvastatin (Crestor) was shown to
increase 25(OH)D levels by 22.3 ng/mL and 1,25-dihydroxyvitamin D (the active
form) by 3.7 pg/dL when taken daily for 8 weeks (Yavuz, Cardiovasc Drugs Ther 2009), although
not all studies have found a large an impact. This was also seen in a separate
study by the same research group in which rosuvastatin (10 mg/day) taken daily
for two months increased 25(OH)D blood levels by about 23 ng/mL (from 11.8 to
35.2 ng/mL); however, the same study found that fluvastatin (Lescol XL),
taken at a dose of 80 mg per day, had no effect on vitamin D
levels (Ertugrul, Cardiovasc Ther 2011).
Atorvastatin (Lipitor) appears to have a more modest effect on
vitamin D levels, although results from clinical trials have been inconsistent.
A study in Spain found that either a low (10 mg to 20 mg) or higher (40 mg to
80 mg) daily doses of atorvastatin for one year led to modest increases in
25(OH)D blood levels (about 3 ng/mL) (Perez-Castrillon, Am J Cardiol 2007). However,
a study in India found that atorvastatin (10 mg/day) taken for six months
caused a small but significant reduction in 25(OH)D blood levels (about 2
ng/mL), while those taking rosuvastatin (5 mg/day) showed an increase in
25(OH)D levels, although the increase was modest (about 2 ng/mL) compared to
the studies described above. The researchers noted that atorvastatin is a
stronger inducer (i.e. it enhances activity) of an enzyme (CYP3A4) involved in
the breakdown of 25(OH)D, possibly explaining the reduction (Patwardhan, Indian J Pharmacol 2020).
There is some evidence that 20 to 80 mg of lovastatin (Mevacor) daily
increases 25(OH)D blood levels, while it seems that simvastatin (Zocor) either
increases or has little effect on vitamin D levels (Gupta, Atherosclerosis 2011).
Back pain
A study among overweight and obese adults in Australia with back pain who also
were deficient in vitamin D (levels below 20 ng/mL) found that high-dose
vitamin D significantly reduced back pain among those who were severely
deficient (levels below 12 ng/mL), but not among those with levels
above 12 ng/mL. Vitamin D was given as an initial 100,000 IU dose followed by
4,000 IU per day for 16 weeks, boosting levels, on average, by 22 ng/mL (Brady, J Ster Biochem Mol Biol 2018).
[Note: Obese individuals require larger doses of
vitamin D to raise levels.]
Rheumatoid arthritis
Low levels of vitamin D are associated with a higher risk of developing rheumatoid
arthritis and may be associated with more significant disease severity
and progression. These associations do not prove a cause-and-effect
relationship.
A study in China found the mean level of serum vitamin D in men and women with
rheumatoid arthritis to be 17.2 ng/mL, while it was 23.2 ng/mL in a matched
control group of healthy individuals. Among the patients with arthritis, lower
vitamin D levels were associated with higher rates of swollen joint, tender
joint, joint pain, and morning stiffness, as well as osteopenia and
osteoporosis (Hong Rheumatology 2014).
A study in France among 643 people with early rheumatoid
arthritis found that disease activity and severity was worse at baseline for
those with vitamin D deficiency (<10 ng/mL) compared to those with higher
levels. Vitamin D deficiency was also associated with a 70% greater chance of
functional disability at 6 months, as well as 90% greater chance of
radiographic progression and erosion progression at 12 months (Mouterde, J Rheumatol 2020).
Osteoarthritis (worn joints)
Giving vitamin D3 to people with
painful osteoarthritis of the knee was not found to improve
symptoms nor slow progression of the disease more than giving a placebo,
according to a two-year study in Boston (McAlindon, JAMA 2013).
In fact, throughout the study, those given vitamin D were more likely to report
using non-steroidal anti-inflammatory drugs (e.g., ibuprofen) than patients
given placebo. However, most patients who participated in the study were not
deficient in vitamin D to begin with -- the average starting blood
level of 22.7 ng/mL. Vitamin D was given at an initial dose of 2,000 IU daily
and then adjusted, primarily upward, to achieve levels over 36 ng/mL. Only the
subset of people who began the study deficient in vitamin D (levels below 15
ng/mL) experienced improvement taking vitamin D, although this improvement
could not be considered statistically significant due to the small size of this
group.
Similarly, a large three-year study among people aged 50
years and older in the UK with knee osteoarthritis given 800 IU daily of
vitamin D3 showed no benefit compared to placebo with regard to progressive
narrowing of the joint space, mobility, function, or pain. The average starting
blood level of vitamin D was just slightly above 20 ng/mL, with half the
individuals under that amount and, therefore, deficient in vitamin D. However,
unlike the study above, further analysis did not show better results for those
who started the study deficient in vitamin D compared to those who were not (Arden, Osteoarth Cartilge 2016).
A two-year study in Australia found that knee joint pain
decreased by 36% in a group treated with vitamin D3 (50,000 IU per month: equal to 1,667 IU
per day) but this was not found to be statistically significant because pain
declined 26% among those given placebo. Both groups lost knee cartilage volume
during the study but the loss was slightly less in the vitamin D group --
although not to a significant degree. Unlike the Boston study above, many
patients in this study were deficient in vitamin D, with a mean level of 17.5
ng/mL, which, by the end of the study, was over 24 ng/mL in 79% of those
treated with vitamin D and 43% of those receiving placebo. Although not an
original endpoint of the study, there was a statistically significant
improvement in joint function for the vitamin D group compared to placebo.
Interestingly, while improvements plateaued in the placebo group after 1 year,
symptoms continued to improve in the vitamin D group through the second year (Jin, JAMA, 2016). A
later analysis of the same two-year study looked at the effects of vitamin D
supplementation on foot pain and related disability, which is
common in people with knee osteoarthritis and associated with more severe knee
pain. The analysis showed modest improvements in foot pain and disability in
the vitamin D treatment group that maintained blood levels of 20 to 30 ng/mL.
Although small, these improvements were, statistically, significantly better
than the general lack of improvement seen in the placebo group as well as in
those in the treatment group who did not maintain blood levels of at least 20
ng/mL (Tu, Arthritis Care Res (Hoboken) 2020).
These studies suggest that vitamin D supplementation does not benefit
osteoarthritis of the knee in people not deficient in vitamin D, while the
evidence is mixed on whether it may help those who are deficient in vitamin D.
Cardiovascular disease, blood pressure, and cholesterol
As discussed below, several studies have shown increased
risk of cardiovascular disease associated with lower blood levels of vitamin D
(i.e., lower than 15 to 20 ng/mL). Studies in which vitamin D has been given to
such people with low levels have shown cardiovascular benefits (e.g., small
improvements in blood pressure, cholesterol, arterial stiffness) with regular,
moderate doses (600 to 1,000 IU), but generally less benefit and even side
effects with higher doses (2,000 IU daily or 100,000 IU monthly or quarterly).
There appears to be no cardiovascular benefit giving high-dose vitamin D to
people with blood levels already above 15 to 20 ng/mL.
A major study (the VITAL study) of a cross-section of
middle-aged Americans given 2,000 IU of vitamin D daily for a median of 5.3
years found no overall reduction in cardiovascular events (heart attack,
stroke, or death from cardiovascular causes) relative to placebo. However,
participants were not deficient in vitamin D — the average
starting blood level was 30.8 ng/mL, which increased to over 40 ng/mL among
those given vitamin D during the study (Manson, NEJM 2018).
Similarly, a study in England gave 2,000 or 4,000 IU of vitamin D, or a
placebo, daily for one year to over 300 generally healthy older people with
average vitamin D blood levels of 20 ng/mL -- about 10% of whom were already
taking 400 IU of vitamin D or more daily. Although blood levels of vitamin D
more than doubled, there was no significant effect on blood pressure, heart
rate, arterial stiffness, echocardiogram measures, cardiac function, or blood
levels of prohormone that regulates blood pressure (Tomson, J Am Heart Assoc 2017).
On the other hand, an earlier analysis of two large studies showed that men who
consumed 600 IU or more per day of vitamin D from foods and supplements were
16% less likely to have cardiovascular disease and stroke over
a period of approximately 20 years compared to men consuming less than 100 IU
per day. The same association was not seen among women; the reason for this is
unclear but one possible explanation given is that women may need higher intake
of vitamin D because they tend to have a higher percentage of body fat than men
and vitamin D is fat soluble. In addition, vitamin D intake during the study
period, which ended in 2006, may have been too low to produce meaningful
differences.21
Research has found that men with low levels of vitamin D in the blood (15 ng/mL
and lower) are at increased risk for heart attack compared to
those with levels at 30 ng/mL and higher, even after adjusting for other risk
factors and physical activity. Similarly, in a study lasting about 6 years,
adults with vitamin D levels below 30 ng/mL were more likely like to suffer
from hypertension, coronary artery disease, cardiomyopathy,
and diabetes than those with higher levels.32 In fact, after adjusting for other
factors, the risk of death from all causes was 164% higher
among those with the lower levels of vitamin D. The researchers note that 71%
of people in the study (involving over 10,000 people in Kansas) had serum
vitamin D levels below 30 ng/mL — the mean was 24.1 ng/mL. Among those with
levels below 30 ng/mL, the risk of death was reduced if a vitamin D supplement
was being taken; however, there was no such additional advantage with
supplementation for those with levels already above 30 ng/mL. The researchers
did not analyze the results by further subgroups of vitamin D level. A study that followed 230,000 men and women (average age
48) in the southwest U.S. for 5 years applied different vitamin D level
subgroupings and found that the risk of cardiovascular disease was 35% higher
for those with vitamin D levels below 15 ng/mL (9% of the studied population)
compared to those with higher levels (Muhlestein, Circulation 2015).
Although the apparent benefit of avoiding vitamin D deficiency appears
dramatic, there is potential downside from much higher levels (see How Much Do You Need and "How Much is Too
Much?" for more about mortality rates and vitamin D).
Research suggests that long-term, high-dose vitamin D
supplementation does not improve mortality rates, and
may worsen certain outcomes, in people with chronic
heart failure, despite modest improvements in heart output reported in one
study. In that trial, 163 people in the UK with chronic heart failure (less
than half the normal ventricular output) were given high-dose (4,000 IU)
vitamin D3 or placebo daily
for 1 year, with the primary goal of increasing walking distance in a 6-minute
test. All of the patients started the study with vitamin D levels below 20
ng/mL. Among those given vitamin D, blood levels of vitamin D generally rose to
about 50 ng/mL, however, there was no increase in walking distance -- which
actually decreased by 4%, while it increased by 4% among those
given placebo. Those taking vitamin D did, however, experience a modest but
statistically greater improvement in heart output (left ventricular ejection
fraction increased from 25.6% at baseline to 33.3%, while, in the placebo
group, it increased from 26.5% at baseline to only 27.9%) (Witte, J Am Coll Cardiol 2016).
[ConsumerLab.com Comment: The high dose given in this study caused patients to
achieve unusually high vitamin D blood levels -- levels associated with increased falls in
other studies, possibly explaining the reduction in walking distance despite
improved heart output. A lower but still higher than normal dose (e.g., 2,000
IU) could have achieved vitamin D sufficiency and may have improved heart
output as well as improved walking distance.]
A placebo-controlled study in Germany among 400 people
with advanced heart failure and low blood levels of vitamin D found that 4,000
IU of vitamin D given daily for three years increased median blood levels of
25(OH)D from 14 ng/mL to 37 ng/mL but did not reduce mortality and increased
the need for mechanical circulatory support (MCS) implants (used to manage
reduced heart output) and hospitalization (Zittermann, Eur Heart J 2017).
Researchers followed the participants for an additional three years after
supplementation ended (during which blood levels of vitamin D would have likely
decreased) and found that those previously treated with vitamin D were no
longer at increased risk of requiring an MCS implant or hospitalization,
further suggesting that high-dose supplementation had a detrimental effect (Zittermann, ESC Heart Failure 2020).
Low levels of vitamin D are generally associated with elevated
blood pressure. However, studies have, at best, only shown a modest
reduction in blood pressure when vitamin D is given. A comprehensive review of
46 trials concluded that vitamin D is ineffective for lowering blood pressure,
regardless of starting levels of vitamin D in the blood, and should not be used
as antihypertensive agent -- although most patients with hypertension in the
analyzed studies were also being treated with antihypertensive medication,
possibly obscuring an effect of vitamin D (Beveridge, JAMA Intern Med 2015). One trial
which found no effect was conducted among adults age 70 and older with systolic
hypertension. The participants, most of whom were also taking anti-hypertension
medication, were given 100,000 IU of vitamin D3 every three months (equaling
1,100 IU per day) for one year, raising the mean vitamin D blood level from 18
ng/mL to 28 ng/mL. Vitamin D supplementation failed to improve hypertension or
other measures of cardiovascular health, including cholesterol levels (Witham, JAMA 2013).
However, another placebo-controlled study using a dose of 2,000 IU of vitamin
D3 daily for 6 months found that those receiving vitamin D supplementation
experienced reductions in systolic and diastolic blood pressures of,
respectively, 6.2 mm Hg and 4.2 mm Hg compared to those not receiving vitamin
D. People in the study were all taking nifedipine (a calcium channel blocker).
Among those receiving vitamin D, mean vitamin D blood levels rose from 19.4
ng/mL to 34.1 ng/mL (Chen, Atherosclerosis 2014).
Be aware that one study found vitamin D deficiency to be associated with low
blood pressure upon standing (known as orthostatic hypotension) in older
men (see Muscle, balance and falls for details).
A 12-week study in Iran of overweight and obese premenopausal women found that
daily supplementation for 12 weeks with 1,000 IU vitamin D3 increased HDL
("good") cholesterol by 7%. However, total
cholesterol increased 1.7% and there was also a 4% increase in LDL
("bad") cholesterol — although it contained less ApoB, suggesting
less plaque-forming ability. Interestingly, body fat decreased
by 9.6% (about 6 lbs), although total body weight was unchanged.31 A larger and longer
(2 year) study in the U.S. found that postmenopausal women given 400 IU of
vitamin D3 and 1,000 mg of calcium (from calcium carbonate), taken in two
divided doses daily, experienced a 4.5 mg/dL decrease in LDL cholesterol
compared to those who received a placebo. Vitamin D blood levels rose to a mean
of 24.3 ng/mL among the supplemented women compared to 18.2 ng/mL in the
placebo group. Although there was no statistically significant effect of taking
the supplement on total cholesterol, HDL, or triglycerides, the researchers did
find that women with higher blood levels of vitamin D tended to have higher
levels of HDL and lower levels of both triglycerides and LDL (Schnatz, Menopause 2014).
A small study of obese adolescents given a monthly dose of
100,000 IU of vitamin D3 for 3 months (averaging 3,333 IU per day) showed no
improvement in arterial function and insulin and glucose levels, and increases
of 32% and 9%, respectively, in triglycerides and total cholesterol. A weakness
of the study was that few participants had been deficient in vitamin D (below
20 ng/mL), with the average starting level of 22 ng/mL, which increased to 35
ng/mL (Javed, Pediatric Obesity 2015). A large placebo-controlled study giving 100,000 IU of vitamin
D3 monthly to older adults (average age of 66), for approximately 3 years found
no reduction in cardiovascular events even among a subgroup who started the
study deficient in vitamin D (blood levels below 20 ng/mL) (Scragg, JAMA Cardio 2017). However, a 16-week study among overweight African-Americans with
vitamin D deficiency (blood levels averaging about 15 ng/mL), found that high
doses of vitamin D (60,000 IU or 120,000 IU given once-a-month -- each of which
raised levels to about 35 ng/mL) improved (i.e., reduced) arterial stiffness by
about 8 to 10%. A lower dose (18,000 IU per month) did not have this effect
despite raising the levels to an average to 23 ng/mL. The study did not assess
effects on cardiovascular disease (Raed, PLOSOne 2017).
Diabetes, insulin resistance and glucose control
Maintaining a vitamin D level of at least 25 or 26 ng/mL or moderately
higher may reduce insulin resistance and may improve blood sugar control in
people at risk for or with diabetes, although not all studies have found a
benefit.
Risk of type 1 diabetes
Higher serum levels of vitamin D — up to a point -- have been
associated with a lower risk of developing type 1 diabetes (i.e.,
requiring insulin). In a study of two thousand people on active duty in the
military, those with vitamin D levels between 24 and 31 ng/mL had the lowest
risk of being diagnosed with type 1 diabetes. Compared to this group, the risk
of diabetes was more than 2.5 times as great among those with levels between 17
and 24 ng/mL, and the risk was more than 3.5 times as great among those with
levels below 17 ng/mL. No risk reduction was associated with levels above 31
ng/mL — in fact, the risk of diabetes was slightly higher for those with levels
above 31 ng/mL than those with levels between 24 and 31 ng/mL (Gorham, Diabetologia 2012).
Observational data suggests that dietary intake of vitamin D is associated with
lower risk of developing type 1 diabetes (Hypponen, Lancet 2001). It has been suggested
that to reduce the risk of type 1 diabetes, infants and children receive
supplemental vitamin D if they have limited sun exposure, live in northern
areas, are exclusively breastfed, or are dark skinned (Harris, J Nutr 2005).
Insulin resistance and prediabetes
Obesity itself is a major risk factor for insulin resistance, but too little
vitamin D may increase the risk. A study found that obese individuals with
vitamin D blood levels below 20 ng/mL were 12 times more likely to be insulin
resistant than obese individuals with sufficient levels of vitamin D (Kabadi, Diabetes Care 2012) . In addition, a
study of overweight and obese women who were not diabetic found that vitamin D
blood levels of at least 26 ng/mL appear to be needed for normal glucose
metabolism in both Black and white women, and those with this amount of vitamin
D had lower body fat, blood glucose, insulin and triglyceride levels than women
with lower levels of vitamin D (Sorkin, JN 2014).
Furthermore, a study of 115 overweight older adults in Lebanon
with low average blood levels of vitamin D (10 ng/mL) but who did not have
diabetes (although 14 were considered to be pre-diabetic) found that 10,000 IU
of vitamin D3 taken three times per week for six months modestly reduced
insulin resistance (as measured by HOMA-IR) from an average of 2.63 to 2.4, and
decreased fasting blood sugar levels, compared to placebo (Hajj, J Nutr Health Aging 2018). However, a placebo-controlled trial among 64 men and women in
Ireland with prediabetes and low blood levels of vitamin D found that high-dose
vitamin D (3,000 IU daily for six months) did not improve
blood sugar control or insulin function despite increasing vitamin D blood
levels from an average of 12 ng/mL to 40 ng/mL (Wallace, Am J Clin Nutr 2019).
Maintaining adequate blood levels of vitamin D may also have a
beneficial effect on blood sugar and insulin levels in healthy people who are
not overweight: A study among 81 healthy men and women in Japan, most of whom
had low or deficient blood levels of vitamin D (average blood level 13 ng/mL)
found that, compared to placebo, 420 IU of vitamin D3 taken daily for one year
increased average blood levels of vitamin D to an average of 24 ng/mL,
decreased fasting blood glucose (from an average of 88.3 mg/dL to 85.3 mg/dL),
and improved insulin resistance values (as measured by HOMA-IR) from 1.17 to
0.84 (Sun, Nutr Res 2016).
One study found the risk of developing type 2 diabetes was 43% lower among
individuals with vitamin D levels over 25 ng/mL compared to those with levels
under 14 ng/mL (Mitri, Eur J Clin Nutr 2011).
A study in India among men and women with prediabetes and very low blood levels
of vitamin D (averaging 10 ng/mL) found that oral supplementation with 60,000
IU of vitamin D3 after breakfast once a week (equivalent to about 2,140 IU
daily) for three months improved insulin sensitivity (measured by the insulin
sensitivity (OGIS) index) compared to placebo. However, there were no
improvements in the insulin-sensitivity check index (QUICKI), HOMA-IR, nor in
fasting or post-meal blood sugar levels compared to placebo. Interestingly,
average vitamin D blood levels in those who took vitamin D increased to 52
ng/mL, which is above the level at which the risk of adverse effects may
increase (Ahmed, Cureus 2020).
Supplementing people at risk of type 2 diabetes who are not
deficient in vitamin D does not reduce the incidence of type 2 diabetes, as was
shown in a large, placebo-controlled 2.5 year study in which people with
pre-diabetes took 4,000 IU of vitamin D daily, raising the average level from
27.7 ng/mL to 54.3 ng/mL. However, among the subgroup of people who started the
study with vitamin D levels below 12 ng/mL, those given vitamin D were 62%
less likely to develop type 2 diabetes than those given placebo — a
major difference (Pittas, NEJM 2019). A
placebo-controlled study among older men and women at high risk of diabetes or
newly diagnosed type 2 diabetes with vitamin D levels averaging 21 ng/mL (45%
of whom were below 20 ng/mL, i.e., vitamin D deficient) found that
supplementation for 6 months with 5,000 IU daily of vitamin D significantly
improved peripheral (i.e., in muscles) insulin sensitivity although not hepatic
sensitivity, i.e., there was no improvement in insulin secretion, glucose
levels, or HbA1C (Lemieux, Eur J Endocrin 2019).
In people with type 2 diabetes
Among people with type 2 diabetes with vitamin D levels of 20 ng/mL or higher,
vitamin D supplementation may not provide benefit (Mitri, Eur J Clin Nutr 2011). In fact, a large
U.S.-based trial found that giving high-dose vitamin D (4,000 IU daily) for 48
weeks to people with stable type 2 diabetes who were not vitamin D deficient
(average starting level was 27 ng/mL) did not improve any measure of blood
sugar control (Angellotti, J Endocrine Society
2018). Also see "Depression" below for more about type 2
diabetes and vitamin D.)
A study in Denmark found that both high and low vitamin D levels
are associated with a form of nerve damage called cardiovascular
autonomic neuropathy (CAN) in people with type 1 and type 2 diabetes.
CAN affects heart rate and blood vessel function and may cause low blood
pressure on standing and exercise intolerance. Patients with CAN have a greater
chance of having a heart attack and lower chance of surviving one. The findings
suggest that beneficial effects of vitamin D are restricted to a specific serum
range (around 20 ng/mL to 50 ng/mL) and both too low and too high levels are
detrimental to the autonomic nervous system (Hansen, Diabetic Med 2016).This
may help explain similar associations found between vitamin D levels and falls as well as mortality.
Gestational diabetes
Supplementation with a combination vitamin D
and calcium may improve blood sugar control in pregnant women with gestational
diabetes. In a six-week study of 56 women with gestational diabetes (at 24
to 28 weeks gestation), those who received 1,000 mg calcium per day, plus
50,000 IU of vitamin D3 at the beginning of the study and another 50,000 IU at
week 3, had significantly lower fasting blood glucose levels compared to those
given placebo (respectively, a 0.89 mmol/l reduction versus a 0.26 mmol/l
increase), lower serum insulin levels (-13.55 vs. +9.17 pmol/l), and a
significant increase in insulin sensitivity (+0.02 vs -0.002 ) (Asemi, Diabetologia 2014).
Non-alcoholic fatty liver disease (NAFLD):
Low levels of vitamin D have been associated with non-alcoholic fatty liver
disease -- the accumulation of fat in the liver (also called hepatic steatosis)
which can lead to inflammation, scarring and cirrhosis (Elaides, Aliment Pharmacol Ther 2013). NAFLD
affects approximately 30% of Americans. A preliminary study in 40 women and men
with significant liver fat accumulation and insufficient blood levels of
vitamin D (averaging 11.8 ng/mL) found that with a weekly dose of 20,000 IU of
vitamin D3 (equivalent to about 2,857 IU per day), liver fattiness decreased by
approximately 5% after only four weeks; while vitamin levels rose to an average
of about 35 ng/mL. A weakness of this study, however, is that it did not
include a control group (Papaostoli, J Gastrointestin Liver
Dis 2016). A study of adults with NAFLD
with vitamin D blood levels below 30 ng/mL given 2,000 IU of vitamin D daily
for six months found that levels rose above 30 ng/mL in most (75%) of those who
did not have liver inflammation but in only 15% of those with inflammation
(known as steatohepatitis). Only those whose levels increased showed
significant improvements in plasma ALT levels (an indicator of liver function)
and HOMA-IR scores (an assessment of insulin resistance). Higher doses of
vitamin D may be necessary to sufficiently raise vitamin D levels in such
people (Dasarathy, J of Nutr 2017).
Inflammation
Raising low levels of vitamin D may also reduce inflammation in the body. In a
study of blood from thousands of adult Americans, levels of C-reactive protein
(CRP), a marker of inflammation, decreased as vitamin D levels increased to
just below 21 ng/mL28 However, there was
no further benefit when vitamin D levels reached and exceeded 21 ng/mL. In
fact, after adjusting for cardiovascular risk factors, it was found that CRP
levels slowly but progressively increased at that point, suggesting
a slight inflammatory action of vitamin D at
these higher levels. The results seem to reinforce the importance of
maintaining a plasma vitamin D level of at least 20 ng/mL and suggest some
potential downside of higher levels of vitamin D.
Somewhat similar conclusions were drawn from a
well-controlled, 1-year study of vitamin D in adults aged 60 to 84 years in
Australia. Starting with vitamin D levels of about 17 ng/mL, people were given
monthly dose of vitamin D of 30,000 IU (equal to 1,000 IU/day), 60,000 IU, or a
placebo. At 1 year, there were no significant differences in levels of
inflammatory biomarkers in the treated groups versus placebo — except for a
slight increase in a pro-inflammatory marker (IL-6) in the higher-dosed group,
half of whom achieved vitamin D blood levels of 30 ng/mL or higher. The
researchers note that this may suggest a detrimental effect of higher vitamin D
levels (Waterhouse, Br J Nutr 2015).
Vitamin D appears to accelerate the resolution of
inflammatory responses during tuberculosis therapy.42 In a study in London, patients given
very large doses of vitamin D3 (100,000 IU every 2 weeks) along with standard
antibiotic therapy had less inflammation, and their infections cleared 13 days
earlier on average, than patients who did not receive vitamin D. It is
important to note, however, the very high prevalence of profound vitamin D
deficiency in the studied population -- more than half the patients had levels
of vitamin D below 8 ng/mL prior to therapy. Added vitamin D may not yield the
same benefits for patients who already have sufficient levels of vitamin D.
Asthma
Moderate doses of vitamin D may improve symptoms of asthma in children as
well as in adults with uncontrolled asthma. However, improvements seem to be
limited to those with very low vitamin D levels, e.g. less than 10 ng/mL.
A review of medical studies published from 1950 to 2009 that looked at, among
other variables, vitamin D intake and asthma, suggested that vitamin D
deficiency may be linked to airway inflammation, decreased lung function and
poor asthma control. The researchers conducting the review hypothesized that
vitamin D supplementation may lead to improved asthma control, although this
cannot be established as many of the studies were not specifically designed to
test the effects of vitamin D supplementation on patients with asthma (Urashima, Am J Clin Nutr 2010). A clinical
study published in 2014 tested whether high-dose vitamin D supplementation
reduced treatment failures among adults with asthma already receiving an
inhaled corticosteroid (ciclesonide) and a bronchodilator (levalbuterol).
Vitamin D supplementation (4,000 IU per day after an initial 100,000 IU dose)
did not lead to a statistically significant reduction in initial treatment
failures compared to those receiving a placebo supplement. However, during the
28-week study, the group receiving vitamin D was 20% less likely to have a
treatment failure and 37% less likely to have an exacerbation of symptoms. It
is possible that more significant results may have been obtained if the study
did not have certain weaknesses: Half the patients started the study with
vitamin D levels above 20 ng/mL and, therefore, were not vitamin D deficient
and might not benefit from additional vitamin D; and, because of the very high
dosage used in the study, many of these people may have achieved unusually high
blood levels of vitamin D which other studies suggest may counter beneficial
effects of vitamin D (Castro, JAMA 2014). Further analysis of this
group found no benefit regarding colds -- see Denlinger study, below). A small pilot
study (not placebo-controlled) tested a lower dose (a daily capsule of 2,000 IU
of vitamin D3) for 12 weeks in asthmatic people age 65 and older in
Philadelphia. Prior to initiation of therapy, it found that mean vitamin D
levels in the blood were significantly lower (19.0 ng/mL) in those with
uncontrolled asthma compared to those with well-controlled symptoms (25.7
ng/mL). Self-reported symptoms of asthma decreased significantly after 12 weeks
of vitamin D treatment only in patients who had uncontrolled asthma, although
clinical measurements of airflow remained unchanged. The researchers note that
vitamin D receptors are present in the smooth muscle of the bronchi and vitamin
D has been shown to play a role in modulating the immune system (Columbo, Allergy, Asthma, &
Clin Immun 2014).
A study in Japan among schoolchildren with asthma found
that giving them each 800 IU of vitamin D daily for two months led to
significantly greater improvements in asthma control than did giving a placebo.
This improvement remained significant even four months after discontinuing
vitamin D, at which point 34% of those who had received placebo had difficulty
breathing compared to only 15% of those who had received vitamin D.
Interestingly, the children in both groups had had relatively high levels of
vitamin D (around 30 ng/mL) before the trial began and few were vitamin D
deficient (Tachimoto, Allergy 2016). In
contrast, a placebo-controlled study among 192 children with asthma in the U.S.
aged 6 to 16 years (most of whom had vitamin D levels above 20 ng/mL) found
that giving very high-dose vitamin D (4,000 IU daily) for 48 weeks did not
reduce the number of days until the next severe asthma exacerbation or lead to
reductions in their use of an inhaled steroid (fluticasone) (Forno, JAMA 2020). Furthermore, analysis
of additional data from the study showed that supplementing with vitamin D did
not reduce the immune response (based on antibody levels) to dust mites or
cockroaches — two common triggers of year-round asthma attacks (Rosser, J Allergy Clin Immunol 2021).
A review in 2016 of seven clinical trials (ranging in
length from 4 months to one year -- including the Castro and Tachimoto studies
noted above) investigating the effects of vitamin D supplementation in children
or adults with asthma (most of whom had mild to moderate asthma and used their
regular asthma medications as needed) found that oral vitamin D supplementation
(average daily dose 900 IU vitamin D3, although some participants received
additional, larger doses in some trials) reduced the average number of attacks
per year requiring treatment with oral steroid medication from 0.44 to 0.22,
and reduced the risk of hospitalization from asthma attacks from 6% to about
3%. However, measures of lung function (such as forced expiratory volume, or
FEV1) were not improved (Martineau, Cochrane Database Syst
Rev 2016). Due to lack of data, the researchers were not able to
assess whether the improvements would be limited to those who were deficient in
vitamin D before supplementation, or whether those with more severe asthma
would benefit. A later review of studies similarly
found that vitamin D supplementation reduces the rates of asthma exacerbations
requiring treatment with systemic corticosteroids. However, it
found that these protective effects were only seen among people with very low
vitamin D levels (less than 10 ng/mL) prior to vitamin D treatment and not in
people with higher levels (Jolliffee, Lancet Respir Med, 2017).
COPD (Chronic obstructive pulmonary disease)
Several studies have shown that high-dose vitamin D may reduce exacerbations
in adults with COPD and/or asthma who also have low blood levels of vitamin D,
but it does not appear to be beneficial in those who already have sufficient
levels.
A placebo-controlled study in the UK of 240 people with COPD found that taking
vitamin D3 (120,000 IU orally every 2 months — equal to 2,000 IU per day)
significantly reduced the risk of having moderate or severe exacerbations among
those who began the study deficient in vitamin D (blood levels below 20 ng/mL).
This benefit was not found for those who began the study with sufficient levels
of vitamin D. Vitamin D did not reduce the risk of upper respiratory infection
among any group. (Martineau, Lancet Resp Med 2014).
A study in Belgium found that vitamin D supplementation
(100,000 IU every 4 weeks) significantly reduced exacerbations of COPD but only
among patients starting with vitamin D levels less than 10 ng/mL (Lehouck, Ann Intern Med 2012). Similarly,
a study in New Zealand among 775 older men and women (average age 67)
with asthma and/or COPD found that, overall, vitamin D3
supplementation (initial oral dose of 200,000 IU followed by 100,000 IU monthly
for more than three years) did not reduce the risk of exacerbations (use of
oral corticosteroids more than 20 days) compared to placebo, except in those
who began the study with deficient blood levels of vitamin D (< 10 ng/mL) (Camargo, Nutrients 2021).
Allergies
Higher serum vitamin D levels are associated with a reduced risk of allergy
in children and adolescents, but not in adults. Preliminary evidence suggests
that giving vitamin D to pregnant women may reduce infants' risk of allergic
sensitivity and supplementing people with low levels of vitamin D may help
reduce some symptoms of allergy.
A review of data from a nationwide study of over 6,000 individuals showed that,
for children and adolescents, allergic sensitization was more common in those
with serum vitamin D of less than 15 ng/mL compared to those with 30 ng/mL or
greater for 11 out of 17 allergens. Results were adjusted for potentially
confounding factors like time spent on indoor activities. The strongest
associations were for allergy to oak (5 times the risk), peanut (2.4 times the
risk), and ragweed (1.8 times the risk). There was also increased risk of
allergy to dog, cockroach, mite, shrimp, ryegrass, Bermuda grass, birch and
thistle. In adults, there was no consistent association between allergy and
vitamin D levels.19
Giving vitamin D daily to infants (as well as to their mothers while
pregnant) reduces infants' risk of allergic sensitivity to dust mites and reduces
visits to the doctor for asthma during the infancy. This
was shown in a study in New Zealand in which pregnant women were given 1,000 IU
or 2,000 IU of vitamin D during the last 3 months of pregnancy and their
newborn infants were then given, respectively, 400 IU or 800 IU for 6 months.
Another group of mothers and infants received placebo. During the first 18
months of life, 11% of infants in the placebo group saw a doctor for asthma,
compared to 0% who received the lower dose of vitamin D and 4% who received the
higher dose. Virtually all of the infants were breastfed at birth, although 47%
began infant formula prior to age six months. The researchers noted that other
studies have shown that sensitization to dust mites is associated with
increased risk of childhood asthma (Grant, Allergy 2016).
A double-blind study among 68 men and women (average age
29) in Iran with seasonal allergies (allergic rhinitis) with generally low
average blood levels of vitamin D (14.4 ng/mL) found that those who took 50,000
IU of vitamin D3 once per week for two months in addition to the antihistamine medication
cetirizine (Zyrtec, Aller-Tec) had significant decreases in self-reported nasal
itching, sneezing, runny nose and post-nasal drip compared to those who took
cetirizine with a placebo. There was no improvement in eye redness and itching.
Among those who took vitamin D, average blood levels of vitamin D increased to
24 ng/mL while levels remained relatively unchanged (15 ng/mL) in those who did
not take vitamin D (Bakhshaee, Eur Arch
Otorhinolaryngol 2019).
Chronic Hives (Urticaria)
Chronic hives or urticaria is characterized by the recurring appearance of
hives and welts. A 12-week, placebo-controlled study among 120 people with
chronic urticaria in India who were deficient in vitamin D (average blood level
of 14 ng/mL) found that a 60,000 IU dose of vitamin D3 taken every two weeks
(averaging 4,286 IU per day) significantly reduced disease severity and levels
of inflammatory cytokines in the blood. Need for antihistamine medication also
decreased. Blood levels of vitamin D increased to an average 29.5 ng/mL among
those taking it. The researchers attribute the improvement to vitamin D's
action as an immunoregulatory hormone (Mony, Clinica Chimica Acta, 2020).
[Note, it is preferable to take lower doses of vitamin D daily or weekly than a
large dose less often, although this is used in some clinical trials, like this
one, to ensure compliance.]
Eczema
Some research shows that taking vitamin D reduces eczema (atopic
dermatitis) severity in people with moderate to severe disease and low
or borderline low levels of vitamin D when used along with standard treatment.
Achieving or maintaining
a vitamin D blood level of at least 20 ng/mL was associated with a significant
reduction in the severity of eczema (atopic dermatitis) in comparison to levels
below 20 ng/mL in a study of 58 children and adults in Mexico with moderate to
severe eczema who were also given standard treatment (topical steroid, soap
substitute, and emollient). Levels of 30 ng/mL or higher provided no further
benefit (Sanchez-Armendariz, Int J Dermatol 2018). A
study in Egypt among 86 children and adolescents with severe eczema found that
taking 1,600 IU of vitamin D3 daily for three months in addition to applying 1%
hydrocortisone cream twice daily moderately reduced eczema severity compared to
using hydrocortisone cream alone. The percentage of people who achieved at
least 75% improvement in eczema severity was significantly higher in the
vitamin D group than the placebo group (39% vs 7%). In those who took vitamin
D, average blood levels of vitamin D increased from 22.8 ng/mL to 36.11 ng/mL,
while levels in the placebo group did not significantly change from the
baseline value of about 25 ng/mL (Mansour, Pharmacol Res Perspect
2020).
Psoriasis
Vitamin D supplementation was found to improve psoriasis in a study among 45
patients with mild, chronic, plaque psoriasis in Thailand who
had not responded satisfactorily to other treatments and generally had low
vitamin D levels. A statistically significant improvement in symptoms relative
to placebo was seen at 3 months. Improvements with vitamin D continued through
6 months, but the difference from placebo at that point fell slightly short of
statistical significance. Patients were given 60,000 IU of vitamin D2 (as three
20,000 IU capsules) every 2 weeks (averaging 4,286 IU/day) for 6 months. At the
start of the study, just over one-fourth of patients had vitamin D levels below
20 ng/mL, with an average level of 24 ng/mL and, by the end of the study, none
of the vitamin D-treated patients were below 20 ng/mL, compared to 44% in the
placebo group (an increase, due to seasonality), although vitamin D only raised
levels, on average, by about 3 ng/mL — a surprisingly small increase
considering the large dose. The researchers noted that vitamin D deficiency
appears to be several times higher among those with psoriasis than in the
general Thai population (Disphanurat, Derm Res Prac 2019).
Fibromyalgia
Fibromyalgia is a common syndrome in which a person has long-term, body-wide
pain and tenderness in the joints, muscles, tendons, and other soft tissues.
Some, but not all, studies suggest improvements in symptoms of fibromyalgia
with vitamin D supplementation, and it would seem worthwhile to raise vitamin D
levels if not already at least 20 to 24 ng/mL.
One randomized controlled study found that increasing vitamin D blood levels
from a mean of 19 ng/mL to about 50 ng/mL was associated with a modest decrease
in fibromyalgia pain (a 20-point decrease on a 100-point scale). The study
involved 30 adults (mostly women) in Austria with fibromyalgia. Most of the
participants started the study with vitamin D levels below 24 ng/mL and were
given 2,400 IU of vitamin D3 daily, while those starting with levels between 24 ng/mL
and 32 ng/mL were given 1,200 IU daily. Treatment continued for 20 weeks or
until vitamin D levels reached 48 ng/mL (levels in several patients went as
high as 55 to 93 ng/mL). Twenty-four weeks after supplementation ended, pain
returned to the original level in the group (Wepner, Pain 2013).
A study in Mexico among 80 women (average age 51) with mild to moderate
fibromyalgia found that weekly supplementation with 50,000 IU of vitamin D3 for
12 weeks did not improve function or measures of fatigue, pain, anxiety or
depression compared to placebo. However, 95% of those who received vitamin D
were not deficient in vitamin D to start (levels were 20 ng/mL or higher, and
were raised to an average of 51.8 ng/mL) and those in the placebo group who had
levels below 20 ng/mL were also given vitamin D (for ethical reasons), bringing
their average level up to 20 ng/mL. Symptoms scores dropped almost equally in
both groups. It does not seem possible to draw a valid conclusion from this
study regarding the benefit of vitamin D in treating women with fibromyalgia (Lozano-Plato, Clin Rheumatol 2021).
Insomnia
Although insomnia can occur in people with vitamin D deficiency, the
evidence that vitamin D supplementation improves sleep in people with low blood
levels of vitamin D is mixed. In addition, supplementation with high doses of
vitamin D may decrease the quality of sleep.
Vitamin D supplementation was shown to decrease the amount of
time it took to fall asleep by an average of about 10 minutes, and increase the
duration of sleep by about a half-hour, in U.S. veterans with chronic pain
whose 25(OH)D blood levels increased from an average of 18 ng/mL to 26 ng/mL
with supplementation. However, this study did not include a placebo group, and
it's not known if the improvement in sleep was a direct result of
supplementation, or due to a decrease in pain that also occurred, limiting the
significance of the findings (Romano, Curr Pharm Des
2020).
A placebo-controlled study in Norway among 189
men and women (average age 51) with low 25(OH)D blood levels (average 14 ng/mL)
found that increasing blood levels to an average of 34 ng/mL with vitamin D3
supplementation did not increase sleep duration, or reduce
symptoms of daytime sleepiness or insomnia, compared to placebo, even among
those who reported having insomnia before supplementation. Vitamin D3 was given
for four months starting with a single, high oral dose of 100,000 IU followed
by a once weekly dose of 20,000 IU — equivalent to 2,857 IU per day (Larsen, Sleep Med 2021).
Some research suggests that high-dose vitamin D supplementation may interfere
with melatonin production, and some but not all studies suggest that having blood
levels over 32 ng/mL may worsen sleep quality (see Concerns and Cautions).
Restless legs syndrome
A three-month, placebo-controlled trial among 22 men and women with restless
legs syndrome found that increasing average vitamin D blood levels from 19
ng/mL to 36 ng/mL with high-dose vitamin D supplementation (50,000 IU once a
week) did not decrease the severity of the symptoms of RLS (Wali, Sleep Breath 2018).
Headache
Low blood levels (under 20 ng/mL) of vitamin D have been associated with a
higher risk of frequent headaches and a moderate increase in migraine episodes,
although it has not yet been determined whether supplementing with vitamin D
provides these benefits. A study among 2,601 middle-aged men in Finland found
those who had the lowest blood levels of vitamin D (under 12 ng/mL or below)
were twice as likely to report frequent headaches than
men with higher blood levels. About 15% of men with the lowest levels (less
than 12 ng/mL) had headaches at least weekly, while the percentage was only 8%
among men with levels of 12 to 16 ng/mL, 16 to 22 ng/mL, or above 22 ng/mL (Virtanen, Scientific
Reports 2016). The researchers noted that vitamin D deficiency
has also been associated with chronic tension-type headache, perhaps by causing
musculoskeletal pain. A study in Korea among 157 men and
women (average age 37) with migraine found that headaches
occurred 20% more frequently in those who were deficient in vitamin D (< 20
ng/mL) than those who were not deficient, regardless of gender, type of
migraine (chronic, episodic, with or without aura), and factors such as
depression, anxiety and sleep quality. However, vitamin D deficiency was not
associated with the severity of migraine episodes (Song, J Clin Neurol 2018).
Lupus
A preliminary study suggests that raising low vitamin D
levels with supplementation provides beneficial immunological effects in
patients with systemic lupus erythematosus (SLE). Giving 100,000 IU
of vitamin D3 (weekly for a month and then monthly) along with regular therapy
to SLE patients with generally low vitamin D levels (averaging 19 ng/mL) raised
vitamin D blood levels to 42 ng/mL after 6 months of therapy, during which
patients experienced no flare ups and experienced an increase in regulatory T
cells and decreases in memory B cells, effector T cells, and anti-DNA
antibodies (Terrier,
Arth Res & Ther 2012).
Crohn's disease
Some, but not all, research suggests that people with Crohn's disease tend to
have lower blood levels of vitamin D, and that lower levels of vitamin D may be
associated with disease severity (Weisshof, Curr Opin Clin
Nutr Metab Care 2015). A small study among people with mild to moderate
Crohn's disease and insufficient blood levels of vitamin D found that
increasing average blood levels of vitamin D from 16 ng/mL to 40 ng/mL over 24
weeks decreased average Crohn's disease activity index (CDAI) scores by 112
points (from 230 to 118 points on a scale of 0 to 600 points) but did not
increase bone density compared to baseline. Participants started at a dose of
1,000 IU of vitamin D3 per day for the first week, and this dose was increased
to 5,000 IU per day for most participants in order to reach a blood level of 40
ng/mL. Most participants did not have adequate calcium intake at the beginning
of the trial, but average total calcium intake from diet and supplements
increased from 879 mg to 1,153 mg over the course of the study (Yang, Clin Transl
Gastroenterol 2013).
Irritable bowel syndrome (IBS)
A study in the UK among 135 men and women (average age 29) with mild to
moderate IBS, most of whom also had low or deficient blood levels of vitamin D,
found that 3,000 IU (75 mcg) of vitamin D3 taken as a sublingual spray (by
BetterYou Ltd, which funded the study) daily for three months did not reduce
symptom severity or improve quality of life compared to placebo, despite
increasing average blood levels of vitamin D from 19 ng/mL to 37 ng/mL (Williams, Eur J Nutr
2021).
Menstrual pain and Premenstrual Syndrome (PMS)
A small study of women with primary dysmenorrhea (painful menstrual cramping)
and a mean vitamin D blood level of 27 ng/mL found that giving a single high
dose (300,000 IU) of vitamin D3 reduced pain by 41% during the next two
menstrual periods. None of the women who received vitamin D needed
anti-inflammatory medicine to manage menstrual pain during the two months,
whereas 40% of those taking placebo used it at least once.29 A concern, however, is that high dose vitamin D has been
shown to increase the risk of falls and fractures — at least in the elderly (as
noted above) and the dose given works out to 5,000 IU vitamin D per day, more
than the tolerable upper intake level of 4,000 IU per day (see Concerns and Cautions).
A study among extremely vitamin D deficient (< 10
ng/mL) adolescent and young women (ages 15 — 21) with self-reported severe or
extremely severe emotional and cognitive symptoms associated with premenstrual
syndrome found that high-dose supplementation (an initial dose of 200,000 IU
followed by 25,000 I.U. every two weeks ) with liquid vitamin D3 (Dibase®,
Abiogen Pharma, Italy) for four months significantly reduced these symptoms:
Mean scores of "irritability" decreased from 130 to 70, "crying
easily" decreased from 41 to 30, sadness decreased from "51 to
31" and "disturbed relationships" decreased from 150 to 70
compared to the beginning of treatment. Those who took a placebo had a
significant reduction only in "irritability" (from 128 to 119). (Tartagni, J Pediatr Adolesc Gynecol 2015). It should be noted
that the dosing may have been unnecessarily high as blood levels rose to 35 to
60 ng/mL.
Polycystic Ovary Syndrome (PCOS)
A randomized, placebo-controlled study in Jordan among 58 overweight women with
vitamin D deficiency and PCOS (average age 24) found that taking 50,000 IU of
vitamin D3 once
weekly for 12 weeks increased 25(OH)D levels from 12.5 ng/mL at baseline to
50.2 ng/mL. Compared to placebo, women supplemented with vitamin D showed
decreased levels of parathyroid hormone and testosterone, increased levels of
sex hormone binding globulin, and reduced severity of hirsutism (male-patten
hair growth in women). Ovarian volume, which is often increased in women with
PCOS, returned to normal for 24% of women given vitamin D compared to none of
the women given placebo. Also, a greater percentage of women given vitamin D
experienced regular menstrual cycles compared to placebo (93% vs 10%) (Al-Bayyari, Clin Nutr 2020). The researchers did
not determine if these improvements increased fertility.
Uterine fibroids
A study of women ages 35 to 49 found that those with vitamin D levels above 20
ng/mL were 32% less likely to have had uterine fibroids than those with lower
levels. Similarly, women who reported getting at least one hour per day of sun
exposure (weather permitting), were 40% less likely to have had fibroids than
women reporting less sun exposure (Baird, Epidemiology 2013). The risk of
fibroids appeared to continue to decrease as vitamin D levels approached 35
ng/mL. Possibly explaining these findings are laboratory studies showing that
vitamin D in its active form inhibits the overproduction of tissue by uterine
muscle cells -- the cause of fibroids. The study was conducted in Washington,
D.C. in the late 1990s and only 10% of Black women and 50% of white women had
vitamin D levels above 20 ng/mL. Fibroids are the leading reason for
hysterectomy in the U.S.
Early menopause
Adequate intake of vitamin D from the diet is associated with a lower risk of
early menopause (i.e., menopause before age 45). Early menopause is of concern
because it is associated with higher risk of cardiovascular disease,
osteoporosis, and other conditions. A study of more than 80,000 women found
that those who had the highest intakes of vitamin D from foods (528 IU per day
-- equivalent to that found in 2.5 cups of milk per day) had a 17% lower risk
of early menopause than women with the lowest intakes from food (148 IU per
day) after adjusting for age, smoking and other factors. The association
between intake of vitamin D from foods and reduced risk of early menopause was
strongest when vitamin D was obtained from dairy foods, as opposed to non-dairy
foods, although the reason for this is not clear. Intake of vitamin D from
supplements was not associated with a reduced risk — and high intake of calcium
from supplements (particularly 900 mg or more per day) was actually associated
with an increased risk of early menopause (Purdue-Smith, Am J Clin Nutr 2017).
Erectile dysfunction
Vitamin D plays a role in endothelial function and in the production of nitric
oxide, which are important for proper erectile function (Andrukhova, Mol Endocrinol 2014; Molinari Cell Physiol Biochem 2011). A study in Turkey
among 111 men with erectile dysfunction and low blood levels of vitamin D
(average 14 ng/mL, measured as 25(OH)D) found that those who took 4,000 IU (100
mcg) of vitamin D3 in addition to 5 mg of tadalafil (Cialis) once daily for
three months had greater improvements in erectile function (an increase of
about 13 points vs 5.5 points on a 30-point scale) and increased sexual desire
(an increase of about 2.4 points vs 1.5 points on a 10-point scale) compared to
those who took tadalafil alone. Both groups had similar improvements in
orgasmic function, and sexual and overall satisfaction. In those who took
vitamin D, average blood levels increased to 35 ng/mL, while there was no
significant change in vitamin D levels among those who did not take vitamin D (Demirci, Urol Int 2021).
Pregnancy
As described below, an adequate vitamin D level during pregnancy is
associated with better infant growth and decreased risk of pre-term labor,
pre-eclampsia, and gestational diabetes. Supplementing with vitamin D to
correct deficiency has also been shown to reduce health risks to the mother,
improve bone mineral density in children as they grow, and possibly reduce the
risk of tooth defects in children. However, high-dose vitamin D during
pregnancy does not seem to reduce the risk of pre-term birth, NICU admission,
or neonatal infection or improve motor or cognitive development in children,
although it might reduce the risk of pregnancy loss.
Vitamin D levels in the blood of pregnant women are associated with infant
growth. A study in the U.S. found that the birth weight and head
circumference of babies rose with increasing vitamin D levels up to 15 ng/mL (Gernand, J Clin Endocrin & Metab 2012). Mothers with levels of
15 ng/mL or greater gave birth to newborns 46 grams (0.1 lb) heavier and with
head circumferences 0.13 cm larger, on average, than those of mothers with
vitamin D levels less than 15 ng/mL. A level of 15 ng/mL or greater in the
first trimester was also associated with half the risk of an infant being small
for its gestational age.
Having sufficient blood levels of vitamin D during pregnancy is
also associated with a decreased risk of gestational diabetes (diabetes
developing in pregnant women). A study among 8,468 women in China found that,
among those who had 25(OH)D blood levels of 20 to 30 ng/mL (measured before 20
weeks gestation), 9.73% developed gestational diabetes compared to 12% among
those with blood levels below 20 ng/mL (Yue, Nutr Metab (Lond) 2020).
A study in India evaluated the effect of giving pregnant
women large doses of vitamin D. Those with already sufficient levels (above 20
ng/mL) were given a single dose of 60,000 IU D3 at week 20 of their pregnancy (averaging about 400 IU per
day over the duration of their pregnancy), and those with insufficient (10 to
20 ng/mL) or deficient (<10 ng/mL) levels were given a monthly dose of
120,000 IU twice or four times, respectively, raising the average blood level
of the entire group to 32 ng/mL. In another group of women who were not given
vitamin D (average vitamin D level of 18.4 ng/mL), 44% developed pre-term
labor, pre-eclampsia, and/or gestational diabetes, in contrast to 20.3% of
the women given vitamin D. The non-treated group also had babies with a lower
average birth weight (5.28 lbs) than did those given vitamin D (5.72 lbs) (Sablok, Clin Endocrinol 2015). The researchers note
that lower-dose daily preparations may have been preferable to the large
monthly doses but were not available.
A study in the U.S. among 392 pregnant women who, on
average, already had sufficient levels of vitamin D, found that supplementing
with 3,000 IU of vitamin D daily during pregnancy did not reduce
the risk of preterm birth, low birth weight, NICU admission, respiratory
distress, or infection in the infant compared to not supplementing.
However, pregnancy loss was significantly lower and
infants' Apgar scores (reflecting their general condition at
birth) were significantly higher among women who supplemented with vitamin D
compared to those who did not (Persad, Am J Obstet Gynecol 2021).
Giving expectant mothers high-dose vitamin D appears to
reduce the risk of tooth enamel defects in their children. At
age six, the children in Denmark of mothers who were given vitamin D3 (2,400 IU
plus another 400 IU per day) from the 24th week of pregnancy to one week
postpartum had a 50% lower risk of enamel defects in baby and permanent teeth
compared to children of mothers given 400 IU per day (Note: The recommended
daily allowance for pregnant women is 600 IU per day). Interestingly, the women
were generally not deficient in vitamin D prior to supplementation, having
average blood levels of about 30 ng/mL, which increased to 43 ng/mL at one week
postpartum in those who took the higher dose of vitamin D but decreased
slightly to 28 ng/mL in those who took the lower dose. However, there was no
association between high-dose vitamin D supplementation and the risk of
cavities (Norrisgaard, JAMA Pediatr 2019).
The same study found that children of the mothers given
high-dose vitamin D had greater whole body bone mineral density at
age 6 than those of mothers given only 400 IU. However, this only held true for
children of mothers who, prior to the study, had vitamin D levels below
30 ng/mL (an arbitrary breakpoint for analysis). There was no bone
benefit from giving high-dose vitamin D to women whose levels were already
sufficient. In fact, an accompanying editorial noted that giving vitamin D to
women with levels above 50 ng/mL is associated with decreased growth of
offspring (Holmlund-Suila, JAMA Ped 2020). The researchers noted
that starting vitamin D earlier in pregnancy may have additional benefit
because bone growth centers begin in the first trimester (Brustad, JAMA Ped 2020).
Further analysis of results from this same trial did not find
benefits from prenatal high-dose vitamin D in children by age 6 with regard to
motor, language, or cognitive development, nor reduced emotional or behavioral
problems in comparison to those of mothers given 400 IU daily. The average
blood level of vitamin D prior to high-dose supplementation was 30.6 ng/mL,
with only 14% of the women having levels less than 20 ng/mL. (Sass, JAMA Netw Open 2020).
Respiratory infection, colds, and influenza
Vitamin D may be effective in reducing respiratory infections in people who
do not already have adequate levels (20 ng/mL) of vitamin D (which is most
common in the winter and spring) and when vitamin D is given daily, not in
extremely large periodic doses.
In healthy adults with generally sufficient vitamin D levels
(averaging 29 ng/mL), monthly supplementation of high dose vitamin D3 (100,000
IU) resulted in no reduction in the number of upper respiratory
infections (colds), the severity or duration of such infections, nor the
number of days of missed work, compared to a similar group of people given
placebo (Murdoch, JAMA 2012). Among those receiving the supplement, vitamin D levels
averaged over 48 ng/mL throughout the study. The researchers commented that
vitamin D supplementation may have been helpful had the population been vitamin
D deficient, citing a study in which vitamin D supplementation was associated
with a 50% reduction in acute respiratory infections among
Mongolian schoolchildren who had an average vitamin D level below 10 ng/mL (Camargo, Pediatrics 2012).
Similarly, a five-year, placebo-controlled study among 15,373
people in Australia ages 60 to 84 found that monthly, high-dose (60,000 IU)
vitamin D3 did not reduce the risk of developing an acute respiratory
infection. However, blood levels of vitamin D measured during the study
averaged 46 ng/mL in the vitamin D group and 31 ng/mL in the placebo group,
indicating that people in both groups had more than adequate levels (Pham, Lancet Diabetes Endocrinol 2021).
A study in London found that periodic high doses of vitamin
D increased the risk and duration of respiratory infections. The
study was conducted among 194 older residents of group homes and 46 of their
caregivers (average age was 67 years). Sixty-four percent of subjects began the
study with blood levels below 20 ng/mL (92% were below 30 ng/mL). During the
study, all residents were given 400 IU of vitamin D3 daily and more than half
were given an additional 96,000 IU every two months -- for a total dose
averaging 2,000 IU per day. (A subgroup of caregivers was given what also
averaged to 2,000 IU per day, but as 120,000 IU every two months.) Over one year,
those who received the large doses of vitamin D were 48% more likely to develop
an upper respiratory infection than those who did not receive the large doses,
and these infections lasted longer (7 days vs. 5 days, respectively). The
researchers note that other studies have found that relatively low-dose vitamin
D has been shown to offer protection against upper respiratory infection and
that intermittent large doses have not. Interestingly, those receiving large
doses had an average level of 34 ng/mL at the end of the study (2 months after
the last large dose), while those who did not receive large doses (most of whom
received just 400 IU daily) and had fewer respiratory infections ended the
study with levels averaging 24 ng/mL (Martineau, Thorax 2015).
Similarly, a placebo-controlled study in people with mild
to moderate asthma found that giving high-dose vitamin D (100,000 IU initial
dose and 4,000 IU daily for 28-weeks) did not decrease the risk of developing a
cold. In fact, with this vitamin D supplementation (which raised the mean
vitamin D level to 42 ng/mL), the risk of a developing a cold was found to
be 40% higher among those who reached vitamin D blood levels
of 30 ng/mL or higher, and 70% higher among those who were
African-American (Denlinger, Am J Resp and Crit Care Med 2015. Also see Castro study,
above, for effects on asthma control in this same group.)
In contrast the above studies in adults, a study in Sweden
found vitamin D supplementation to be quite helpful. The double-blind study was
conducted in adults with frequent upper respiratory infections in whom vitamin
D levels tended to be low (half had levels below 20 ng/mL). Many also had
immunodeficiencies. Vitamin D3 (4,000 IU) or placebo was taken daily for one
year. Although benefits were not seen until after 3 months, over the full
course of the year vitamin D reduced the risk of infection by 36% and the total
number of respiratory tract infections by 28% relative to placebo (Bergman BMC Res Notes, 2015). An earlier analysis of
the same study additionally showed that vitamin D resulted in reductions of 50%
in positive bacterial cultures and 60% in antibiotic consumption (Bergman, BMJ Open 2012).
A study among older men and women (average age 81) in a long-term
care facility with average vitamin D blood levels of about 23 ng/mL who, each
month, received either high dose (100,000 IU) or a lower dose (which was either
12,000 IU monthly or 400 IU to 1,000 IU daily as part of standard care) found
that over the course of a year, those who received high dose vitamin D3 had a 40% lower incidence of acute respiratory infections
compared to those who received the low dose. However, the high dose patients
were also more than twice as likely to experience a fall (although not a
fracture) during the study period (Ginde, J Am Geriatr Soc 2016) — a finding in line
with other research showing that high dose vitamin D may weaken legs and increase
the risk of falls (See "Muscle, balance and falls" for more about this).
Respiratory infections tend to be seasonal events,
occurring more often in winter/spring than summer/fall. Some research has found
that antimicrobial activity in the airway varies with seasons, being less
active in winter/spring than summer/fall. This might contribute to
increased respiratory infections in the winter/spring. Low levels of vitamin D
have been associated with reduced antimicrobial activity in the airway. A study
of 40 people (average age 28) with low levels of 25-hydroxy vitamin D showed
that taking 1,000 IU of vitamin D3 daily for 90 days (during the winter and
spring) corrected for seasonal differences in antimicrobial activity of the
airway (Buonfiglio, Nutrients 2020). This suggests that
supplementation with vitamin D during the winter/spring months might reduce the
risk of respiratory infection.
Researchers in Japan studied the effect of vitamin D3 supplements (1,200 IU per day from December through March)
on the incidence of seasonal influenza A in school children.
Influenza A infection occurred in 18.6% of children in a placebo group versus
10.8% of children who received the supplement -- a 42% reduction in risk among
those taking the supplement. The reduction was more prominent among children
who had not been taking other vitamin D supplements. Influenza infection was
not reduced among a subgroup of asthmatic children but those who became
infected were significantly less likely to have an asthmatic attack if they had
received vitamin D than if they had not. Supplementation did not affect the
incidence of influenza B (which is less common than influenza A and is not
seasonal).14
An analysis of 25 studies of vitamin D for cold and flu
(including many of the studies noted above) concluded that vitamin D
supplementation protected against acute respiratory tract infection, but the
patients most likely to benefit were very deficient (blood levels of vitamin D
below 10 ng/mL) and receiving daily or weekly doses rather than less frequent,
large doses. Giving vitamin D reduced the risk of infection by 42% in people
with levels below 10 ng/mL, and by 70% if dosing was daily or weekly. For those
with levels above 10 ng/mL, the risk reduction with giving vitamin D was only
statistically significant when given daily or weekly, resulting in a 25% reduction
in risk of infection (Martineau, BMJ 2017).
Adequate vitamin D levels were associated with a lower
risk of pneumonia in a study of men and women ages 53 to 73 in
Finland which followed them for an average of nine years ( Aregbesola, J Epid Comm Hlth 2013). Compared to adults
with vitamin D levels above 20 ng/mL, the likelihood of being hospitalized with
pneumonia was 40% higher among those with levels below 20 ng/mL but above 13.5
ng/mL, and 140% higher among those with levels below 13.5 ng/mL, after
adjusting for other factors which might predict pneumonia. The researchers
found that a low vitamin D level was almost as strong a risk factor for
pneumonia as smoking.
COVID-19:
Most, but not all, studies have linked adequate levels of vitamin D in
people who develop COVID-19 with less severe disease, decreased need for
intensive care and ventilation, and a lower risk of death. Preliminary research
suggests that supplementing with moderate to high vitamin D when vitamin D
levels are low (about 20 ng/mL or lower) may improve prognosis in people
hospitalized with COVID-19, but extremely high single doses have not been shown
to help. There appears to be an increased risk of COVID-19 in people with very
high levels of vitamin D.
How vitamin D may work
As noted elsewhere, vitamin D is an immunomodulatory hormone that may help
reduce respiratory infections and is required in certain steps of the body's
immune response to fight the replication of viruses such as SARS-CoV-2 (Berry, Brit J Nutr 2011). Vitamin D has been theorized as helping to
prevent a damaging "cytokine storm" in the lungs of COVID-19
patients. Another theory, based on the analysis of lung tissue of COVID-19
patients, suggests that vitamin D might prevent a "bradykinin storm"
by preventing bradykinin levels in the lungs from getting too high and causing
the fluid leakage from the blood vessels in the lungs (Garvin, Elife 2020).
Reduced risk of coronavirus infection
Three studies linked low levels of vitamin D to a higher risk of SARS-CoV-2
infection.
A study among 392 healthcare workers (average age 41) in the
U.K. who had previously shown symptoms of COVID-19 found that the presence of
SARS-CoV-2 antibodies (confirming that infection had occurred) was more common
in those who were vitamin D deficient (25(OH)D <12 ng/mL) than those who
were not vitamin D deficient (72% vs. 51%), suggesting that vitamin D
deficiency may increase susceptibility to SARS-CoV-2. Men of Black, Asian, or
ethnic minority groups were particularly affected, with SARS-CoV-2 antibodies
detected in 94% of those who were vitamin D deficient compared to only 53% of
those who were not deficient (Faniyi, medRxiv 2020 - preprint).
A study in Chicago found that people who were likely to be
deficient in vitamin D (determined from previous vitamin D testing, such as
having a level below 20 ng/mL and/or a history of lack of supplementation)
were 77% more likely to test positive for coronavirus than
those expected to be vitamin D sufficient after controlling for demographic and
other variables. The researchers concluded that "vitamin D deficiency that
is not sufficiently treated is associated with COVID-19 risk." (Meltzer, JAMA Netw Open 2020). A subsequent
study by these researchers did not show a significantly lower likelihood of
testing positive at levels of 40 ng/mg or greater compared to levels of 30-39
or 20-29 ng/mL in the studied population; however, specifically among Black
individuals, the likelihood of testing positive was lower at levels at or above
40 ng/mL than at 30-39 ng/mL, although oddly, the likelihood of testing
positive at or above 40 ng/mL was not significantly different from that at
20-29 ng/mL (Meltzer, JAMA Netw Open 2021).
Similarly, a study in Israel found that people with vitamin D levels below 30
ng/mL were 45% more likely to test positive for SARS-CoV-2 as well as 95% more
likely to be hospitalized for it after adjusting for demographic and other
variables. The 30 ng/mL level was arbitrarily selected for the analyses and a
look at the study data shows greater clustering of positive test results at
levels below 20 ng/mL (Merzon, medRxiv 2020).
Be aware that high levels of vitamin D have been associated with increased risk
of COVID-19.
Reduced severity of disease, need for
intervention, and death
Low levels of vitamin D have also been associated with more severe respiratory
symptoms and higher risk of death from COVID-19 in some, but not all, studies.
A study in Germany among 185 people (average age 60) with COVID-19 found that
those with blood levels of vitamin D (total 25(OH)D) below 12 ng/mL when they
became ill were approximately six times as likely to require invasive
mechanical ventilation and 15 times as likely to die from
COVID-19 compared to those with blood levels above 12 ng/mL, even after
adjusting for age, gender, and underlying health conditions (Radujkovic, Nutrients 2020).
Additionally, a study among 20 hospitalized COVID-19 patients in New Orleans,
found that 84.6% of the COVID-19 patients in the ICU (intensive care unit) had
blood levels of vitamin D of less than 30 ng/mL vs. 57.1% of COVID-19 patients
who did not require intensive care, although the difference did not reach
statistical significance, possibly due to the small size of the study. All of
the COVID-19 ICU patients under 75 years of age had vitamin D blood levels
below 30 ng/mL, and among these, 64.6% had levels below 20 ng/mL and 27% had
levels below 10 ng/mL. The researchers noted that vitamin D insufficiency is
more prevalent in African Americans, the elderly, and those with conditions
such as high blood pressure and diabetes, all of whom are at higher risk for more
severe outcomes from COVID-19 (Lau, medRxiv 2020 -- preprint).
A study among 144 people (median age 66) in Boston and New York hospitalized
with COVID-19 found that those with 25(OH)D levels at least 30 ng/mL had
significantly lower rates of death compared to those with levels less than 30
ng/mL (9.2% vs. 25.3%, respectively). It is important to note that 30 ng/mL was
arbitrarily selected as the threshold value for the primary analyses but
"similar findings were obtained ... with a threshold of 20 [ng/mL]".
That is, levels of at least 30 ng/mL were not necessarily better than levels of
at least 20 ng/mL (Angelidi, Mayo Clin Proc 2021).
A review of the records of 42 people (average age 65)
hospitalized in southern Italy for acute respiratory failure due to COVID-19
showed an association between severe vitamin D deficiency (blood levels of
25(OH)D <10 ng/mL) and a higher risk of mortality. Patients with severe
vitamin D deficiency had a 50% probability of dying by day 10 compared to a 5%
probability of dying among those with 25(OH)D levels at least 10 ng/mL,
suggesting that severe vitamin D deficiency may worsen prognosis of patients
with COVID-19 (Carpagnano, J Endocrinol Invest 2020).
A study among 235 adults (average age 59) treated for
COVID-19 in a hospital in Iran found that those with 25(OH)D levels of less
than 30 ng/mL were 59% more likely to have a severe or critical case compared
to those with levels of 30 ng/mL or more (Maghbooli, PLoS One 2020). [Note: This study is currently under review
due to the publisher's concerns as to whether the statistical analyses used can
support the authors' conclusions, the number of patients whose diagnosis was
not laboratory confirmed, and other issues.] Blood levels of vitamin D
were also found to be an independent predictor of mortality in a study of
hospitalized COVID-19 patients in Turkey, where average 25(OH)D levels among
those who died was only 10 ng/mL compared to 19 ng/mL in those who survived (Karahan, J Nutr Health Aging 2020).
Interestingly, a study in Italy that focused on COVID-19
patients taking doses of vitamin D equivalent to 800 IU or higher per day (mean
intake 1,800 IU daily) during the prior 3 months (and excluding those taking
lower doses) showed no lower risk of hospitalization or in-hospital mortality
compared with those who did not take vitamin D supplements,
despite almost three-fold higher blood levels of vitamin D (32.9 ng/mL vs 11.3
ng/mL, respectively) (Cereda, Nutrition 2020).
Treatment of COVID-19 patients
As described below, there have been several preliminary reports suggesting
benefits from giving patients hospitalized with COVID-19 vitamin D or a form of
vitamin D (calcifediol), although it remains uncertain what dose is most
effective, and any benefit seems to be limited to only those who are vitamin D
deficient.
A review of medical records of elderly residents of a nursing
home in France showed that survival at one month after COVID-19 diagnosis was
86% greater for those who had been given a high-dose (80,000 IU) vitamin D in
the previous month or in the week following diagnosis compared to those who did
not receive supplementation (Annweiler, J Steroid Biochem Mol Biol 2020). It should be stressed
that these patients were given vitamin D due to high frequency of vitamin D deficiency
(not as COVID-19 treatment) and that more frequent (daily or weekly) use of
lower dose vitamin D to treat deficiency is preferable whenever possible
(see How Much Is Too Much).
A preliminary analysis of patients admitted to a hospital system in
northeastern England (where vitamin D deficiency is common) found a 35% higher
prevalence of vitamin D deficiency in COVID-19 patients requiring intensive
care compared to those managed in medical wards. Deficiency was promptly
treated, which may partially explain why fatality rates did not differ by
initial vitamin D level (Panagiotou, letter in Clin Endocrinol (Oxf) 2020).
A study in Spain among 76 people hospitalized with
COVID-19 infection (all of whom were given hydroxychloroquine and azithromycin)
found that those also given 532 mcg of calcifediol (a 25-hydroxylated form of
vitamin D) on the day of admission followed by 266 mcg of calcifediol on day 3
and day 7 of hospitalization had a lower risk of being admitted to the ICU for
complications compared to those not given calcifediol (2% with calcifediol vs
50% without), as well as a lower risk of death compared to those not given
calcifediol (0 deaths with calcifediol vs 2 deaths without) (Castillo, J Steroid Biochem Mol Biol 2020). Bear in mind that the
people included in this study were probably vitamin D deficient, as average
levels of 25(OH)D in Córdoba, Spain, where the study was conducted, is about 16
ng/mL. It remains unknown if calcifediol would be beneficial in people with
adequate levels of vitamin D. Furthermore, the dose of calcifediol used in this
study was very high. Prescribed doses of calcifediol (for its approved
indications) are typically much lower (about 30 to 60 mcg per day) than those
used in this study. Excessive intake of vitamin D in any form, including as
calcifediol, can increase the risk of hypercalcemia (see Concerns and Cautions). Finally, calcifediol is a prescription
medicine in the U.S. and is not available in supplements.
A study in India among people diagnosed with mild or
asymptomatic COVID-19 found that 62% achieved SARS-CoV-2 negativity after 14
days of high-dose vitamin D treatment compared to just 20.8% in a control
group. Vitamin D was given as 60,000 IU daily for 7 days, followed 60,000 IU
either daily or once weekly for another week (depending on blood levels of
vitamin D after the first week). Blood levels of vitamin D were increased from
8.6 ng/mL to 51.7 ng/mL after 14 days for those in the vitamin D group (Rastogi, Postgrad Med J 2020).
A study in Singapore among 43 men and women age 50 or older
hospitalized with COVID-19 found that those who were started on a daily oral
dose of vitamin D3 (1,000 IU), magnesium (150 mg) and vitamin B12 (500 mcg)
within the first day of hospitalization and continued for up to 14 days were
about 71% less likely to require oxygen therapy and further intensive care
compared to those not receiving the supplements. However, blood levels of
vitamin D, magnesium and B12 were not measured, so it's not known if any of the
patients were deficient before supplementation (Tan, Nutrition 2020).
In contrast, a study in Brazil among 232 people (average age
56) with severe COVID-19 found that a single oral dose of 200,000 IU of vitamin
D3 did not shorten length of hospital stay or reduce
mortality, admission to ICU, or need for mechanical ventilation compared to
placebo, despite increasing blood levels of vitamin D to 30 ng/mL or more in
87% of the supplemented patients. Although not all patients included in this
study were vitamin D deficient at baseline, a subgroup analysis found no
benefit even among patients who were vitamin D deficient. However, vitamin D3
was not given until about 10 days after symptom onset, which may have been too
late to provide any significant benefit (Murai, medRxiv preprint 2020 and Murai, JAMA 2021).
Ear infection (Otitis media)
Among children ages 1 to 5 years with a history of recurrent ear infections,
those with higher blood levels of vitamin D had a decreased risk of
developing uncomplicated ear infections (acute otitis media) during
a 6-month study including wintertime. However, the study found that higher
vitamin D levels did not reduce the risk of complicated ear
infections (e.g., ear drum rupture). In fact, rates of complicated infections
were actually higher at vitamin D levels above 30 and 40 ng/mL than at lower
levels, leading the researchers to speculate that these higher vitamin D levels
potentially foster certain bacterial infection in the ear. The study also found
that giving 1,000 IU daily for 4 months raised vitamin levels from about 26
ng/mL to 37 ng/mL, while levels fell to about 19 ng/mL in children receiving
placebo (due to reduced sun exposure in winter). Although the children
receiving vitamin D experienced significantly fewer episodes of uncomplicated
ear infections, there was no significant reduction in complicated infections (Marchisio, Pediatr Infect Dis J 2013). It would seem best for
children to follow the recommendations for vitamin D outlined in the Summary above.
Hearing loss
An analysis of health data of 1,123 older people (average age 76) found that
hearing loss of speech-frequency and low-frequency (low-pitch) sounds was about
twice as great for those with low levels of vitamin D (total 25(OH)D < 20
ng/mL) compared to those with levels of 30 ng/mL or more, although there was no
increased risk for those with levels between 20 ng/mL and 29 ng/mL. There was
no association between vitamin D levels and the odds of high-frequency hearing
loss, which is the most common form of hearing loss (Szeto, Am J Clin Nutr 2020). Note that this analysis only showed
association and does not establish cause-and-effect relationships.
Depression & Mood
Lower levels of vitamin D have been associated with a higher risk and
severity of depression in some but not all studies; however, there is little evidence
that taking vitamin D reduces the risk of depression or improves mood. An
possible exception is in people with type 2 diabetes.
A study in Italy showed that older women with low vitamin D levels (below 20
ng/mL) were twice as likely to develop depressive mood as those with higher
levels. Older men with low levels were 60% more likely to develop depressive
mood (Milaneschi, J Clin Endocrinol Metab 2010). Data from the same
study showed that those who were severely vitamin D deficient (below 10 ng/mL)
were approximately 60% more likely than those with vitamin D levels above 30
ng/mL to experience substantial cognitive decline, although there was no such
association with attention level (Llewellyn, Arch Intern Med 2010).
A 3-year study found the risk of depression was 21%
lower among women (aged 50 to 79) who reported total daily vitamin D intake
(from foods and supplements) of at least 800 IU compared to women with intake
of less than 100 IU. Excluding women with evidence of depression at the
beginning of the study, a 20% lower risk of depression was seen with intake of
just 400 IU or more per day from foods, but there was no reduced
risk from supplements alone (Bertone-Johnson, Am J Clin Nutr 2011).
However, not all research has found an association
between vitamin D levels and risk of depression. A 5-year study among Puerto
Rican adults living in the Boston area (average age 57) found that those with
vitamin D deficiency (25(OH)D less than 12 ng/mL) were no more likely to report
symptoms of depression than those with adequate vitamin D levels (20 ng/mL or
more). The researchers noted that the inconsistent findings across studies
regarding the association between vitamin D levels and depression may be due to
differences in study designs, study populations, cutoffs used for evaluating
vitamin D status, and assessment of depression (Sahasrabudhe, J Nutr 2020).
On the other hand, a 6-month pilot study in the U.S. suggested that high-dose
vitamin D (50,000 IU of vitamin D2 per week) significantly improved mood in
women with type 2 diabetes who had serious depressive symptoms. Mean serum
blood levels of vitamin D increased from 18.8 ng/mL to 37.5 ng/mL during the
intervention. The study also showed a modest improvement in systolic blood
pressure and a slight decrease in weight. Although promising, the study
had no control group (Penckofer, Abstract from ADA Scientific Sessions 2013).
A study among 64 men and women in Iran with type 2 diabetes
and mild to moderate depression who had generally low blood levels of vitamin D
also found that 4,000 IU of vitamin D3 taken daily for three months decreased
symptoms of depression by an average of 27.6%, which was significantly greater
than among those given a placebo who experienced an average 10.8% decrease in
symptoms. Average blood levels of vitamin D increased in the treated group from
15 ng/mL to 32 ng/mL. Those who took vitamin D also showed modest improvements
relative to the placebo group in HbA1c (- 0.5% vs - 0.07%) and blood insulin
levels (- 0.7 vs 0.1 mU/L), although there were no significant changes in
fasting blood sugar or cholesterol levels (Omidian, Diabetes Metab Syndr 2019).
Meanwhile, a placebo-controlled study in which 50,000 IU of vitamin D3 was
given monthly over autumn and winter to pre-menopausal women who were not
depressed, nor, in general, deficient in vitamin D (starting levels averaged 25
ng/mL), showed no impact on mood, anxiety, or depressive
symptoms (Choukri, J Nutri Sci 2018). Furthermore, a placebo-controlled study in Denmark among 62
men and women diagnosed with mild, moderate or severe depression found that
daily supplementation with 70 mcg of D3 (2,800 IU) for six months did not
improve depression scores - even among those who were deficient in vitamin D
(< 10 ng/mL) before supplementation. Average blood levels of vitamin D rose
from 17 ng/mL to 39 ng/mL during the study (Hansen, BMC Res Notes 2019).
A year-long, placebo-controlled study among 151 older men and women (average
age 67) in the Netherlands with moderate depression and somewhat low average
blood levels of vitamin D (18 ng/mL) also failed to find a benefit. Among those
who took vitamin D (1,200 IU per day) and maintained a calcium intake from
foods and/or supplements of approximately 1,000 mg per day, vitamin D blood
levels increased to 34 ng/mL, but there were no significant improvements in
symptoms of depression or anxiety, and no improvements in physical and
cognitive function compared to those who took a placebo and whose average blood
levels of vitamin D remained relatively low (average 17 ng/mL) (de Koning, Am J Clin Nutr 2019).
A 5-year study involving more than 18,000 adults in Massachusetts aged 50 and
older with no history of depression found that 2,000 IU daily of vitamin D3 did
not result in statistically significant differences in the rate of occurrence
of depression. However, the individuals enrolled in the study were generally
not vitamin D deficient, with a mean 25-hydoxyvitamin D level of 30.8 ng/mL and
nearly 90% having levels at or above 20 ng/mL. About half of each group was
also supplemented with 1 gram daily of highly-concentrated fish oil, which also
had no effect on the occurrence of depression (Okereke, JAMA 2020).
Alzheimer's disease, dementia, memory and cognitive decline
Studies indicate that maintaining a vitamin D level of at least 20 ng/mL may
be helpful in reducing the risk of developing Alzheimer's disease.
Supplementing with vitamin D also seems to modestly improve cognition in older
individuals with mild cognitive impairment who are vitamin D deficient, but it
does not appear to boost cognitive performance in adults who are not
cognitively impaired.
A study that followed 1,658 older adults in the U.S.
for a mean period of 5.6 years found that the risk of developing dementia was
increased for people with starting blood levels of vitamin D below 20 ng/mL.
All participants were relatively healthy at the start of the study. People who
began the study with a level of 10 ng/mL up to 20 ng/mL were 53% and 69% more likely
to develop dementia and Alzheimer's disease, respectively, than
those with starting levels of 20 ng/mL and above; and people with levels below
10 ng/mL were 125% and 122% more likely to develop dementia and Alzheimer's
disease, respectively, than those starting with levels of 20 ng/mL or above.
While the study suggests that higher levels of vitamin D may be beneficial, it
did not test whether raising a person's vitamin D level reduces the risk of
dementia. However, as the researchers note, it clarifies that having a level
above approximately 20 ng/mL is unlikely to further reduce the risk of
developing dementia (Littlejohns, Neurology 2014).
Similarly, a study among 916 healthy older men and women in
France (average age 73) who were followed for an average of 11.4 years found
that those starting with vitamin D levels below 20 ng/mL had nearly
triple the risk of developing Alzheimer's disease during the study
than those starting with levels at or above 20 ng/mL. In addition, those who
began the study with vitamin D blood levels below 10 ng/mL also had
significantly faster rates of cognitive decline, and were more likely to have
high cholesterol and triglycerides than those with levels at or above 10 ng/mL
(Feart, Alzheimer's & Dementia 2017). Another
study that followed older, ethnically diverse adults in California for a mean
period of 4.8 years found that rates of decline in two areas of cognitive
functioning — episodic memory (word list learning) and executive functioning —
were greater among those starting with vitamin D levels below 20 ng/mL than
those starting with levels of 20 ng/mL and above. Decline in these two areas
are strongly associated with Alzheimer's dementia. Vitamin D status was not
associated with rates of decline in two other cognitive areas: semantic memory
(object naming and picture association) and visuospatial ability. The average
starting level of vitamin D among the participants was 19.2 ng/mL (Miller, JAMA Neurol 2015)
A study in France among women 75 years of age and older
found those with higher intakes of vitamin D from their diets were least likely
to develop Alzheimer's disease over a seven-year study period. Women consuming
more than 3,108 IU of vitamin D per week (444 IU per day) were 77% less likely
to develop Alzheimer's disease than those with lower vitamin D intake. There
was, however, no association between vitamin D intake and the risk of
developing other types of dementia. The study excluded women who had taken
vitamin D supplements (Annweiler, J Gerontol A Biol Sci Med 2012).
A 12-month, placebo-controlled clinical trial in China among 181
older individuals with mild cognitive impairment (MCI) found
that vitamin D supplementation (400 IU daily, taken with or after a meal)
resulted in modest but statistically significantly improvements in cognitive
functioning shown in verbal and performance tasks. The vitamin D and placebo
groups each started with average vitamin D levels of about 19 ng/mL, which
increased to 23.4 ng/mL in the vitamin D group. Total cholesterol levels also
decreased modestly in the vitamin D group relative to the placebo group, driven
by decreases in triglycerides and, unexpectedly, HDL ("good") cholesterol
(Note: Vitamin D has had mixed effects on cholesterol levels, and high doses
may even increase total cholesterol) (Hu, J Neurol Neurosurg Psychiatry 2018).
Another study in China among 183 older people (average age 67)
with MCI found that taking 800 IU of vitamin D daily for 12 months modestly
improved overall cognitive function based on the full-scale intelligence
quotient (FSIQ) score. People given vitamin D showed a 1.81% increase in FSIQ
score, while those given placebo showed a 3.28% decrease in
FSIQ score. People in the vitamin D group also showed improvements in some
verbal measures (such as vocabulary and short-term verbal memory) and non-verbal
measures (such as visuoconstructional ability and ability to interpret social
situations) based on the Wechsler Adult Intelligence Scale-Revised score
compared to those given placebo. Blood levels of vitamin D3 increased from 19.07 ng/mL to 23.38 ng/mL for people in
the vitamin D group. Interestingly, vitamin D also increased telomere
length (measured in the DNA of white blood cells), which may be of potential
benefit, as decreased telomere length may be a factor in predicting progression
of cognitive decline (Yang, J Alzheimer's Dis 2020).
However, high-dose vitamin D supplementation for four months
did not improve cognitive functioning in healthy
middle-aged and older adults in Norway with low blood levels of
vitamin D (average level of 13.6 ng/mL). Participants in the placebo-controlled
study were given a starting dose of 100,000 IU of vitamin D followed by 20,000
IU taken weekly, boosting average levels to 35.6 ng/mL (Jorde, J Neurologic Sci 2018).
Parkinson's disease
A study from Finland suggested that higher vitamin D status provides protection
against Parkinson's disease. People with the highest vitamin D levels (above 20
ng/mL) had a 65% lower risk of developing Parkinson disease than those with the
lowest vitamin D levels (below 10 ng/mL).
Multiple sclerosis
Although research suggests that vitamin D deficiency is a risk factor for
developing multiple sclerosis, it is not clear that supplementing with vitamin
D reduces the risk. An FDA review concluded that, in healthy people, there is
"no credible evidence of a relationship between intake of vitamin D and a
reduced risk of MS" (FDA Constituent Update 2018). There is mixed
evidence as to whether vitamin D levels of pregnant mothers correlate with MS
risk in their children, but one study (in Finland) found that the risk of MS as
an adult was 90 percent higher in children of mothers who were significantly
deficient in vitamin D (levels less than 12.02 ng/mL) compared with the
children of mothers with levels between 12.02 ng/mL and 20.03 ng/mL (Munger, JAMA Neurol 2016).
Autism Spectrum Disorder
Low blood levels of vitamin D have been associated with increased risk of
autism spectrum disorder. Preliminary clinical research suggests that vitamin D
given to children with autism spectrum disorder and vitamin D deficiency may
improve symptoms. There is no evidence that vitamin D improves symptoms of
autism in children who already have adequate levels of vitamin D.
A study in the Netherlands found that children whose mothers had very low
vitamin D blood levels (< 10 ng/mL) during pregnancy (measured during the
fifth month of gestation) were 3.8 times as likely to have
autistic traits by age six than those whose mothers had sufficient vitamin D levels
(20 ng/mL). Even with levels between 10 and 19 ng/mL, there was a 75% higher
risk, although this was not deemed statistically significant (Vinkhuyze, Mol Psychiatry 2016). The researchers noted
that vitamin D is involved in the production of the neurotransmitter serotonin,
which may play a role in certain autistic characteristics.
Similarly, a study in China found that infants with very low
levels of vitamin D at birth were more likely to have autism spectrum disorder
on follow up at age 3 than those with moderate levels. The average level in
autistic children was just 7 ng/mL compared to 16 ng/mL in non-autistic
children. It was predicted that the lowest risk of autism was among babies with
a blood level of 19.2 ng/mL, as risk was seen to increase above this level (Wu, J Bone Mineral Res 2017).
In 2016, researchers in Egypt reported an association between
lower blood levels of vitamin D and higher severity of autism symptoms. They
also reported that treating children with autism spectrum disorder (ages 3 to
10) with high-dose vitamin D (about 5,000 IU daily, as drops) for four months
resulted in a reduction in symptoms, while there was no change among children
given placebo drops (Saad, J Child Psychol Psychiatry 2016). However,
irregularities later discovered in how the data was collected and analyzed led
the editors of the journal in which the report was published to retract it in
2019, stating they "... no longer have confidence in the findings reported
in the original paper." (Editors, J Child Psychol Psychiatry 2019).
A placebo-controlled trial in Iran among 43 children with
autism spectrum disorder (ages 3 to 13, average age 9), most of whom were
vitamin D deficient at the beginning of the study, found that giving 300 IU/kg
of vitamin D daily (up to a maximum dose of 6,000 IU/day) for 15 weeks
increased the average blood level of vitamin D from just 8.19 ng/mL to 39.10
ng/mL and modestly reduced autism severity based on the childhood autism rating
scale (CARS) and autism treatment evaluation checklist (ATEC), which focus on
various symptoms and skills. However, supplementing with vitamin D did not
improve aberrant behaviors such as irritability, hyperactivity, social
withdrawal, and inappropriate speech. Note that the dose given was extremely
high, particularly for children. Lower doses would be safer and still able to
treat deficiency (Javadfar, Nutrition 2020).
Executive functioning and cognitive performance
Executive functioning refers to the set of mental skills that
help you get things done, like planning and strategic thinking. Maintaining a
sufficient level of vitamin D appears to be associated with better executive
functioning, according to a study in Norwegian adolescents. The study found
that adolescents with low vitamin D blood levels (below 20 ng/mL) scored worse
on tests of executive functioning and were more likely to report attention
issues than those with higher levels. It also found that giving 1,520 IU (or 38
mcg) of vitamin D3 daily
for three months (which increased average vitamin D blood levels from 17.6
ng/mL to 24.8 ng/mL) improved performance on the most demanding executive
functioning tasks -- although not on easier tasks (Grung, Scan J Psychol 2017). A preliminary study among Norwegian men
also suggests a positive association between vitamin D blood levels of 20 ng/mL
and above and better executive functioning (Hansen, Percept Motor Skills 2011).
A one-year study among 42 postmenopausal women in New Jersey who were
overweight or obese found that a daily dose of 2,000 IU of vitamin D resulted
in better performance in visual and working memory and learning than 600 IU or
4,000 IU. The 4,000 IU dose seemed to negatively impact reaction time, as that
group had a slower reaction time than the 600 IU group. The average starting
vitamin D blood level was 22.6 ng/mL, increasing to 30.2, 36, and 40.8 ng/mL,
respectively, in the 600, 2,000, and 4,000 IU groups (Castle, J Gerontol Series A 2019). Note: Obese people
tend to require larger doses of vitamin D to raise blood levels than people who are not
overweight.
Weight control
Vitamin D does not appear to play a role in weight control. Raising blood
levels of vitamin D from an average of 13 ng/mL to 24 ng/mL increased lean body
mass (muscle) by about 1 lb. (as noted earlier) but did not decrease BMI or body fat in
healthy in active men and women in Japan who supplemented with 420 IU of
vitamin D for one year (Sun, Ann Nutr Metab 2019).
Similarly, a 12-month study found that taking vitamin D3 had no overall effect on weight or fat loss in overweight
or obese postmenopausal women consuming a reduced calorie diet and following a
program of 45 minutes of aerobic 5 days per week (Mason, Am J Clin Nutr 2014). Regardless of whether they took 2,000 IU
vitamin D3 daily
or a placebo, women lost an average 16 lbs. (Note: The 2,000 IU dose of vitamin
D is fairly high for regular daily use, particularly in this study in which
average vitamin D blood levels were above 20 ng/mL to start. Seven percent of
the women taking vitamin D achieved levels above 50 ng/mL, which is potentially
harmful. In fact, a subsequent analysis of this study found that those who
received vitamin D lost strength in their leg muscles -- see
"Muscle, balance, and falls" above.) Interestingly, among the vitamin
D-treated women, those who achieved blood levels greater than 32 ng/mL lost
more weight than those whose levels remained below 32 ng/mL (19 lbs vs. 12 lbs)
and had greater reductions in their waistlines (3.5 inches vs. 2.2 inches) and
body fat. However, it may just be that vitamin D levels in the blood
rose more in women who lost more fat, due to the fact that vitamin D is fat
soluble and stored within fat; indeed, an earlier study by the same researchers
showed that weight loss raises vitamin D levels (Mason, Am J Clin Nutr 2011).
Frailty
A study found that older women (69 years and older) whose vitamin D levels were
not between 20 and 29.9 ng/mL had a greater risk of being frail.18 Frail individuals were those experiencing at least three
of the following criteria: weight loss, weakness, exhaustion, slowness, and low
physical activity. The risk of frailty was increased by 47% among those with
vitamin D levels below 15 ng/mL, 24% among those with levels below 20 ng/mL,
and 32% among those with levels above 29.9 ng/mL. An average of 4.5 years after
these measurements were made, those originally not frail but whose blood levels
had been below 20 ng/mL were 21% more likely to have become frail or died.
These findings correspond with the 2010 report from the Institute of Medicine
(IOM) indicating that 20 ng/mL is a sufficient level for vitamin D and that
levels above 30 ng/mL may be associated with certain risks.17
Cancer
All types
Studies generally show that having vitamin D serum levels above 20 ng/mL are
associated with lower risk of various cancers and levels of up to 39 ng/mL may
reduce the risk of death from cancer. Limited evidence suggests that vitamin D
supplementation may reduce pain and possibly fatigue in patients with advanced
cancer and low levels of vitamin D.
A major study (the VITAL study) of a cross-section of
middle-aged Americans given 2,000 IU of vitamin D daily for median of 5.3 years
found no overall reduction in invasive cancers and death from cancer relative
to placebo, although few participants were vitamin D deficient: The average
starting blood level was 30.8 ng/mL and increased to over 40 ng/mL with vitamin
D supplementation. However, when excluding the first two years of
the study, the rate of death from cancer was found to be 25%
lower with vitamin D than with placebo. As noted in the study, the results are
consistent with other studies: While supplementing with vitamin D may not
reduce the overall incidence of cancer, it may decrease tumor invasiveness and
the propensity to metastasize (Manson, NEJM 2018).
A secondary analysis of results from the VITAL study found
that vitamin D modestly reduced the risk of advanced cancer (i.e.,
cancer that was metastatic or fatal) compared to placebo. Advanced cancer occurred
in 2.1% of people in the placebo groups compared to 1.7% of people in the
vitamin D group (17% reduction). When results were analyzed based on BMI of the
people in the study, the incidence of advanced cancer was reduced by 38% for
those with a normal BMI (BMI <25) but not for those who were overweight (BMI
25 to <30) or obese (BMI 30 or more) (Chandler, JAMA Netw Open 2020).
Other studies have not demonstrated a reduction in cancers from taking vitamin
D supplements. For example, a large 4-year placebo-controlled study of
post-menopausal women in rural Nebraska found that giving 2,000 IU daily of
vitamin D3 and 1,500 mg of calcium (as 3 doses of 500 mg) did not significantly
lower the risk of cancer. However, a weakness of this study is that the women
were generally not deficient in vitamin D to start — their blood serum levels
averaged 32 ng/mL (rising to 44 ng/mL in the treatment group). In fact, most of
the women (including those in the placebo group) were already taking vitamin D
supplements before the study and were allowed to continue during the study,
with average daily intake of around 800 IU (Lappe, JAMA 2017). Similarly, a study of more than 5,000 older adults in
New Zealand found that giving high-dose vitamin D (200,000 IU followed by
monthly doses of 100,000 IU) for 2.5 to 4.2 years had no impact on cancer
incidence compared to placebo treatment. However, most people did not start the
study deficient in vitamin D (average blood level was 26.5 ng/mL). Vitamin D
treatment raised levels by more than 20 ng/mL (Scragg, JAMA Oncology 2018).
An unusual report published in 2016 suggests that, for
white women aged 55 years and older, vitamin D levels at or above 40 ng/mL, as
compared to levels below 20 ng/mL, are associated with greater than a 65%
reduction in risk of all invasive cancers combined, excluding skin cancer. This
study, however, has several weaknesses including the fact that it was based on
pooled data from two unrelated studies, one of which, run by the group GrassrootsHealth (which derives revenue from vitamin D home tests), was
based entirely on a self-selected group of women who chose to maintain
relatively high levels of vitamin D and self-reported their health status via a
questionnaire. While the data indicated much lower rates of cancers
(predominantly breast cancer) at increasing mean levels of vitamin D, the
greatest decrease was seen as mean levels increased from below 20 ng/mL into
the high 30s with no significant benefit indicated above that level. In
addition, potential adverse effects were not assessed (McDonnell, PLOS ONE 2016).
A small but well-controlled study among 150 palliative
care cancer patients with low levels of vitamin D (25(OH)D of 20 ng/mL or less)
showed that those given 4,000 IU of vitamin D3 oil drops daily for 12 weeks
increased their dose of fentanyl (an opioid pain medicine) at a slower rate
compared to those receiving placebo (about 0.56 mcg less fentanyl/hour
per week), suggesting modestly reduced pain. Patients receiving vitamin D also
reported less fatigue as measured by the Edmonton Symptom Assessment System
(ESAS) scale, although not on a different scale. There was no between-group
difference in antibiotic use or quality of life. Average 25(OH)D increased from
about 14 ng/mL to 32 ng/mL among those in the vitamin D group (Frankling, Cancers 2021).
A moderately decreased risk of developing colorectal
cancers, specifically, has been demonstrated with higher vitamin D levels
as well as with higher vitamin D intakes (Ma, J Clin Oncol 2011). An analysis of data from two large studies
of health professionals found higher vitamin D levels to be associated with a
much lower risk of developing a subtype of colorectal cancer in which there is
extensive immune cell infiltration within the tumor — perhaps explained by
vitamin D's effects on the immune system. Compared to people with the lowest
vitamin D blood levels (around 19 ng/mL), those with mid-range levels (around
27.9 ng/mL) had only 33% of the risk of developing this type of tumor, and
those with the highest vitamin D levels (around 37.4 ng/mL) had just 10% of the
risk (Song, Gut 2015). A review of 17 studies compared the risk of colorectal
cancer in people with varying blood levels. It found that, compared to those
having levels of 20 to <25 ng/mL, the risk was 31% higher when
levels were below 12 ng/mL, but 19% lower at 30 to <35
ng/mL and 27% lower at 35 to <40 ng/mL, although there was
no statistically significant risk reduction at 40 ng/mL or greater (McCullough, J Natl Cancer Inst 2018).
In seeming contrast to this, a large, multi-year study in the
U.S. found that daily supplementation with vitamin D3 (1,000 IU) and/or calcium
(1,200 mg) did not reduce the risk of developing new precancerous colorectal
polyps (adenomas) among people who had adenomas removed in the past. There was
no statistically significant difference in the occurrence of adenomas between
those who were or were not given the supplements. However, the vast majority of
subjects began the study with adequate blood levels of vitamin D (averaging 24
to 25 ng/mL); in fact, anyone with a level below 12 ng/mL was excluded from the
study (Baron, NEJM 2015). These findings, therefore, may not apply to people with
vitamin D levels which are inadequate, i.e., under 20 ng/mL. In fact, a
large study that followed men and women in the U.S. and Canada with previously
untreated advanced or metastatic colorectal cancer for a median of 5.6 years
found that those who started chemotherapy with vitamin D blood levels of at
least 24.1 ng/mL were 19% less likely to have disease progression and 34% less
likely to die in comparison to those who were deficient in vitamin D (< 10.8
ng/mL) at the start of treatment (Yuan, Clin Cancer Res 2019).
A study of 1,666 women (average age 59) with breast
cancer found that those with higher vitamin D blood levels around the
time of diagnosis had the highest overall survival rates over an average 7
years of follow up. Nineteen percent of women with the lowest levels of vitamin
D (under 17 ng/mL) died during the follow up period, while only about 14% died
among those with higher levels. After accounting for differences in tumors and
treatments, it was calculated that women with vitamin D levels of 17 to 25
ng/mL and those with more than 25 ng/mL were, respectively, 22% and 28% less
likely to have died than women with the lowest levels. The reduction in risk
associated with vitamin D was greatest for premenopausal women. Women with
lowest blood levels of vitamin D at the time of diagnosis were more likely to
have the most advanced-staged tumors (Yao, JAMA Oncol 2016).
Somewhat similarly, an analysis in 2014 of five clinical studies found that
women who had the highest vitamin D blood levels at the time of breast cancer
diagnosis were twice as likely to survive during the studies (which lasted 5 to
20 years) as women with the lowest vitamin D levels (Mohr, Anticancer Research 2014). Due to differences in
the studies analyzed, the "low" vitamin D groups included women with
less than 14 to 30 ng/mL of vitamin D while the "high" groups
included those with more than 22 to 32.4 ng/mL.
While this association between vitamin D levels and mortality with breast
cancer is not proven to be "cause-and-effect," there is no scientific
reason to believe that breast cancer would cause a decrease in vitamin D,
suggesting a likely beneficial effect of vitamin D.
This potential beneficial link between vitamin D and breast cancer was somewhat
strengthened by analysis of a study which gave 2,000 IU daily to overweight or
obese postmenopausal women in the hope that it would aid weight loss during
dieting -- although it did not (see Mason 2014 study in "Weight
control" above). It was found that women whose vitamin D levels increased
the most or to at least 32 ng/mL had the greatest reduction in blood estrogens,
which are a known risk factor for breast cancer (Mason, Menopause 2016). However, most
of the reduction in blood estrogens appeared to be due to dieting itself,
with estrogen levels falling, on average, by about 14.5% among women who didn't
receive vitamin D compared to about 19.5% among those who did.
An analysis of data pooled from three studies
concluded that higher vitamin D blood levels "... were associated with a
dose-response decrease in breast cancer risk with concentrations ≥ 60
ng/mL being most protective." However, this is a potentially unsafe level and the conclusion is dubious. The
analysis was primarily based on data from just one of the studies, known as the
GrassrootsHealth study, which, unlike the other two, was not randomized nor
placebo-controlled and was based on self-reported health information from a
self-selected group of people interested in vitamin D. Not surprisingly, it was
also the only study that had a significant number of participants with vitamin
D levels higher than 40 ng/mL (McDonnell, PLOS One 2018).
A randomized, placebo-controlled study in Canada among 80
women with newly diagnosed invasive breast cancer and generally sufficient
blood levels of vitamin D (average 29 ng/mL) found that high-dose vitamin D3
(40,000 IU) taken daily for two to six weeks before breast cancer surgery did
not slow tumor growth. Blood levels increased to about 98.5 ng/mL
(an extremely high level) in those who took high-dose vitamin
D, and decreased somewhat, to 25 ng/mL, in those who did not. Women who took
high-dose vitamin D also experienced more fatigue than those who took a
placebo, although no serious adverse effects were reported (Arnaout, Breast Cancer Res Treat 2019).
A study in Spain found that lower levels of vitamin D in the
blood were associated with higher risks of bladder cancer. Compared
to people with vitamin D levels of 30 ng/mL or above, the risk of bladder
cancer was 83% higher among those with levels under 10 ng/mL, 67% higher among
those with levels of 10 up to 15 ng/mL, and 63% higher among those with levels
of 15 up to 20 ng/mL. There was no statistically significant difference in
risk, however, between those with levels of 20 up to 30 ng/mL compared to those
above 30 ng/mL. (Amaral, JNCI 2012). Even greater increases were found with the risk of metastatic bladder
cancer.
Pancreatic cancer
Laboratory studies suggest that vitamin D may inhibit pancreatic
cancer cell growth and a review of five large epidemiologic studies
concluded that higher levels of serum vitamin D were associated with a lower
risk of developing pancreatic cancer.27 Compared to people whose serum vitamin D levels were less
than 20 ng/mL, the risk of developing pancreatic cancer over the following 12
to 18 years was 25% lower among those with levels of 20 mg to 29 ng/mL, and 29%
lower among those with levels above 30 ng/mL.
Vitamin D inhibits prostate cancer cells in
laboratory studies. Whether or not vitamin D supplementation actually reduces
the risk of prostate cancer is not known, but some studies do suggest an
association between vitamin D levels and prostate cancer risk. For example, a
large study in the U.S. found that both low and high vitamin D
concentrations in the blood to be associated with increased risk of prostate
cancer, particularly high-grade prostate cancer. The middle "sweet
spot" associated with the lowest risk (about half the risk of the higher
or lower levels) was between 23 ng/mL and 29 ng/mL, leading the researchers to write
that the optimal range "for prostate cancer prevention may be
narrow" Kristal, Canc Epi Biomark, Prev 2014. This finding is
somewhat consistent with a smaller study of men in Chicago undergoing radical
prostatectomy (due to indications of possible cancer), in which those
found not to have advanced cancer had a median blood level of
27.0 ng/mL, which was only slightly higher than that of men with advanced
cancer (22.7 ng/mL). However, the study found that men with advanced cancer
were more likely to be Black, and the Black men were more likely to have lower
levels of vitamin D (as seen in other studies), so when the results were
analyzed just among Blacks or among whites, there was no longer an association
between vitamin D levels and advanced prostate cancer (Nyame, J Clin Oncol 2016).
A study of men aged 40 to 79 in the U.S. undergoing their first prostate biopsy
for potential cancer, found that, in African American men, having a vitamin D
level below 20 ng/mL was associated with increased odds of the biopsy showing
prostate cancer. In addition, among both European American and African American
men, having a level below 12 ng/mL was associated with a higher grade and stage
of prostate cancer (Murphy, Clin Cancer Res, 2014).
A study of male smokers in Finland concluded that "men with higher vitamin
D blood levels are at increased risk of developing prostate cancer," but
this assertion has been called misleading since the risk increased only among
men with calcium intakes of 1,338 mg per day or greater — an intake that
substantially exceeds the recommended intake for adult men (1,000 mg).
Increased calcium intake itself is a potential risk factor for prostate cancer.33, 34
Skin cancer A study of people with melanoma in
whom lesions had recently been removed found no difference in
disease-free survival with or without vitamin D
supplementation (100,000 IU every 50 days) over a course of three years,
despite that fact that half the participants started the study with a vitamin D
level of 18 ng/mL or lower (Johansson, Nutrients 2021). It should also be noted that taking single,
very-high doses of vitamin D (as was used in this study) has been associated
with adverse effects, and in many cases, taking lower, daily doses may be
preferable.
In summary, to potentially reduce the risk of cancer, it would seem
reasonable to maintain a vitamin D level above 20 ng/mL and, to reduce the risk
of death from cancer, into the upper 30's, but not necessarily higher. For
prostate cancer, the "sweet spot" may be more limited -- to between
23 ng/mL and 29 ng/mL, while for colorectal cancer it may be higher — up to 39
ng/mL. Vitamin D supplementation does not appear to increase survival rates
amount people being treated for cancer, but having a blood level of at least 24
ng/mL at the start of treatment for advanced or metastatic colorectal cancer is
associated with increased survival rates.
Overall mortality
A review of studies involving vitamin D concluded that supplementation with
vitamin D3 reduced
overall mortality among older adults significantly by 11%, while vitamin D2 had no overall effect (Chowdhury, BMJ 2014). The review also found
that, in the U.S., about 13% of all deaths could be attributable to
"suboptimal" vitamin D levels, which is even greater than the risk of
death associated with physical inactivity. The review did not define exactly
when, or how much, vitamin D is most effective, but you can find sensible
guidelines in the Summary, above.
A study that followed more than 300,000 healthy adults in the
UK for a median of 8.9 years found that the risk of dying during that period
decreased as vitamin D blood levels increased to 24 ng/mL (or to 19 ng/mL for
death from cancer) and then leveled off (Fan, J Clin Endocrinol Metab 2020).
Similarly, a study that followed 1,970 European men (ages
40 to 79) for an average of 12.3 years found that those with vitamin D blood
levels (i.e., total 25-hydroxyvitamin D levels) less than 9.3
ng/mL (i.e., severely deficient) had an 83% increased mortality risk compared
to those with highest levels (Antonio, eECE 2020).
On a similar note, an analysis of data from 3,509 patients
recovering from noncardiac surgery at the Cleveland Clinic found that those
with higher levels of vitamin D in their blood were less likely to experience
serious post-operative complications, including death (Turan, Anesth Analg 2014). In fact, compared to
the level of complications in patients with serum vitamin D levels below 13
ng/mL, the risk of having serious complications fell to 65% when vitamin D
levels were between 13 to 20 ng/mL, to 53% at levels between 20 and 27 ng/mL,
and to 44% at levels between 27 and 36 ng/mL. Interestingly, at levels above 36
ng/mL, the relative odds of complications did not fall further and rose
slightly, to 49%, consistent with other studies that have shown a reversal in
benefits with vitamin D levels above approximately 35 ng/mL. The researchers
suggest a trial be conducted in which vitamin D supplementation is given
preoperatively.
Quality
Concerns and Tests Performed:
Like other supplements, neither the FDA nor
any other federal or state agency routinely tests calcium or vitamin D
supplements for quality prior to sale. However, quality issues can include the
following:
·
Labeled Amount Does the product
really contain the labeled amount of vitamin D (and other key listed
ingredients such as calcium, magnesium, boron, and vitamin K)?
·
Purity Vitamin D
supplements for bone health often include calcium as an ingredient. Calcium may
potentially be contaminated with heavy metals such as lead, arsenic and
cadmium. In children, infants, and fetuses, even low levels of lead can
adversely affect neurobehavioral development and cognitive function. In adults,
lead at somewhat higher levels can cause elevated blood pressure, anemia, and
adversely affect the nervous and reproductive systems. Lead is of particular
concern during pregnancy as the mother can deliver it to the fetus. Arsenic is
a carcinogen and can damage organs. Cadmium is a probable carcinogen (i.e.,
cancer-causing agent), can be toxic to the kidneys, can soften the bones,
causing bone pain, and may affect fetal development.
·
Ability to Break Apart for Absorption For a tablet to be most useful, it must fully disintegrate
prior to leaving the stomach, delivering its contents for absorption in the
gut. Some tablets are not properly made and can pass through your body
completely or partially intact, depriving you of its ingredients. Remnants of
such products are sometimes found in the stool. This happens, for example, when
a tablet is too tightly compressed (too "hard") or is too thickly
coated.
ConsumerLab.com, as part of its mission to independently
evaluate products that affect health, wellness, and nutrition, purchased
vitamin D supplements (some including calcium, boron, magnesium, and/or vitamin
K) sold in the U.S. and Canada and tested them to determine whether they 1)
possessed the claimed amount and form of vitamin D, calcium, magnesium, boron,
and vitamin K, 2) were able to disintegrate fully to be available for absorption
and, 3) if they contained 250 mg of minerals per daily dosage and/or whole
herbs, were free from unacceptable levels of lead, cadmium, and arsenic
(see Testing Methods and Passing Score).
What CL
Found:
Most products contained their listed amounts
of vitamin D and other key ingredients but the following two did not and,
therefore, were Not Approved. These failures were each confirmed in a second independent
laboratory.
·
Natural Vitality Natural Calm Plus Calcium - Raspberry-Lemon
Flavor contained its
claimed amounts of calcium and magnesium, but contained a bit less vitamin D
than claimed (22.1 IU instead of 35 IU) and more than double its listed amount
of boron (198.5 mcg instead of 88.3 mcg) per teaspoon of powder. Although this
suggests a quality control problem, these discrepancies do not pose a safety
issue as the listed amounts are relatively small to start: The daily
requirement for vitamin D is 400 IU to 800 IU, and although there is no daily
requirement for boron -- because it is not essential -- most people get about
1,000 mcg to 10,0000 mcg from their diets and the daily upper tolerable intake
level for adults is even higher: 17,000 to 20,000 mcg (National Academies). (Note: In 2017 CL
tested a magnesium-only version of Natural Calm of the same
flavor and it passed testing.)
·
Thorne Basic Bone Nutrients contained its claimed amounts of calcium and magnesium,
but only 69.7% of its claimed vitamin D (348.5 IU vs. 500 IU) and just 2.2% of
its vitamin K (1 mcg versus 45 mcg). These are major discrepancies,
particularly for vitamin K, indicating that one should not rely on this product
for either of these nutrients.
Nineteen of the 21 products that ConsumerLab.com selected for
testing met all quality criteria, as did four products tested through
ConsumerLab.com's voluntary Quality Certification Program. These products were
found to contain their claimed amounts of vitamin D as well as calcium, boron,
and vitamin K, none was contaminated with heavy metals, and all tablets and
caplets disintegrated properly.
Vitamin D per pill or teaspoon
Be aware that the amount of vitamin D in a single pill, teaspoon of powder, or
liquid serving of a supplement varied tremendously across products, from as
little as 22.1 IU (Natural Vitality Natural Calm) to as much as 10,000 IU
in Bronson Vitamin D3 10,000 IU. Most products provide 100 IU to
2,000 IU of vitamin D per unit, which is more in line with what are safe and
effective doses to boost vitamin D intake to recommended levels — 600 IU except
800 IU for adults over 70 years of age and 400 IU for infants under 1 year of
age.
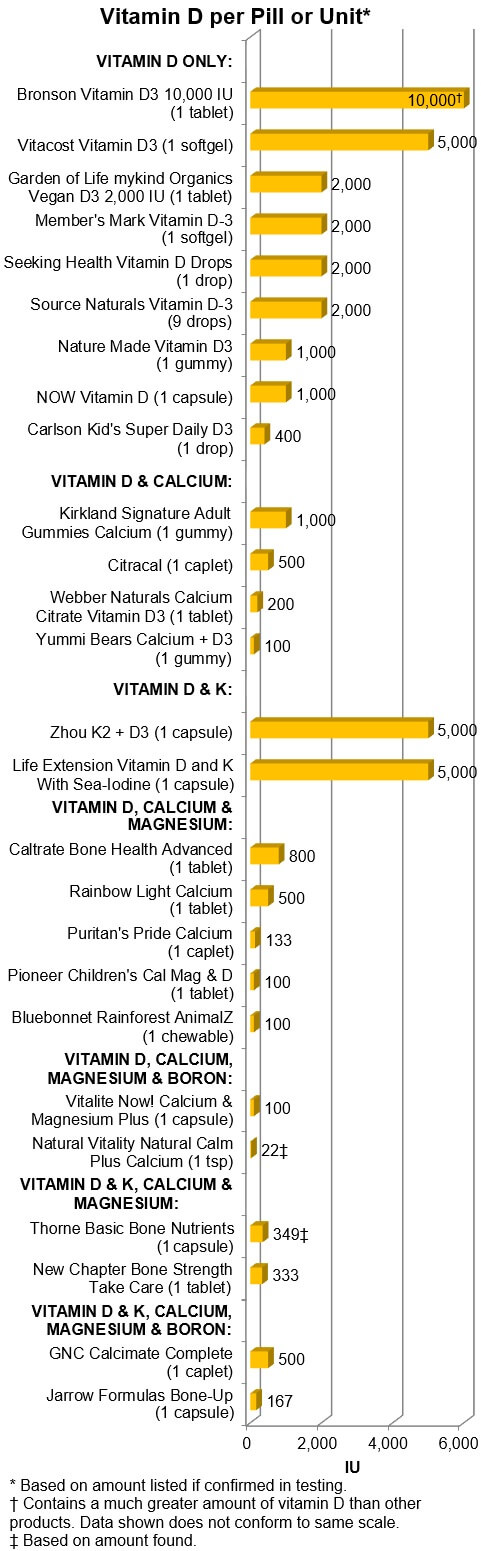
Cost
Vitamin D itself is a very inexpensive ingredient, with 400 IU costing less
than a penny from some products, as calculated and shown in the graph below. If
you are just seeking vitamin D at a dose of even 2,000 IU, you can get it for
about a dime or less. Extra ingredients and special formulations, such as
gummies, chewables, powders can raise the cost significantly, although liquid
drops tend to be more reasonably priced per dose.
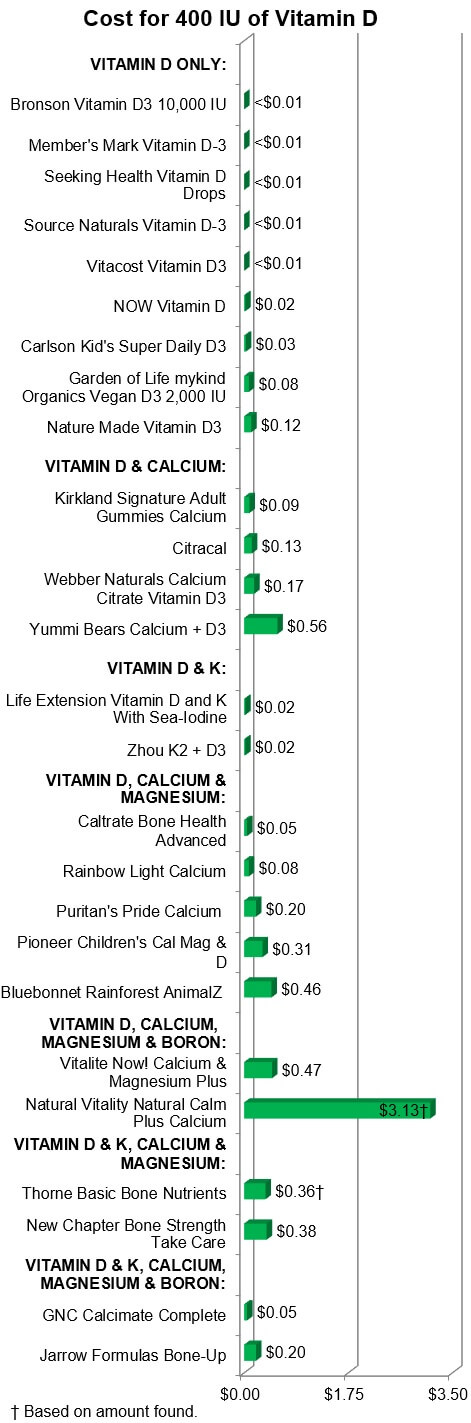
Top
Picks:
Among Approved products, ConsumerLab.com chose
several as Top Picks (see below). To be
a CL Top Pick, a Vitamin D supplement had to pass ConsumerLab's
tests of quality, provide a reasonable dose, and offer good value (i.e., a
favorable price). In combination products, amounts of other ingredients were
also considered.
Keep in mind that unless your blood level of vitamin D (25-hydroxy vitamin D)
is under 20 ng/mL, you may not need a supplement and most children and adults
require only 600 IU
of vitamin D per day (800 IU if you're over 70). The established daily upper
tolerable intake level (the "upper limit") for adults is 4,000 IU per
day and there are risks from getting too much vitamin D — it's probably best
not to take more than 2,000 IU per day (see How Much Is Too Much and Cautions and Concerns for more information).
For combination products, be aware that most adults need a total of 1,000 to
1,200 mg of calcium, 90 to 120 mcg of vitamin K, and 310 to 420 mg magnesium
from their total daily diets, which likely is already providing most or all of
this. Some supplements provide much more of these other ingredients than you
need. As to boron, it is not clear if you need it, but products that include a
few thousand micrograms (i.e., a few milligrams) are safe.
Vitamin D Only:
·
Overall Top Pick: Source Naturals Vitamin D-3 liquid
drops. This is an excellent choice because you can easily adjust your dose to
suit your current needs and those of other family members. One drop provides
222 IU of vitamin D3 for just a fraction of a cent. If you need a higher dose,
you can get 2,000 IU from 9 drops (which is the suggested daily serving size on
the label) at a cost of just 2 cents. The drops have a mild lemon-orange flavor
and can be added to food or beverages — preferably consumed as part of a meal
containing fats or oils to aid vitamin D absorption (as would be the case with
any vitamin D supplement). If you have trouble using the dropper and are prone
to squeeze out more drops than you need, consider one of the other liquids
which have special tops that pour out drops.
As vitamin D supplements can slowly lose potency after they are opened, consider refrigerating
your vitamin D supplement (to slow the loss) if you won't use it up before its
listed expiration date (usually about 2 years from the date of manufacture).
One bottle of Source Naturals provides 695 servings (each
serving consisting of 9 drops providing 2,000 IU), so if you are only using,
for example, 3 drops (667 IU) daily, a bottle could potentially last for more
than five years.
·
Low-Dose: Again, Source
Naturals Vitamin D-3 liquid drops, since you can get as little as
222 IU by taking just one drop, costing a fraction of a cent. Carlson
Kid's Super Daily D3 is another very good choice, providing 400 IU
per drop — which is 2/3 of the daily requirement for most adults and children
and 100% of that for infants. The Carlson drops have no taste
at all and the cost is 3 cents per drop. One bottle provides enough 400 IU
daily doses for an entire year.
·
Moderate Dose: Again, Source
Naturals Vitamin D-3 is a good choice to get hundreds of IUs of
vitamin D3 at little cost.
·
High Dose: If you want 2,000
IU, you can consider the liquids discussed above or Seeking Health
Vitamin D Drops, which is just as inexpensive as Source Naturals but
provides 2,000 IU in a single drop, for 2 cents, as opposed to
9 drops with Source Naturals -- so be careful not take more
than one drop of Seeking Health. Alternatively, you can take a
single softgel of Member's Mark [Sam's Club] Vitamin D-3 2000 IU —
each costs just 2 cents.
·
Very High Dose: Vitacost
Vitamin D3 medium sized softgels each provide 5,000 IU of vitamin
D for just 3 cents each. Be aware that these exceed the safe upper
tolerable intake for vitamin D of 4,000 IU.
·
Extremely High Dose: Bronson
Vitamin D3 10,000 IU. Each capsule provides 10,000 IU of
vitamin D3 for 6 cents. This is a potentially dangerous dose and should not be
taken more than every several days. It is best to avoid such a high dose, which
should only be considered when a person is known to be severely deficient in
vitamin D unlikely to reliably take a daily vitamin D supplement.
Children's Products Containing Vitamin D: Carlson Kid's
Super Daily provides 400 IU per
drop and has no taste, so it can easily be added to foods and beverages.
Alternatively, at somewhat lower cost, consider giving one or two drops (222 IU
to 444 IU) of Source Naturals D-3. Another good quality drop for
children is Baby Ddrops Vitamin D3, which we tested in 2017, but
these cost about 20 per drop -- rather than 3 cents for Carlson.
Vitamin D and Calcium: Bayer Citracal Petites provide
400 mg of calcium (from calcium citrate) and 500 IU of vitamin D per 2 caplet
serving for 16 cents. This is a little less than half the daily requirement for
calcium, as well as enough vitamin D to boost someone who's a little low in
vitamin D. Note that, despite the product name, that the caplet size is large,
although narrow. If you live in Canada, Webber Naturals Calcium Citrate
Vitamin D3 is also Top Pick in this category,
providing 300 mg of calcium (from calcium citrate) and 200 IU of vitamin D for
9 cents.
Children's Vitamin D and Calcium: Our Top Pick,
although pricey, is Yummi Bears Calcium + D3, which provide 376 mg
of calcium (from tricalcium phosphate) and 300 IU of vitamin D3 per 3 gummy
bears for 42 cents. (Although not tested this year, a less expensive option
is L'il Critters Calcium & D3, which was tested and approved in
2017, and provides 200 mg of calcium (from tricalcium phosphate) and 220 IU of
vitamin D3 per 2 gummies for just 10 cents). We are not big fans of gummies for
several reasons, including the fact that they may over-consumed as candy,
resulting in overdosing. But if gummies are the only way to get a kid who
otherwise won't get enough nutrients from foods or non-sweetened supplements to
meet the daily requirements, they are a reasonable option.
Vitamin D and Vitamin K: Although both of the products we tested in
this category (Life Extension Vitamin D and K With Sea-Iodine and Zhou
K2 + D3) passed testing, neither is a Top Pick for
regular use as they both provide 5,000 IU of vitamin D, a very large does that
exceeds the upper tolerable intake level of 4,000 IU per day. In
addition, Life Extension provides a very large amount of
vitamin K — a total of 2,100 mcg, which is many times the daily 90 mcg to 120
mcg that is adequate for women and men, respectively. The likely basis for this
are studies suggesting that very high-dose vitamin K over long periods of time
may further strengthen bones, as discussed earlier. Life Extension also
contains a very large amount of iodine -- several times the daily requirement
and approaching the tolerable upper intake level for adults.
Although not tested this year, NOW Vitamin D-3 & K-2, a capsule
that provides 1,000 IU of vitamin D and 45 mcg of vitamin K (as MK-4 K2) for 7
cents passed our tests in 2017 and would be a reasonable choice if you are just
looking to boost your vitamin K intake to an adequate level while getting a bit
over the daily requirement of vitamin D. (See the Vitamin K Review for more
information about forms of Vitamin K).
Vitamin D, Calcium and Vitamin K: We didn't test any products in
this category this year. However, if this is combination you want, Viactiv
Calcium Plus D, which passed our tests in 2017, provides 500 mg of calcium
(from calcium carbonate), 500 IU vitamin D3 and 40 mcg vitamin K1 (about half
the recommended intake for women and
one-third the recommended intake for men) for 10 cents per soft chew.
Children's Products Containing Vitamin D, Calcium, and Magnesium: Similar
to the adult products in this category, both of the products that we tested for
children primarily use calcium carbonate and magnesium oxide. Both provide the
same amounts of calcium (250 mg) and vitamin D (200 IU) and similar amounts of
magnesium per two chewable tablets. Our Top Pick is Pioneer
Children's Cal Mag & D as it is less expensive (15 cents)
than Bluebonnet Rainforest AnimalZ (23 cents). Pioneer is
vanilla flavored while Bluebonnet is cocoa flavored.
Vitamin D, Calcium, Magnesium and Boron: Vitalite Now! Calcium
& Magnesium Plus provides calcium (250 mg), magnesium (125 mg),
and boron (1,000 mcg) in each capsule, as well as a modest amount of vitamin D
(100 IU). Although the label suggests taking four capsules daily (for a
relatively high daily cost of 48 cents), fewer capsules would be sufficient for
most people with regard to the three minerals, although not necessarily for
vitamin D. The source of calcium is a list of nearly every form of calcium, but
carbonate is the first and may be the main form, so it is important to take
this product with a meal, which you should anyhow to maximize vitamin D
absorption.
Vitamin D, Calcium, Magnesium, and Vitamin K: Only one of two
products in this category passed our tests: New Chapter Bone Strength
Take Care However, due to its high cost, it is not a Top Pick.
The suggested daily serving of 3 tablets provides 1,000 IU of vitamin D, 770 mg
of calcium, 80 mcg of vitamin K from K1 and K2, and a modest amount of
magnesium. It is best to break this into two or three servings to be taken with
meal during the day, as 770 mg of calcium is too much to take at one time. This
is a relatively expensive product at 96 cents per day and, considering that
there is no compelling research showing superiority of algae-based calcium or
magnesium, you can easily get these same ingredients for less by purchasing the
ingredients separately.
Vitamin D, Calcium, Magnesium, Boron, and Vitamin K: Both of the
products that we tested in this category, GNC Calcimate and Jarrow
Formulas Bone Up, provide significant amounts of calcium, vitamin K, and
boron. What sets them apart is the amount of magnesium they provide, with Jarrow providing
several times as much as GNC as well as a daily dose of
vitamin D (1,000 IU) that is closer to the adult requirement (600 IU to 800 IU)
than GNC's 2,000 IU. Although costs more (51 cents daily for 6
pills versus 25 cents daily for 4 pills), Jarrow Formulas Bone Up is
our Top Pick for this category. With either product, consider
cutting the suggest dose in half if you are just trying to boost your intake of
these nutrients and not trying to fulfill the majority of the daily
requirements from a supplement. By the way, Jarrow Formulas Bone-Up provides
calcium as StimuCal microcrystalline hydroxyapatite — see What to Consider When Buying for more about this
ingredient.
Test
Results by Product:
Listed below are the test results for 26
supplements containing vitamin D. Products are grouped by main ingredients, and
there are subgroupings for children's products. Within each group, products are
listed alphabetically. ConsumerLab.com selected 21 of these products. Four
other products (each indicated with a CL flask) were tested at the request of
their manufacturers/distributors through CL's voluntary Quality Certification Program and are included
for having passed testing.
Shown for each product are the claimed amount and form of the tested
ingredient(s), serving size recommended on its label, pill size, price
information and, for comparison purposes, the cost per 400 IU of vitamin D.
Products listed as "Approved" met their label claims and
ConsumerLab.com's quality criteria (see Passing Score). The full list of ingredients is available for each product in
the last column.
Jump to results by ingredient:
·
Vitamin D Only: Pills/Gummies
·
Children's Vitamin D and Calcium:
·
Vitamin D, Calcium, and Magnesium
·
Children's Vitamin D, Calcium, and Magnesium
·
Vitamin D, Calcium, Magnesium, and Boron
·
Vitamin D, Calcium, Magnesium, and Vitamin K
·
Vitamin D, Calcium, Magnesium, Boron, and Vitamin K
Results
of ConsumerLab.com Testing of VITAMIN D SUPPLEMENTS
(INCLUDING COMBINATIONS WITH CALCIUM,
MAGNESIUM, BORON AND/OR VITAMIN K)
(Click arrows or swipe left or right to see
all columns)
Approval Statusⓘ
Product Name
Claimed Amount of and Form
of Vitamin D, Calcium, Magnesium, Boron & Vitamin K Per Servingⓘ
Heavy Metalsⓘ
Suggested Daily Serving on
Label
Pill Sizeⓘ
Cost for Suggested Serving
[Price per 400 IU (10 mcg) Vitamin D]
Price
Notable Features
Full List of Ingredients
Per Serving
APPROVED
Top
Pick
for extremely high dose
vitamin D only
Bronson® Vitamin D3 10,000
IU
Dist. by Bronson
Laboratories
1 tablet
10,000 IU (250 mcg)>UL
(D3)
✔
Heavy metals: NA
Also tested for disintegrationⓘ
As a dietary supplement for
adults, take 1 tablet daily, preferably with a meal, or as directed by a
healthcare professional.
Medium circular organic
1 tablet
$0.06
[<$0.01]
$19.99/360 organic tablets
USDA Organic seal. Non-GMO.
Gluten-free. Soy-free. Wheat-free. Nut-free.
1 tablet
Vitamin D3 (as cholecalciferol) 250 mcg (10,000 IU).
Other Ingredients: Organic corn maltodextrin, organic potato starch, organic
corn syrup solids, more...
APPROVED
Garden of Life® mykind
Organics Vegan D3 2,000 IU![]()
Dist. by Garden of Life LLC
1 tablet
2,000 IU (50 mcg)
(D3)
✔
Heavy metals: Pass
Adults chew 1 tablet daily.
Children 4 years and older chew 1 tablet under adult supervision.
Medium/large circular vegan chewable tablet
1 tablet
$0.42
[$0.08]
$12.59/30 vegan chewable tablets
Certified organic food
blend 180 mg, certified organic mushroom blend 50 mg
Kosher. USDA Organic seal. Non GMO Project Verified seal. Certified Vegan
Vegan.org seal. Gluten-Free.
1 tablet
Vitamin D (as D3 from Lichen) 2,000 IU, Certified Organic Food Blend [Organic
Flax (seed), Organic Carrot (root), Organic Broccoli (flower & stem),
Organic Cauliflower (flower & stem), Organic Spinach (leaf)] 180 mg, more...
APPROVED
Top
Pick
for high dose vitamin D
only
Member's Mark® [Sam's Club]
Vitamin D-3
Dist. by Sam's West, Inc.
1 softgel
2,000 IU (50 mcg)
(D3)
✔
Heavy metals: NA
For adults, take one (1)
softgel daily, preferably with a meal.
Medium softgel
1 softgel
$0.02
[<$0.01]
$8.33/400 softgels
No gluten. No yeast. No
wheat. No milk or milk derivatives. No lactose. No sugar. No preservatives. No
artificial color. No artificial flavor. No sodium (less than 5 mg per serving).
Gluten free.
1 softgel
Vitamin D (as D3 Cholecalciferol) 2,000 IU.
Other Ingredients: Soybean oil, gelatin, glycerin, corn oil.
APPROVED
Nature Made® Vitamin D3
Dist. by Nature Made
Nutritional Products
2 gummies
2,000 IU (50 mcg)
(D3)
✔
Heavy metals: NA
Adults, chew 2 gummies
daily.
Medium/large gumdrop shaped gummy
2 gummies
$0.60
[$0.12]
$26.98/90 gummies
No artificial flavors -
natural fruit flavors. No synthetic dyes - colors derived from natural sources.
No high fructose corn syrup. No artificial sweeteners. Gluten free.
2 gummies
Calories 15, Total Carbohydrate 4 g, Total Sugars [Includes 2 g Added Sugars] 2
g, Vitamin D3 (as Cholecalciferol) 50 mcg (2,000 IU).
Other Ingredients: Glucose syrup, sugar, more...
APPROVED
NOW® Vitamin D
Dist. by NOW Foods
1 capsule
1,000 IU (25 mcg)
(D2)
✔
Heavy metals: NA
Take 1 capsule daily with a
meal.
Medium/large veg capsule
1 capsule
$0.04
[$0.02]
$4.86/120 veg capsules
Kosher. Non-GMO. Not
manufactured with wheat, gluten, soy, milk, egg, fish, shellfish or tree nut
ingredients.
1 capsule
Vitamin D2 (as Ergocalciferol) 25 mcg (1,000 IU).
Other Ingredients: Rice flour, hypromellose (cellulose capsule), magnesium
stearate (vegetable source) and silica.
APPROVED
Top
Pick
for very high dose vitamin
D only
Vitacost Vitamin D3
Dist. by Vitacost.com
1 softgel
5,000 IU (125mcg)>UL
(D3)
✔
Heavy metals: NA
As A Dietary Supplement For
Adults 18 Years Of Age And Over, Take 1 Softgel Daily Or As Directed By A
Healthcare Professional.
Medium softgel
1 softgel
$0.03
[<$0.01]
$6.69/20 softgels
Free of: milk, eggs,
peanuts, tree nuts, crustacean shellfish, fish, soy, gluten, titanium dioxide.
1 softgel
Vitamin D (as cholecalciferol, D3) 5,000 IU.
Other Ingredients: Safflower oil, corn oil, gelatin, glycerin and water.
APPROVED
Seeking Health® Vitamin D
Dropsⓘ![]()
Dist. by Seeking Health,
LLC
1 drop [0.033 ml]
2,000 IU (50 mcg)
(D3)
✔
Heavy metals: NA
Carefully dispense one drop
and take by mouth daily, or use as directed by your healthcare professional.
Liquid from bottle
1 drop
$0.02
[<$0.01]
$19.95/1 fl oz. [30 ml] bottle (approx. 900 servings)
Does Not Contain: Milk,
eggs, fish, shellfish, tree nuts, peanuts, wheat, soy, gluten, GMO, sweeteners,
flavors, colors, or preservatives.
1 drop
Calories 0, Total Fat 0 g, Cholesterol 0 mg, Vitamin D3 (as cholecalciferol) 50
mcg (2,000 IU).
Other Ingredients: Olive oil.
APPROVED
Top
Pick
for vitamin D only
Source Naturals® Vitamin
D-3
Dist. by Source Naturals,
Inc.
9 drops [0.17 ml]
2,000 IU (50 mcg)
(D3)
✔
Heavy metals: NA
9 drops once daily in a
drink.
Liquid from bottle
9 drops
$0.02
[<$0.01]
$13.29/4 fl oz. [118.28 ml] bottle (approx. 695 servings)
Contains no yeast, dairy,
egg, gluten, corn, soy or wheat. Contains no sugar, starch, salt,
preservatives, or artificial color, flavor or fragrance.
9 drops
Vitamin D-3 (as cholecalciferol) 2,000 IU.
Other Ingredients: Medium chain triglycerides, orange and lemon essential oils.
Children's Products Containing Vitamin D:
APPROVED
Top
Pick
for children's vitamin D
only
Carlson® Kid's Super Daily®
D3
Dist. by Carlson Div. of
J.R. Carlson Laboratories, Inc.
1 drop [0.028 ml]
400 IU (10 mcg)
(D3)
✔
Heavy metals: NA
Children two years of age
or older: give one drop daily or as directed by your healthcare professional.
Liquid from bottle
1 drop
$0.03
[$0.03]
$9.68/0.35 fl. oz. [10.3 ml] bottle (approx. 365 servings)
Gluten-free. Soy-free. No
artificial preservatives.
1 drop
Vitamin D (as cholecalciferol) (400 IU) 10 mcg.
Other Ingredients: Medium chain triglyceride oil (coconut and pal source).
APPROVED
Top
Pick
for vitamin D & calcium
Bayer Citracal® Petites
Dist. by Bayer HealthCare
LLC
2 caplets
500 IU (12.5 mcg)
(D3)
✔
400 mg
(calcium citrate)
✔
Heavy metals: Pass
Also tested for disintegrationⓘ
Adults: Take 1 serving (2
caplets) twice daily with or without food or as recommended by your physician,
pharmacist, or health care professional.
Large coated caplet
2 caplets
$0.16
[$0.13]
$8.24/100 coated caplets
None.
2 caplets
Vitamin D (as cholecalciferol) 500 IU, Calcium (element) 400 mg.
Ingredients: Calcium citrate, polyethylene glycol, croscarmellose sodium,
hydroxypropyl methylcellulose, magnesium silicate, more...
APPROVED
Kirkland Signature™
[Costco] Adult Gummies Calcium
Dist. by Costco Wholesale
Corporation
2 gummies
1,000 IU (25 mcg)
(D3)
✔
500 mg
(tribasic calcium phosphate)
✔
Heavy metals: Pass
As a dietary supplement for
adults, chew two (2) gummies daily, preferably with a meal.
Very large gumdrop shaped gummy
2 gummies
$0.22
[$0.09]
$12.99/120 gummies
USP® dietary supplement
verified seal. No preservatives. No artificial flavors. No yeast or gluten. No
lactose.
2 gummies
Calories 20, Total Carbohydrate 5 g, Total Sugars [Includes 3 g Added Sugars] 3
g, Vitamin D 25 mcg (1,000 IU), Calcium 500 mg, Phosphorus 230 mg.
Ingredients: Sugar, corn syrup, tribasic calcium phosphate, water, more...
APPROVED
Webber Naturals® Calcium
Citrate Vitamin D3![]()
Dist. by WN
Pharmaceuticals® Ltd.
1 tablet
200 IU (5 mcg)
(D3)
✔
300 mg
(calcium citrate)
✔
Heavy metals: Pass
Also tested for disintegrationⓘ
2-4 tablets daily, a few
hours before or after taking other medications, or as directed by a physician.
Large tablet
1 tablet
$0.09
[$0.17]
$29.99/350 tablets
Free of artificial colours,
preservatives or sweeteners; no dairy, sugar, wheat, gluten, yeast, soy, egg,
fish, shellfish, salt, tree nuts or GMOs. Suitable for vegetarians.
1 tablet
Calcium (citrate) 300 mg, Vitamin D3 (cholecalciferol) 200 IU (5 mcg).
Non-medicinal Ingredients: Coating (carbohydrate gum, glycerin), croscarmellose
sodium, vegetable grade magnesium stearate (lubricant).
Children's Products Containing Vitamin D & Calcium:
APPROVED
Top
Pick
for children vitamin D
& calcium
Yummi Bears® Calcium + D3
Dist. by Hero Nutritionals,
Inc.
3 gummies
300 IU (7.5 mcg)
(D3)
✔
375 mg
(tricalcium phosphate)
✔
Heavy metals: Pass
As a dietary supplement,
give each child three (3) bears per day.
Large bear shaped gummy
3 gummies
$0.42
[$0.56]
$12.61/90 gummies
Phosphorus 175 mg
Vegetarian approved. Free of: GMOs, gluten, yeast, wheat, dairy, eggs, soy,
tree nuts, peanuts, shellfish, fish, gelatin, artificial flavors, artificial
colors and artificial preservatives.
3 gummies
Calories 20, Total Carbohydrate 5 g, Sugars 4 g, Vitamin D (Vitamin D3 as
cholecalciferol USP) 300 IU, Calcium (as tricalcium phosphate) 375 mg,
Phosphorus (as tricalcium phosphate) 175 mg.
Other Ingredients: Organic tapioca syrup, natural cane sugar, more...
APPROVED
Life Extension® Vitamin D
and K With Sea-Iodine™
Dist. by Quality
Supplements and Vitamins, Inc.
1 capsule
5,000 IU (125 mcg)>UL
(D3)
✔
1,000 mcg
(K1)
1,000 mcg
(MK-4 K2)
100 mcg
(MK-7 K2)
2,100 mcg
(total vitamin K)
✔
Heavy metals: NA
Take one (1) capsule once
daily with food, or as recommended by a healthcare practitioner.
Medium/large capsule
1 capsule
$0.30
[$0.02]
$18.00/60 capsules
Iodine™ complex blend 1,000
mcg>UL
1 capsule
Vitamin D3 (as cholecalciferol) 5,000 IU, Vitamin K activity from: [Vitamin K1
(phytonadione) 1,000 mcg, Vitamin K2 (as menaquinone-4) 1,000 mcg, Vitamin K2
(as all-trans menaquinone-7) 100 mcg] 2,100 mcg, more...
APPROVED
Zhou® K2 + D3
Dist. by Zhou Nutrition®
1 capsule
5,000 IU (125 mcg)>UL
(D3)
✔
90 mcg
(MK-7 K2)
✔
Heavy metals: NA
Take 1 vegetable capsule
with food once daily or as directed by your healthcare professional.
Large veggie capsule
1 capsule
$0.26
[$0.02]
$15.64/60 veggie capsules
Zero gluten, soy, milk,
eggs, fish, shellfish, tree nuts, peanuts & wheat. Made with non-GMO
ingredients.
1 capsule
Vitamin D3 (as Cholecalciferol) 5,000 IU, Vitamin K2 (as Menaquinone) (MK-7) 90
mcg.
Other Ingredients: Rice flour, cellulose (vegetable capsule).
Vitamin D, Calcium & Magnesium:
APPROVED
Caltrate® Bone Health
Advanced
Dist. by Pfizer
1 tablet
800 IU (20 mcg)
(D3)
✔
600 mg
(calcium carbonate)
✔
40 mg
(magnesium oxide)
✔
Heavy metals: Pass
Take one (1) chewable
tablet up to two times daily with or without food or as directed by your
physician.
Medium/large circular chewable tablet
1 tablet
$0.10
[$0.05]
$14.97/155 chewable tablets
None.
1 tablet
Calories 0, Total Carbohydrates <1 g, Total Sugars [Includes 0 g Added
Sugars] 0 g, Sugar Alcohol <1 g, Vitamin D3 20 mcg (800 IU), Calcium 600 mg,
Magnesium 40 mg, Zinc 7.5 mg, Copper 0.25 mg, Manganese 1.8 mg, more...
APPROVED
Top
Pick
for vitamin D, calcium
& magnesium
Puritan's Pride® Calcium
Magnesium Vitamin D3![]()
Dist. by Puritan's Pride,
Inc.
3 caplets
400 IU (10 mcg)
(D3)
✔
1,000 mg
(calcium from oyster shell)
✔
500 mg>UL
(magnesium oxide)
✔
Heavy metals: Pass
Also tested for disintegrationⓘ
For adults, take three (3)
caplets daily, preferably with meals.
Large coated caplet
3 caplets
$0.20
[$0.20]
$7.99/120 coated caplets
No artificial flavor, no
artificial sweetener, no preservatives, no sugar, no milk, no lactose, no soy,
no gluten, no wheat, no yeast. Sodium free.
3 caplets
Vitamin D (as D3 Cholecalciferol) 10 mcg (400 IU), Calcium (as Oyster Shell)
1,000 mg, Magnesium (as Magnesium Oxide) 500 mg.
Other Ingredients: Vegetable cellulose, contains <2% of: natural palm leaf
glaze, polydextrose, titanium dioxide color, triacetin, more...
APPROVED
Rainbow Light® Food-Based
Calcium™ With Magnesium & Vitamin D3
Dist. by Rainbow Light
Nutritional Systems®
1 tablet
500 IU (12.5 mcg)
(D3)
✔
500 mg
(calcium carbonate, amino acid chelate, citrate-malate)
✔
250 mgⓘ
(magnesium oxide, aspartate)
✔
Heavy metals: Pass
Also tested for disintegrationⓘ
For pure and potent
protection, take one tablet per day, with or between meals. May take 2 per day
in divided doses for advanced usage.
Large tablet
1 tablet
$0.10
[$0.08]
$17.99/180 tablets
Betaine HCl 20 mg, stinging
nettle [tops] 20 mg, horsetail [whole herb] 20 mg, organic spirulina 20 mg
Free of gluten, wheat, milk/dairy, nuts, soy, eggs, fish, shellfish, yeast,
sugar, artificial additives.
1 tablet
Calcium (as Carbonate, Amino Acid Chelate, Citrate-Malate) 500 mg, Magnesium
(as Oxide, Aspartate) 250 mg, Vitamin D (as D3 Cholecalciferol) 500 IU, Betaine
HCl 20 mg, Stinging Nettle [tops] 20 mg, Horsetail [whole herb] 20 mg, Organic
Spirulina 20 mg, more...
Children's Products Containing Vitamin D, Calcium &
Magnesium:
APPROVED
Bluebonnet Rainforest
AnimalZ® Calcium Magnesium & Vitamin D3 - Vanilla Frosting Flavor
Dist. by Bluebonnet
Nutrition Corporation
2 chewables
200 IU (5 mcg)
(D3)
✔
250 mg
(calcium carbonate, citrate, malate)
✔
50 mg
(magnesium oxide, bisglycinate chelate)
✔
Heavy metals: Pass
As a dietary supplement for
children three years of age or older, take two animal-shaped chewables once
daily or as directed by a healthcare practitioner.
Medium/large animal-shaped chewable tablet
2 chewables
$0.23
[$0.46]
$10.24/90 chewables
Super fruit and veggie
blend 30 mg
Kosher. Gluten free. Free of milk, egg, fish, crustacean shellfish, tree
nuts, peanuts, peanuts, wheat and soybeans. Also free of yeast, gluten, barley
and sodium.
2 chewables
Calories 6, Total Carbohydrate 1.5 g, Sugars [Includes 1.5 g added sugars] 1.5
g, Vitamin D3 (as 200 IU cholecalciferol) 5 mcg, Calcium (as carbonate,
citrate, malate) 250 mg, Magnesium (as oxide, bisglycinate chelate) 50 mg, more...
APPROVED
Top
Pick
for children vitamin D,
calcium & magnesium
Pioneer® Children's Cal Mag
& D - Cocoa
Mfd. by Healthway Corp.
2 tablets
200 IU (5 mcg)
(D3)
✔
250 mg
(calcium carbonate, citrate)
✔
85 mg
(magnesium oxide, citrate)
✔
Heavy metals: Pass
Children ages 4-8: Two
chewables once daily. Children ages 9-13: Two chewables two times daily.
Medium/large circular chewable tablet
2 tablets
$0.15
[$0.31]
$9.18/120 chewable tablets
Trace mineral complex 10 mg
Gluten free. Product contains no added artificial colors or flavors.
Formulated to be free of dairy.
2 chewables
Calories 5, Total Carbohydrate 2 g, Sugar Alcohol 1 g, Vitamin D-3 (from
cholecalciferol) 200 IU, Calcium (3:1 from carbonate: citrate) 250 mg,
Magnesium (2:1 from oxide: citrate) 85 mg, Trace Mineral Complex (from sea
vegetation: Lithothamnion spp.) 10 mg, more...
Vitamin D, Calcium, Magnesium & Boron:
NOT APPROVED
Natural Vitality® Natural
Calm Plus Calcium - Raspberry-Lemon Flavor
Dist. by Natural Vitality
1 teaspoons [2.5 g]
35 IU (2.6 mcg)
(D3)
Found only 22.1 IU (0.55 mcg) vitamin D per
serving (63.1% of listed amount)
70 mg
(calcium gluconate)
✔
106.7 mg
(magnesium citrate)
✔
88.3 mcg
(boron citrate)
Found 198.5 mcg boron per serving (224.7% of
listed amount)
Heavy metals: Pass
Take 1 - 1 1/2 rounded
teaspoons twice per day at any time, at least 5 hours apart.
Powder in container
1 teaspoon
$0.52
[$1.98 based on amount listed]
[$3.13 based on amount found]
$15.57/8 oz [226 g] container (approx. 90 servings)
Vitamin C 88.3 mg,
potassium (elemental from potassium citrate) 35 mg
Vegetarian. Gluten-Free. Non GMO Project Verified seal. Contains no yeast,
dairy, egg, gluten, soy, wheat, sugar, starch, preservatives or artificial
color or flavor.
1 teaspoon
Vitamin C (as ascorbic acid) 88.3 mg, Vitamin D3 (as cholecalciferol) 35 IU,
Calcium (elemental from calcium gluconate) 70 mg, Magnesium (elemental from
magnesium citrate) 106.7 mg, Potassium (elemental from potassium citrate) 35
mg, Boron (elemental from boron citrate) 88.3 mcg.
Ingredients: Calcium gluconate, more...
APPROVED
Top
Pick
for vitamin D, calcium,
magnesium & boron
Vitalite Now! Calcium &
Magnesium Plus
Dist. by Vitalite Now!
4 capsules
400 IU (10 mcg)
(D3)
✔
1,000 mg
(calcium carbonate, dicalcium phosphate, citrate, amino acid chelate,
hydroxyapatite, gluconate, lactate, orotate, succinate and alpha ketoglutarate)
✔
500 mg>UL
(magnesium oxide)
✔
4,000 mcg
(boron amino acid chelate)
✔
Heavy metals: Pass
4 capsules daily preferably
with meals or as directed by a healthcare professional.
Large capsule
4 capsules
$0.47
[$0.47]
$27.90/240 capsules
Phosphorus 77 mg
Precaution: This product is manufactured and packaged in a facility
which may also process milk, soy, wheat, egg, peanuts, tree nuts, fish and
crustacean shellfish.
4 capsules
Vitamin D-3 (cholecalciferol) 400 IU, Calcium (from carbonate, dicalcium
phosphate, citrate, amino acid chelate, hydroxyapatite, gluconate, lactate,
orotate, succinate and alpha ketoglutarate) 1,000 mg, Phosphorus (dicalcium
phosphate) 77 mg, Magnesium (from oxide) 500 mg, Boron (from amino acid
chelate) 4 mg.
Other Ingredients: Gelatin (bovine), vegetable magnesium stearate and rice
flour.
Vitamin D, Calcium, Magnesium & Vitamin K:
APPROVED
New Chapter® Bone Strength
Take Care™
Dist. by New Chapter, Inc.
3 tablets
1,000 IU (25 mcg)
(D3)
✔
770 mg
(calcium from algae Lithothamnion calcareum & corallioides)
✔
58 mg
(magnesium from algae Lithothamnion calcareum & corallioides)
✔
35 mcg
(K1)
45 mcg
(MK-7 K2)
80 mcg
(total vitamin K)
✔
Heavy metals: Pass
Also tested for disintegrationⓘ
Three tablets daily with
food.
Large slim tablet
3 tablets
$0.96
[$0.38]
$38.37/120 slim tablets
Strontium 5 mg, silica 2
mg, vanadium 13 mcg
Kosher. Non GMO Project Verified seal. Gluten free; 100% vegetarian; no
artificial flavors or colors.
Precaution: Contains: Fermented soy.
3 tablets
Vitamin D3 (as cholecalciferol from ferment media) 1,000 IU, Vitamin K1 (as
phylloquinone from ferment media) 35 mcg, Vitamin K2 (as menaquinone-7 from
natto) 45 mcg, Calcium (from algae Lithothamnion calcareum & corallioides)
770 mg, Magnesium (from algae Lithothamnion calcareum & corallioides)
58 mg, Strontium (from algae Lithothamnion calcareum & corallioides)
5 mg, Silica (from algae Lithothamnion calcareum & corallioides)
2 mg, Vanadium (from algae Lithothamnion calcareum & corallioides) 13 mcg, more...
NOT APPROVED
Thorne® Basic Bone
Nutrients
Mfd. by Thorne Research,
Inc.
1 capsule
500 IU (12.5 mcg)
(D3)
Found only 348.5 IU vitamin D per serving (69.7%
of listed amount)
200 mg
(DimaCal® DiCalcium Malate)
✔
50 mg
(Albion® DiMagnesium Malate)
✔
45 mcg
(MK-7 K2)
Found only 1 mcg vitamin K per serving (2.2% of
listed amount)
Heavy metals: Pass
Take 1 capsule one to four
times daily or as recommended by a health-care practitioner.
Large capsule
1 capsule
$0.32
[$0.25 based on amount listed]
[$0.36 based on amount found]
$38.00/120 capsules
Gluten Free.
1 capsule
Vitamin D (as Vitamin D3) (500 IU) 12.5 mcg, Vitamin K (as K2 (MK-7)) 45 mcg,
Calcium (as DimaCal® DiCalcium Malate) 200 mg, Magnesium (as Albion®
DiMagnesium Malate) 50 mg.
Other Ingredients: Hypromellose (derived from cellulose) capsule, calcium
laurate.
Vitamin D, Calcium, Magnesium, Boron & Vitamin K:
APPROVED
Dist. by General Nutrition
Corporation
4 caplets
2,000 IU (50 mcg)
(D3)
✔
800 mg
(calcium citrate malate)
✔
100 mg
(magnesium oxide)
✔
1,000 mcg
(boron hydrolyzed protein chelate)
✔
50 mcg
(K2)
✔
Heavy metals: Pass
Also tested for disintegrationⓘ
As a dietary supplement,
take two caplets at breakfast and two caplets at dinner for a total of four
caplets daily.
Large caplet
4 caplets
$0.25
[$0.05]
$14.99/240 caplets
Zinc 7.5 mg, copper 1 mg,
manganese 1 mg, MBP® 40 mg
No artificial colors, no artificial flavors, no wheat, gluten free, yeast
free.
Precaution: Contains: Milk and soybeans.
4 caplets
Vitamin D (as Cholecalciferol D-3) 2,000 IU, Vitamin K-2 (as Menaquinone) 50
mcg, Calcium (as Calcium Citrate Malate) 800 mg, Magnesium (as Magnesium Oxide)
100 mg, Zinc (as Zinc Oxide) 7.5 mg, Copper (as Copper Glycinate) 1 mg,
Manganese (as Manganese Gluconate) 1 mg, MBP® 40 mg, Boron (as Hydrolyzed
Protein Chelate) 1 mg.
Other Ingredients: Cellulose, titanium dioxide (natural mineral whitener),
vegetable acetoglycerides.
APPROVED
Top
Pick
for vitamin D, calcium,
magnesium, boron & vitamin K
Dist. by Jarrow Formulas®
6 capsules
1,000 IU (25 mcg)
(D3)
✔
1,000 mg
(StimuCal™ microcrystalline hydroxyapatite)
✔
500 mg>UL
(magnesium oxide)
✔
3,000 mcg
(boron citrate)
✔
45 mcg
(MK-7 K2)
✔
Heavy metals: Pass
Take 2 capsules 3 times per
day (for a total of 6) with meals to facilitate maximum absorption, or as
directed by your qualified healthcare professional.
Large capsule
6 capsules
$0.51
[$0.20]
$20.37/240 capsules
Vitamin C 200 mg, zinc 10
mg, copper 1 mg, manganese 1 mg, potassium 99 mg
No wheat, gluten, egg, fish/shellfish, or peanuts/tree nuts.
Precaution: Contains: Soy (in trace amounts).
6 capsules
Vitamin C (as Calcium Ascorbate) 200 mg, Vitamin D3 (Cholecalciferol) 25 mcg
(1,000 IU), Vitamin K2 (as Natural MK-7 [Menaquinone-7]) 45 mcg, Calcium
(Elemental) (from StimuCal™ Microcrystalline Hydroxyapatite) 1,000 mg, Magnesium
(as Magnesium Oxide) 500 mg, Zinc (L-OptiZinc®) (as Zinc L-Methionine Sulfate)
10 mg, Copper (as Copper Gluconate) 1 mg, more...
Unless otherwise noted,
information about the products listed above is based on the samples purchased
by ConsumerLab.com (CL) for this Product Review. Manufacturers may change
ingredients and label information at any time, so be sure to check labels carefully
when evaluating the products you use or buy. If a product's ingredients differ
from what is listed above, it may not necessarily be of the same quality as
what was tested.
The information contained
in this report is based on the compilation and review of information from
product labeling and analytic testing. CL applies what it believes to be the
most appropriate testing methods and standards. The information in this report
does not reflect the opinion or recommendation of CL, its officers or employees.
CL cannot assure the accuracy of information.
Copyright
ConsumerLab.com, LLC, 2021 All rights reserved. Not to be reproduced,
excerpted, or cited in any fashion without the express written permission of
ConsumerLab.com LLC
ConsumerTips™:
What to Consider When
Buying:
Before buying a vitamin D supplement, be aware that vitamin D can be obtained
in sufficient amounts from exposure to sunlight, fortified milk (400 IU per
quart or 100 IU per cup), and other fortified foods (e.g., many breakfast
cereals and nutrition bars, some brands of orange juice, yogurt, margarine, and
soy beverages).
Fatty (oily) fish are also good sources of vitamin D. For
example, you can get significant amounts of vitamin D from a 3-ounce (85 gram)
serving of canned sockeye salmon (17.9 mcg or 716 IU), canned pink salmon (12.3
mcg or 492 IU), light tuna (e.g., skipjack or yellowtail) (5.7 mcg or 228 IU),
sardine (4.1 mcg or 164 IU). (U.S. Dietary Guidelines 2015-2020). Interestingly, canned
fish tends to provide more vitamin D than traditionally cooked fish (see
our Review of Canned Fish).
Small amounts of vitamin D are found in beef liver
(about 0.17 to 1.2 mcg per 3-ounce serving), cheese (up to 0.85 mcg per 3-ounce
serving), and egg yolks (0.7 to 1 mcg per yolk). A ½ cup of portabella
mushrooms exposed to ultraviolet light can provide 7.9 mcg or 316 IU).
Animal-based products can also provide small amounts of calcifediol, the
25-hydroxylated form of vitamin D. For instance, you can get small amounts of
calcifediol from a 3-ounce (85 gram) serving of beef liver (0.06 to 0.65 mcg),
pork liver (0.37 mcg), and chicken thigh (0.17 mcg), as well as from egg yolk
(0.09 to 0.14 mcg) and butter (about 0.1 mcg per tablespoon) (Schmid, Adv Nutr 2013).
Getting vitamin D from sunlight
UVB light from the sun, the primary wavelength of light that can cause sunburn
and contribute to sun cancer, is necessary for the synthesis of vitamin D in
the skin. However, just ten to fifteen minutes of sun exposure at least two
times per week to the face, arms, hands, or back without sunscreen is usually
sufficient to provide adequate vitamin D. It has been estimated that getting
the equivalent of a 1,000 IU dose of vitamin D requires exposing the face,
hands and arms to full sunlight at noon for 6 to 15 minutes in Miami or 9 to 19
minutes during non-winter months in Boston, based on a darker-skinned
Caucasian. Times are shorter by about 33% for people with very fair skin and
double for those with dark skin. To get only 400 IU, times would be 40% as
long.
A study in Turkey among 40 nursing home residents (average age
76), slightly less than half of whom had low blood levels of vitamin D (< 20
ng/mL), found that sunlight exposure (at 40° north latitude, similar to
Boulder, Colorado and Philadelphia) significantly increased vitamin D blood
levels — measured as 25(OH)D. Among the residents who received sun exposure
without sunscreen for about 20 minutes per day, five days per week, to
approximately 33% of the body (hand, face, neck, forearms and lower legs) for
one month during summer, levels increased from 24 ng/mL to 32 ng/mL, in
contrast to little change in residents who did not receive this sun exposure.
Participants were advised to get their sun exposure between 10:30 and 11:30 am
in order to avoid the hottest times of the day. It's worth noting that all of
the participants had light or fair skin. As noted earlier, longer sun exposure
times may be needed to raise vitamin D levels in people with darker skin (Okan, J Clin Densitom 2021).
Sun exposure cannot cause toxic levels of vitamin D because excessive exposure
to sunlight degrades previtamin D3 (which is normally converted by
sunlight into vitamin D3 in the skin) and degrades vitamin D3 itself (Holick, N Engl J Med 2007). In fact, a study in which Caucasian
subjects with more than sufficient levels of 25-hydroxyvitamin D (the form of
vitamin D commonly measured in blood tests), averaging 33 ng/mL, were exposed
to full midday sun in shorts (and, for women, sports bras) on their backs for
15 minutes and stomachs for another 15 minutes, levels of vitamin D in the
blood increased significantly, but there was no increase in levels of
25-hydroxyvitamin D, and subjects with particularly high starting levels of
vitamin D in their blood showed no increase in these levels with sun exposure.
Older people in the study produced somewhat less vitamin D than younger people
but the difference was not statistically significant (Chalcraft, Nutrients 2020).
Increased awareness about skin cancer has caused people
to avoid the sun or use sunscreen. Concern has been raised as to
whether the use of sunscreen causes a potential risk of reduced vitamin
D. One study suggested that use of a low SPF sunscreen may
provide protection from sun damage while still allowing enough UVB exposure for
the body to synthesize vitamin D, although it's important to note that the
study was funded by the makers of the sunscreen used in the study (Walgreens
Boots Alliance Inc.). The study showed that in fair-skinned adults (average age
35) with sufficient blood levels of vitamin D who were outside for
approximately 5 ½ hours per day for one week, consistent use of one of two
sunscreens each with a sun protection factor (SPF) of 15 but having either low
or high UVA protection prevented sunburn and resulted in modest average
increases in blood levels of vitamin D (5 ng/mL with the low UVA formula and 8
ng/mL with the high UVA formula). (Note: Higher UVA formulas allow more UVB light,
which, as noted above, is needed for vitamin D synthesis) (Young, Br J Dermatol 2019).
Furthermore, an observational study
among 3,418 people ages 20 and older (average age 40) found that frequent sun
protective behaviors — including wearing long sleeves, staying in the
shade, and/or using sunscreen "most of the time or always" when going
outside for more than one hour — was not associated with
reduced total, upper body, or lower body bone mineral density or increased risk
of osteoporotic bone fractures compared to rare sun protective behaviors. Blood
levels of vitamin D were not assessed in this study (although dietary intake of
vitamin D appeared to be similar across the groups), and strength, type and
amount of sunscreen used were not reported (Afarideh, JAMA Dermatol 2021).
However, a study among adults aged 20 to 49 years with moderately dark skin in
Korea who had vitamin D levels below 20 ng/mL found that 30 minutes of daylight
to the hands, arms, and legs (while protecting the face and neck) three times a
week for four weeks in the summer only raised levels by an average 0.9 ng/mL.
Another group instructed to block as much sunlight as possible (with sunscreen
and protective clothing) had an average decrease of -0.7 ng/mL, while a third
group whose members did the same but took 600 to 800 IU of vitamin D daily had
an average increase of 3.5 ng/mL. The researchers concluded that the amount of
sun exposure in the first group -- although similar to some standard
recommendations -- was inadequate for this population (Lee, J Korean Med Sci 2020).
Who is likely to get too little vitamin D?
Inadequate vitamin D intake is common in people who live in northern climates
(north of a line from Boston to the northern border of California), especially
if they are dark-skinned.
Older individuals are at increased risk of vitamin D
insufficiency (Omdahl, Am J Clin Nutr 1982; Holick, J Clin Endocrinol Metab 2005; van der Wielen RP, Lancet 1995), particularly the very
old (Passeri, J Clin Endocrinol Metab 2003). This may be due to a
variety of factors, including reduced time outdoors with reduced skin exposure
to the sun. A study showed that surgical skin samples from older people was
less able to convert a vitamin D precursor compound toward vitamin D than skin
from younger individuals and there was less of this precursor in the top
(epithelial) layer of older skin - although amounts in the lower layer were the
same (MacLaughlin J, J Clin Invest 1985). However, an experiment
in living people found that exposing the backs or entire bodies of old and
young people to equal amounts of light produced the same amounts of vitamin D (Davie, Clin Sci 1980).
People who are obese also tend to have a low plasma concentration of
25-hydroxyvitamin D, as subcutaneous fat may sequester the vitamin.
Because vitamin D is a fat-soluble vitamin, people with reduced ability to
absorb fat in the gut may also require vitamin D supplementation.
Gummies vs. tablets
To enhance its absorption, it is advisable to take
vitamin D with a meal containing fats or oils. However,
if you take it only with water, you may absorb more vitamin D from chewing a
gummy supplement than from swallowing a tablet, as demonstrated in a study
funded by the makers of VitaFusion gummies (Church &
Dwight). In the study, 31 participants who were not deficient in vitamin D
consumed a single, very high dose (20,000 IU) of vitamin D3 either as eleven
and three-quarters VitaFusion D3 gummies or four and
three-quarters vitamin D3 tablets from Nature Made) with 8 oz. of
water on an empty stomach 30 minutes before a standardized breakfast. Over a
48-hour period, average blood levels of vitamin D were found to be approximately
twice as high with the gummies than the tablets (Wagner, Nutrients 2019). Possible reasons for the better absorption
with the gummies were that only the gummies contained oils and this, plus
chewing them, better stimulated the digestive process. Had the supplements been
taken with a meal containing oils, the results for each would likely have been
more similar to each other.
Be aware that gummy vitamins are difficult to manufacture, their ingredients
can more easily degrade, and ConsumerLab's Review of Multivitamins has found gummies more likely to fail tests than tablets or
capsules for containing more or less of ingredients than listed.
Oral Sprays
Vitamin D oral sprays are commercially available (although not
legally, as sprays are not considered dietary supplements) and have been
promoted as an alternative for people with gastrointestinal issues (such as
Crohn's disease, ulcerative colitis and steatorrhea) which can reduce
intestinal absorption of vitamin D. This is based on the premise that sprayed
vitamin D can be absorbed directly through the lining of the mouth. However,
there do not appear to be studies proving that oral absorption actually occurs.
Nevertheless, sprays can certainly work as well as any other type of oral
delivery, possibly because one is still swallowing the liquid. In fact, a small
study in India in people having various bowel diseases and very low levels of
vitamin D found that 1,000 IU of vitamin D3 given as an oral spray daily for
one month significantly increased blood levels of vitamin D (by an average of
10.5 ng/mL) compared to the same dose of D3 taken as a softgel (which resulted
in an average increase of 4 ng/mL) (Satia, Nutr J 2015). In the same study, vitamin D3 spray also significantly
increased vitamin D blood levels of healthy people compared to supplementation
with the softgel — resulting in average increases of 8 ng/mL and 4 ng/mL,
respectively. However, this may not have been a fair comparison, since both the
spray and capsules were taken 30 minutes following a meal. This is
not an ideal way to take vitamin D from a pill, which should be taken with a
meal for best absorption -- and properly taking 1,000 IU of vitamin D as a
softgel daily should increase blood levels by about 10 ng/mL in a lean
individual.
A study in Ireland compared 3,000 IU of vitamin D given daily to healthy adults
as an oral spray (DLux3000 from Better You, UK, which includes
lecithin -- a fat) or as a capsule. After 4 weeks, the spray and capsule were
found to increase vitamin D levels, respectively, by 10.6 ng/mL and 12.2 ng/mL,
with the difference between the two not statistically significant. No
instruction was given to take either formulation at the time of a meal, perhaps
explaining the modest increases despite the large dose (Todd, Br J Nutr 2016). A 6-week, placebo-controlled trial in
England also found that 3,000 IU of vitamin D per day given as a spray resulted
in similar increases in blood levels of vitamin D as the same dose given as a
capsule. Average blood levels increased by about 16.3 ng/mL with both the capsules
and the spray. Two participants reported the formation of small blisters on the
cheek and tongue, one of whom discontinued the study -- although the
researchers did not specify if this occurred in those given the spray or
capsules, they did note that only 86% of the spray group was fully compliant
versus 96.4% of the capsule group. As in the study above, participants were not
instructed to take the capsules or spray with a meal. The vitamin D spray was
provided by Better You, which funded the study (Williams, Eur J Clin Nutr 2019). Sprays tend to be more
expensive: about 8 to 10 cents per 1,000 IU dose. The same dose can be obtained
from a vitamin D liquid drop or pill for little as 1 or 2 cents as shown in
this Review.
In short, in healthy individuals, non-sprays can be as effective as sprays
and are less expensive. In people with intestinal absorption problems, either
may raise vitamin D levels but absorption may be greater with a spray.
Other tips when buying:
When buying vitamin D, be aware that it is measured in International Units (IU)
of vitamin D activity or as micrograms (mcg) of cholecalciferol (D3) or ergocalciferol (D2). 10 mcg = 400 IU.
Some calcium supplements contain the trace mineral boron, typically in amounts ranging from less than 1 mg up to about 6
mg per daily serving. Some, but not all evidence suggests that boron may reduce
calcium loss in the urine, especially when magnesium intake is low (Neilson, FASEB J 1987). Although some preliminary research suggests
boron supplementation in doses of 3 mg to 10 mg per day may be helpful for
osteoarthritis and osteoporosis, one small trial found no increase in spine or
thigh bone mineral density in postmenopausal women who took 3 mg of boron daily
for one year compared to placebo (Biquet, Osteoporos Int 1996). Americans typically get an average of about
1 mg to 1.25 mg of boron daily from foods such as leafy vegetables, raisins,
prunes, non-citrus fruits like apples, and some grains (Rainey, J Am Diet Assoc 1999). There is no
established daily requirement for boron, but there is an upper tolerable intake
level of 20 mg for per day for adults. Be aware that even at doses of 3 mg to
10 mg daily, boron may increase estrogen levels in both women and men (Neilson, FASEB J 1987; Naghii, Biol Trace Elem Res 1997). This may be of
particular concern for women on hormonal therapy or those with a history of
estrogen-sensitive cancer.
A small news article appeared in 2010 regarding research on the content of
vitamin D supplements presented at a Multiple Sclerosis conference by a team at
Johns Hopkins University. The results showed the mean actual dose in 10
supplements to be only 33.5% of the labeled dose, with a range from 0.24% to
81.7%. ConsumerLab.com contacted the research team to learn more about the
findings. We spoke with Dr. Norman Haughey who oversaw the testing. It appears
that the report was preliminary: The team had not yet performed extraction
efficiency testing, i.e., making sure that they got all of the vitamin D out of
the tested samples. Poor extraction recovery will yield low results and is a
well-known problem with vitamin D in supplements where other components of the
product can interfere with measurements.
What to Consider When Using:
In November 2010, recommended intake levels of vitamin D for Americans and
Canadians were increased by the Institute of Medicine (IOM). For infants up to
12 months of age, the daily Adequate Intake (AI) was set at 400 IU (10
micrograms). Note that the AI is only relevant if an infant is not getting
adequate exposure to sunlight. The following Recommended Dietary Allowances
(RDAs) were established for other age groups: 600 IU (15 micrograms) for people
aged 1 to 70 and 800 IU (20 micrograms) for those aged 71 and older.17Confusing matters is that the FDA uses somewhat different daily
amounts to establish the "Daily Values" in the "%DV"
figures appearing in Supplement Facts panels on labels. For decades, the Daily
Value for vitamin D for adults and children ages 4 and older was set at 400 IU
(which turned out to be too low) and, in 2016, the FDA announced that the DV is now 800 IU
(which is higher than necessary for most people) but that labels are not
required to reflect this change until the beginning of 2020. So, for now, if
you see 100% as the "%DV," that means the product provides 400 IU per
serving.
While some studies suggest that even higher intakes of vitamin D may be useful
for a range of purposes, the IOM considered the data behind those suggestions
preliminary. Nevertheless, based on studies that showed a decreased risk of
cancer associated with increased vitamin D intake and/or blood levels, the
Canadian Cancer Society recommends a daily intake of 1,000 IU for adults in the
fall and winter. The Canadian recommendation reflects the fact that there is
reduced sun exposure in northern latitudes. The recommendation is for 1,000 IU
intake year-round for people who are older, have dark skin, don't go outside
often, or wear clothing that covers most of their skin.
In infants, the IOM and American Academy of Pediatrics recommend a vitamin D
target level of 20 ng/dL. Both organizations recommend 400 IU daily to achieve
this level (Wagner, Pediatrics 2008). A convenient way to
give this is to add a single 400 IU drop of a liquid vitamin D (such as Baby
Ddrops — 400 IU per drop -- as listed in the Results table above) to bottled milk per day. Supplementation
should occur even if children are breastfed -- particularly if breastfeeding
continues for more than one year: A study in Canada found that without
supplementation, the probability of breastfed children being vitamin D
deficient was 16% by age 2 and 29% by age 3 (Darmawikarta, Am J Pub Health 2016).
Some groups suggest higher levels in infants of 30-60 ng/dL, however, this is
controversial (Endo Soc, J C Endrocrinol Metab, 2011; Can Paed Soc Paediatr Child Health 2007). A clinical study shows
that 400 IU of vitamin D3 daily was adequate to achieve the target level of 20
ng/dL in 97.5% of healthy, breastfed infants after 3 months of treatment.
Higher doses were also studied (800 IU, 1200 IU, and 1600 IU daily). The 1600
IU dose caused excessively high levels in many infants. Additionally, there was
no difference in bone mineral content between the lower and higher doses after
a year of treatment (Gallo, JAMA 2013). These data confirm that 400 IU daily is an adequate dose for
most healthy infants. Higher doses should be used cautiously. See Concerns and Cautions.
For building bone in young girls (ages 9 to 13), a study found
benefit with a supplement providing, on a daily basis, 800 mg of calcium (from
calcium citrate and calcium carbonate), 400 IU of vitamin D2, and 400 mg of magnesium (from magnesium citrate) when taken
regularly for six months (Greene, Osteoporosis Int 2011). The supplement (Active
Calcium Chewable, USANA Health Sciences, Inc. - not tested in this Review)
was taken as four chewable tablets, two with breakfast and two with dinner as
it is best to divide doses when taking large amounts of minerals. Another study
found that a weekly dose of 1,400 IU or 14,000 IU of vitamin D3 resulted in significant increases in the mineral content
of hip bones -- although the majority of the girls started the study deficient
in vitamin D. Interestingly, the higher weekly dose appeared to have somewhat
less effect than the lower dose (Al-Shaar, Bone 2013).
For reducing the risk of fracture of the hip and nonvertebral bone in people 65
years of age or older, maintaining a serum vitamin D level above 24 ng/mL
appears to be beneficial.39
For reducing the risk of cardiovascular disease and stroke in men, 600 IU or
more of vitamin D per day from food and supplements may be helpful. (A similar
cardiovascular benefit in women has not been shown).21
For reducing high blood pressure in people already taking a calcium channel
blocker (nifedipine), 2,000 IU of vitamin D3 per day has been shown reduce systolic and diastolic
pressures by a few points (Chen, Atherosclerosis 2014). However, a study
giving 100,000 IU of vitamin D3 quarterly
showed no benefit (Witham, JAMA 2013) and a review of 46
studies concluded that vitamin D appears ineffective for lowering high blood
pressure (Beveridge, JAMA Int Med 2015).
For improving cholesterol levels in people already taking a statin medication,
2,000 IU of vitamin D3 per
day has been shown to be effective, particularly among people with lower blood
levels of vitamin D (Qin, Clin Nutr 2015).
For improving balance and muscle strength in older adults 800 to 1,000 IU daily
of vitamin D may be beneficial.30 (Cangussu, Osteoporos Int 2015).In older women
deficient in vitamin D, 4,000 IU daily of vitamin D3 has been shown to increase muscle fiber size, although not
physical functioning (Ceglia, J Clin Endocrin Metab 2013).
For reducing symptomatic pain in fibromyalgia, 2,400 IU of vitamin D3 for people with vitamin D levels below 24 ng/mL, and 2,400
IU for those starting with levels between 24 ng/mL and 32 ng/mL have been
successfully used (although treatment was stopped as a precaution when levels
exceeded 48 ng/mL, which occured with several patients) (Wepner, Pain 2013).
For reducing menstrual pain in women, a single high dose of 300,000 IU vitamin
D3 taken 5 days before
the start of menstruation may be beneficial for the following two months.29 However, there are potential concerns with such a high
dose (see Concerns and Cautions).
During pregnancy, raising vitamin D blood levels to 32 ng/mL in a population
with a high rate of vitamin D deficiency decreased by half the incidence of
pre-term labor, pre-eclampsia, and/or gestational diabetes. Women were given
vitamin D starting at week 20 and dosage depended on initial vitamin D status,
ranging from one dose of 60,000 IU to monthly doses of 120,000 IU for two to
four months (Sablok, Clin Endocrinol 2015).
For reducing the risk of exacerbations of COPD, 100,000 IU of vitamin D monthly
or 120,000 IU every two months has been helpful among people deficient in
vitamin D (Martineau, Lancet Resp Med 2014; Lehouck, Ann Intern Med 2012).
D2 or D3?
Vitamin D can be found in dietary supplements in the D2 or D3 form.
A number of studies have compared the abilities of vitamin D2 and vitamin D3 to
raise vitamin D blood levels. Some have found them equally effective, and some
have found D3 more
effective (Armas, J Clin Endocrinol Metab 2004; Trang, Am J Clin Nutr 1998; Holick, J Clin Endocrinol Metab 2008; Biancuzzo, Am J Clin Nutr 2010). As either form can be
obtained inexpensively, it seems prudent to use supplements containing the D3 form, particularly as D2 may cause erroneously low vitamin D blood test results. The potential advantage
of D3 was illustrated in
a small, but well-controlled, study in New Zealand in which 1,000 IU of vitamin
D2 or D3, or a placebo, was given to healthy, non-obese individuals
(ages 18 to 50) from the end of summer to the end of winter (Logan, Br J Nutr 2013). On average, vitamin D levels dropped 18
ng/mL among those taking placebo and 8 ng/mL among those taking vitamin D2, while those taking D3 maintained their levels (at 32 ng/mL). It's worth noting
that, unlike the U.S., there is little vitamin D fortification of milk or other
foods in New Zealand. Also, due to the relatively high latitude of the study
region (46° — similar, for example, to Portland, Oregon) sunlight was
relatively limited during the period of the study. Consequently, the dose of
vitamin D3 given
may have been greater than needed to maintain vitamin D levels in similar
individuals in much of the U.S. A large study among
women in England, which used a lower dose — 600 IU per day, also demonstrated
vitamin D3 to
be superior to D2. In
this study, which occurred during winter months, 12 weeks of supplementation
with D3 raised
blood levels by 73% compared to only 34% for vitamin D2. The researchers speculated that the greater effect of D3 may be due to 1) a possible shorter half-life in the body
of D2 than D3, and 2) the fact that each form has been shown to reduce levels
of the active 25(OH)D form of the other but, since only D3 is naturally found in the body, D2 may have more of a negative effect on total blood levels (Tripkovic, Am J Clin Nutr 2017).
D3 or Calcifediol?
Vitamin D3 may
be the preferred supplement form of vitamin D for raising 25(OH)D levels
compared to vitamin D2, but
calcifediol, a 25-hydroxylated form of vitamin D, may be even more effective
than vitamin D3. Most
research shows that calcifediol is about three to five times more potent for
increasing 25(OH)D levels than vitamin D3 when taken by mouth. The rate of absorption of calcifediol
has also been shown to be higher than that of vitamin D3. While 25(OH)D levels increase by about 0.7 to 1 ng/mL for
every 100 IU of vitamin D3 taken when
vitamin D levels are low, the rate of absorption decreases as 25(OH)D
levels rise. On the other hand, the absorption of calcifediol is linear,
meaning that the rate of absorption does not decline as blood levels of 25(OH)D
increase (Cesareo, Nutrients 2019). Unlike vitamin D3, however, calcifediol is available only as a prescription drug
in the U.S. and not as a supplement. Similarly, calcitriol, the active
hormone form of vitamin D formed in the body from calcifediol, is also
available only as a prescription drug in the U.S. However, animal-based foods may contain calcifediol, as it is found in animal muscle
and adipose (fat) tissue (Taylor, J Nutr 2014).
How Much Do You Need and "How Much is Too
Much?"
After being ingested, both vitamin D2 and D3 are
metabolized in the liver to form 25-hydroxy vitamin D and in the kidneys to
1,25-hydroxy vitamin D. Total serum levels (sometimes referred to as
"blood levels") of 25-hydroxyvitamin D (also referred to as 25-(OH)D)
are commonly used clinically to evaluate vitamin D status.
Based on the latest recommendations of the Institute of Medicine (IOM), the
Estimated Average Requirement (EAR) for vitamin D among individuals ages 1 to
70 for bone growth and maintenance is daily intake of 400 IU of vitamin D,
assuming minimal to no sun exposure, corresponding to a blood level of vitamin
D (known as serum 25-(OH)D levels) of just 16 ng/mL. Some people will need more
than this "average" requirement" so the IOM calculated an amount
which would satisfy the requirements of practically all (97.5%) individuals;
this amount, the Recommended Daily Allowance (RDA), is 600 IU of
vitamin D, corresponding to a vitamin D blood level of 20 ng/mL. [Another
way of expressing these levels is in nanomoles per liter (the unit of
measurement commonly used in Canada): 1 ng/mL = 2.5 nmol/L, so 20 ng/mL = 50
nmol/L and 30 ng/mL = 75 nmol/L]. For individuals over age 70, the RDA
is 800 IU.
In people deficient in vitamin D, long-term
effects are bone softening, known as osteomalacia in adults and rickets in
children -- who can also suffer bone deformities. Other symptoms can be vague
but can include bone pain and muscle weakness, joint pain
(particularly of the wrists, ankles, shoulders, and shins), chronic tension headaches, depression, insomnia
and hair loss (Khan, J Oncol Pract 2010). In infants, a common early symptom of
deficiency can be excessive sweating (Hossein-nezhad, Mayo Clin Proc 2013).
From reviewing national surveys of blood levels, the IOM concluded that the
majority of Americans and Canadians are getting enough vitamin D (as well as
calcium), although elderly individuals are more likely to fall short on both
and some adolescent girls may not get quite enough calcium. The IOM has
determined that just 6% of U.S. population is vitamin D deficient (≤ 12.5
ng/mL), and 13% of Americans between the ages of 1 and 70 are "at
risk" for vitamin D inadequacy (Manson, N Engl J Med 2016).
The IOM has cautioned that vitamin D blood levels
≥ 50 ng/mL (and daily intakes above 4,000 IU) can put people at risk for
adverse effects. This is based on studies showing an increase in
adverse events (including overall mortality, some cancers, cardiovascular
disease, and fractures and falls) associated with serum 25-(OH)D levels
starting at about 30 ng/mL to 48 ng/mL and higher (75 to 120 nmol/L). Examples
of such adverse events include the following:
·
A population study following nearly a quarter million people in
Denmark for three years found that vitamin D levels of 20 to 24 ng/mL were
associated with the lowest risk of dying during the study.35 A high serum level (56 ng/mL) was associated with a
42% higher risk of dying during the study than people with a
level of 20 ng/mL.
·
An analysis of the vitamin D levels of more than 14,000
Americans aged 17 years and older found that mortality rates fell with
increasing vitamin D levels until reaching 39 ng/mL (Kramer, PLoS One 2012). The lowest mortality
rate was among those in the 30 to <40 ng/mL group, however, mortality rates
were similar across the range of 20 to 40 ng/mL.
·
A population study following nearly half a million people aged
45 years and older for 4.5 years in Israel found that people with vitamin D
levels of 20 to 36 ng/mL had the lowest risk of heart attack or death. Compared
to people in this range, risk of heart attack and death was 91% higher among
those with levels below 10 ng/mL, 26% higher among those with levels 10 to 20
ng/mL, and 13% higher when levels were above 36 ng/mL (Dror, J Clin Endocrinol Metab 2013).
·
A study comparing low-dose to high-dose vitamin D3, found that
those achieving the highest blood levels fell about twice as often as those
just above sufficiency (Bischoff-Ferrari, 2016).
·
A study in Canada comparing the effects of different doses of
vitamin D given daily for 3 years to adults with osteoporosis found that,
compared to a dose of 400 IU per day, 4,000 IU and 10,000 IU reduced bone
mineral density (BMD) in lower leg, and 10,000 IU also reduced BMD
in the forearm. There were no significant differences bone strength for the
different doses (Burt, JAMA 2019). A follow-up
analysis showed that loss of BMD was greater in women than in
men. After 3 years of treatment with 4,000 IU or 10,000 IU of vitamin D, BMD
decreased in the forearms of women by 3.8% and 5.5%, respectively, compared to
a nonsignificant reduction of 1.3% and 1.9%, respectively, in men. Small losses
of BMD also occurred with 400 IU of vitamin D for men and women, but the rate
of bone loss in these groups was similar to what would be expected to occur
with normal aging. A similar, although smaller, loss of BMD in the lower leg
also occurred in women taking higher doses of vitamin D but not in men. The
average blood level of 25(OH)D after 3 years of treatment with 4,000 IU and
10,000 IU of vitamin D was 53 and 58 ng/mL, respectively, which are both above
the vitamin D blood levels that the IOM has warned can put people at risk for
adverse effects (Burt, J Bone Miner Res 2020).
·
An analysis of data from the National Health and Nutrition
Examination Survey (NHANES) found a 35% increase in the risk of cancer-related
death and a 111% increase in all-cause death among people who already had
sufficient blood levels of vitamin D (≥20 ng/mL) but were supplementing
with more than 10 mcg (400 IU) of vitamin D per day (Chen, Ann Intern Med 2019). (See more about this study in the CL Answer
about getting vitamin and mineral from foods vs.
supplements).
A
possible explanation for why taking high-dose vitamin D has been linked with
muscle weakness and increased risk of fractures and falls, comes from a study
among professional athletes in Europe which found that a dose of 70,000 IU
vitamin D3 taken
weekly for three months increased the production of an enzyme (24-hydroxylase)
which breaks down vitamin D in the blood and inactivates the
hormonally active form of vitamin D in the body. The increase in this enzyme
persisted for up to 6 weeks after supplementation was discontinued (Owens, Med Sci Sports Exerc 2017). The researchers
recommended that "lower doses of vitamin D3 ingested frequently may be
most appropriate and gradual withdrawal from supplementation as opposed to
rapid withdrawal may be favorable."
Giving an extremely high single dose (540,000 IU) of vitamin D
orally to critically ill people deficient in vitamin D (averaging about 11
ng/mL) upon admission to intensive care units was not shown to
reduce the risk of death in a large U.S. study involving over one thousand
patients. In fact, within 28 days, 17.3% of those given vitamin D had died
versus 13.1% of those given placebo. At 90 days, the values were, respectively,
23.5% and 20.6%. Deaths were particularly high with vitamin D versus placebo
for those admitted with infections (28.4% vs. 19.9%) or sepsis (33.7% vs.
21.3%). Falls were also more frequent (7.1% vs. 5.3%). Due to the findings, the
study was stopped before enrolling its target of 3,000 patients. Among those
given vitamin D, levels rose to an average 46.9 ng/mL within three days (Nat Heart Lung Blood Inst, New Eng J Med 2019).
An Australian study among 22 men and women (ages 50 to 75),
about two-thirds of whom had low (< 20 ng/mL) or deficient levels of vitamin
D, found that adding a one-time 50,000 IU dose at the beginning of daily 1,000
IU dosing, did not raise vitamin D levels more than daily 1,000 IU alone over
six weeks. For those who started the study with sufficient levels, the 50,000
IU dose appeared to hamper vitamin D increases during the
final three weeks of the study. Both treatments equally increased circulating
osteoprogenitor cells, which are involved in the formation of bone (Feehan, Exp Gerontol 2021).
High doses of vitamin D do not appear to promote or
protect against the development or progression of peripheral arterial
calcification (hardening of the arteries), according to a 3-year study that
compared the effects of taking 4,000 IU or 10,000 IU of vitamin D to taking
just 400 IU among 302 adults in Canada who were generally vitamin D sufficient
(average starting vitamin D blood level of 31.6 ng/mL) (Billington, Osteopor Int 2020).
The idea has been suggested that adverse effects of very high doses of vitamin
D could be eliminated by also administering high doses of vitamins A and K (Masterjohn, Med Hypotheses 2007). This has not been
proven and remains only a hypothesis.
It would seem prudent, based on the latest IOM
recommendations and recent studies, to maintain blood levels of vitamin D above
20 ng/mL, but not much higher than 30 ng/mL. Misinterpretation and
misapplication of the IOM reference standards can have adverse implications for
patient care, including unnecessary vitamin D screening and supplementation.
For healthy patients, routine screening is not recommended (Manson, N Engl J Med 2016).
With regard to the combination of vitamin D and calcium, an analysis of
clinical trials involving older adults found a 9% lower risk of dying over a
3-year period among those who took vitamin D along with calcium supplementation
(1,000 mg) compared to those not taking these supplements.35 The benefit was only found with low dose (400 IU) and not
higher dose (800 IU or more) vitamin D, and only with daily dosing as opposed
to intermittent (e.g., annual) dosing of vitamin D. The benefit was not seen
among people taking vitamin D without calcium, although this does not suggest a
protective effect of calcium. It is difficult to draw useful conclusions for
individuals from this study particularly because blood levels of vitamin D were
not part of the analysis, i.e., it is possible that results would vary
depending one's vitamin D status.
From reviewing national surveys of blood levels, the IOM concluded that the
majority of Americans and Canadians are getting enough vitamin D (as well as
calcium), although elderly individuals are more likely to fall short on both
and some adolescent girls may not get quite enough calcium.
It should be noted that some researchers have set higher benchmarks for vitamin
D sufficiency typically 30 ng/mL or above. For example, using 30 ng/mL as the
benchmark for sufficiency and less than 15 ng/mL to define deficiency, a study
of vitamin D levels concluded that 61% of American children and adolescents had
insufficient levels of vitamin D and an additional 9% were deficient. Deficient
children tended to have higher blood pressure and lower levels of HDL
("good") cholesterol than other children. Older children were more
likely to be deficient, as were those who were obese, drank milk less than once
a week, or spent more than four hours a day with TV, video, or computers. Those
who used vitamin D supplementation were less likely to be deficient (Kumar, Pediatrics 2009).
When laboratories report your vitamin D level,
they will typically show a "standard range" or "reference
range" of about 20 ng/mL to 100 ng/mL. These ranges vary with the
laboratory and are based on levels the lab has found in 95% of a
"healthy" population. However, these numbers do not reflect
the range which has been recommended by the Institute of Medicine, as
described above, which falls at the lower end of this range. If your level is
25 ng/mL, for example, you should not interpret the results as suggesting that
your level is low. Similarly, if your level is 60 ng/mL, this does not mean
your level is ideal -- current evidence, as noted in the Review, suggests that
it is too high.
A rule of thumb for raising serum levels of
25-hydroxyvitamin D is that about 100 IU of vitamin D2 or D3 daily will raise serum levels by about 1 ng/mL in adults and adolescents. However, more vitamin D is
required by obese individuals to get this same increase: A study of obese
adolescents found that about 200 IU was needed to for every 1 ng/mL increase in
serum levels (Belenchia, FASEB J, 2011). Keep in mind, however, that there is
diminishing benefit with doses of vitamin D above 1,400 IU (Cashman, Nutrients 2017). For example, at a daily dose of 600
IU, each 100 IU was found to increase blood levels by 1 ng/mL, but, at a daily
dose of 3,750 IU, each 100 IU increased levels by only 0.41 ng/mL, according to
a study of overweight/obese older adults in Lebanon (Bacha, J Clin Endocrinol Metab 2021).
Be aware that people who
begin supplementation with lower blood levels of 25-hydroxyvitamin D (< 20
ng/mL) may achieve approximately 60% greater increases in levels than
those who already have sufficient levels (> 20 ng/mL) when taking the same
daily dose. This was shown in a 2-year study in people with type 2 diabetes
taking a daily dose of 2,000 IU vitamin D3: Levels increased by 12 ng/mL when
starting with a sufficient level, but by 19 ng/mL when starting with an
insufficient level (Best, J Clin Endocrinol Metab 2021).
With moderate (1,000 IU per day) supplementation, it has been shown to take
about 6 weeks for serum levels to reach their peak. For example, during winter
with no significant sun exposure, supplementation with 1,000 IU has been shown
to increase levels of around 20 ng/mL up to about 30 ng/ml at 6 weeks. In such
a scenario, sun exposure or a dosage higher than 1,000 IU would be necessary to
further elevate levels above 30 ng/mL (Kumar, Pediatrics 2009).
Magnesium affects vitamin D levels — make sure you get
enough
Getting an adequate intake of magnesium helps maintain optimal blood levels of
the prehormone form of vitamin D, 25(OH)D -- the form typically measured in
blood tests. When 25(OH)D blood levels are around 30 ng/mL, magnesium boosts
the conversion of vitamin D to 25(OH)D, raising levels by an average of 3
ng/mL. When levels are higher (about 30 to 50 ng/mL), magnesium actually lowers
the amount of 25(OH)D by an average of about 7 ng/mL.
A study in Spain investigated the effects of magnesium
supplementation (500 mg daily for two months) in postmenopausal women, many of
whom had low dietary intakes of magnesium and and/or low blood or erythrocyte
levels of magnesium, and most of whom had insufficient blood levels of
25-hydroxyvitamin D (< 20 ng/mL). At the end of the study, the women who
supplemented with magnesium had significantly increased vitamin D levels
(average increase 3 ng/mL) compared to those who took a placebo (Vázquez-Lorente, Nutrients 2020).
(Interestingly, with vitamin D2, a form not naturally made in the body,
magnesium keeps boosting levels of the prehormone form, regardless of the
level.) This was demonstrated in a study of 180 adults in the U.S. (Dai, Am J Clin Nutr 2018).
To keep your vitamin D blood level in an optimal range, be sure you're getting an adequate amount of magnesium — many
people don't. An additional 200
mg or so of magnesium will safely bring most people up to an adequate daily
intake. You can get this from supplements or magnesium-rich foods, as discussed
in our Magnesium Supplements Review.
In people who are Black, the traditional measurement of
vitamin D levels using total serum 25-hydroxyvitamin D may not
be appropriate as it may overestimate vitamin D deficiency. Due to a genetic
variant, many Blacks have lower levels of binding protein for vitamin D (which
binds 85 to 90% of total vitamin D), allowing more of the total vitamin D to be
bioavailable, i.e., available for use. Consequently, although total vitamin D
levels may seem low in Blacks, the bioavailable amount of vitamin D may be
sufficient. In fact, a study in Baltimore found mean total vitamin D levels to
be 15.6 ng/mL in Blacks and 25.8 ng/mL in whites, while amounts of bioavailable
vitamin D were the same in both groups. Furthermore, bone mineral density and
calcium levels were higher among the Blacks than whites (Powe, NEJM 2013). The measurement of bioavailable vitamin D may,
therefore, be more accurate for assessing the vitamin D status of Black
individuals. Unfortunately, this is more difficult than measuring
total vitamin D and currently relies on an indirect method in which vitamin
D-binding protein must be measured and the amount of vitamin D bound to the
protein is subtracted from total vitamin D.
Vitamin D Tests — Not Always Reliable
Tests to determine vitamin D levels may not always be reliable. Thousands of
vitamin D readings taken in 2007 and 2008 turned out to be
too high because the test was not properly performed. Newer, faster, and less
expensive immunoassay tests are now widely used. However, a preliminary study
found these devices to yield inaccurate results at least 40% of the time —
tending to provide low results.38 In
the study, blood samples were run with an older established method (LC/MS) and
two newer devices. The established method found vitamin D deficiency (less than
20 ng/mL) in 20% of the samples, but the Abbot Architect and Siemens Centaur-2
immunoassay devices respectively found deficiency in 28% and 44% of the
samples, classifying some people as deficient who were not. The inaccuracies
tended to occur with samples containing vitamin D2. If your test results don't
seem to jive with your vitamin D intake and level of sun exposure, consider a
retest using the LC/MS method, particularly if you are getting vitamin D2 from
supplements or foods.
Take Vitamin D with Food
It is not uncommon for a person being treated for vitamin D deficiency to fail
to achieve adequate serum levels. A small but striking study at the Cleveland
Clinic Foundation Bone Clinic suggests that one reason may be that such people
are taking vitamin D supplements on an empty stomach or with a small meal,
usually breakfast or lunch.25 In
the study, 17 such people were instructed, instead, to take the same supplement
with the largest meal of the day, usually supper. After 2 to 3 months,
researchers found that serum vitamin D levels had increased, on average, by
56.7%. This magnitude of increase was seen across a wide range of vitamin D
dosage and forms (D2 and
D3). As vitamin D is fat
soluble, it is generally recommended that it be taken with a meal containing
fats. However, based on this study, it may be best to take vitamin D with
your largest meal of the day, which is likely to contain the
most fat. A more recent study re-emphasized this point.
In this 1-day study, 50,000 IU of vitamin D3 was given with a breakfast that
was fat-free or which included fats. Mean peak vitamin D blood levels (12 hours
after taking the supplement) were 32% greater in subjects who took the
supplement with a fat-containing meal than in those who took it with the
fat-free meal. The ratio of monounsaturated to polyunsaturated fats in the meal
did not matter (Dawson-Hughes, J Acad Nutri and Dietetics 2014). The researchers
postulate that the presence of fat favors vitamin D absorption by stimulating
the secretion of bile which promotes fat absorption.
Storage
After opening a bottle of a vitamin D supplement, exposing the contents to air,
vitamin D will begin to lose activity over time. How fast this happens is
largely a function of the temperature at which the open bottle
is stored, but can also be affected by exposure to light (which is why dark or
opaque bottles are preferable) and the formulation of the product. At 77° F
(25° C), this loss has been shown to range from just 5% to as much as 40% over
a year. Refrigeration is typically not necessary unless you cannot keep the
product at room temperature or you don't expect to fully use the contents by
the "Best By" or expiration date. In these circumstances, consider
refrigerating the product, as this may significantly slow the loss of potency (Temova, Eur J Hosp Pharm 2017).
Concerns
and Cautions:
Excessive intake of vitamin D as a supplement
can result in hypercalcemia (too much calcium in the blood)
with symptoms including constipation, headache, irritability, confusion,
weakness, metallic taste, loss of appetite, painful calcium deposits and kidney
failure (Bohon, Clin Med Insights Womens Health 2013). Although this is
unlikely to occur when daily intake is under 10,000 IU, to avoid hypercalcemia
and other potential problems associated with higher blood levels of vitamin D,
keep total intake of vitamin D from supplements and food under the established
Upper Tolerable Intake Level (UL) above which the risk of harm increases. The
ULs are 1,000 IU for infants up to 6 months, 1,500 IU for infants 6 months to
12 months, 2,500 IU for children 1 to 3 years, 3,000 for children 4 to 8 years,
and 4,000 IU for all other people.17 Note:
It is not thought to be necessary to factor in the amount of vitamin D produced
by sun exposure when adding up total vitamin D intake. 4,000 IU daily, given
for 6 months to obese adolescents who were deficient in vitamin D, was found to
be safe (no hypercalcemia) as well as effective at raising vitamin D to
sufficient levels (Belenchia, FASEB J 2011).
A large study in Minnesota found that, due to increased
use of vitamin D supplements, the percentage of people with vitamin D blood
levels above 50 ng/mL increased 26-fold from 2002 to 2011, rising from 9 to 233
cases per 100,000 person-years; although hypercalcemia was rare among this
group (0.2%), occurring only among those taking 50,000 IU weekly or more often.
However, as noted in the study, levels above 50 ng/mL have not been found to be
beneficial and pose potential long-term risks (Dudenkov, Mayo Clinic Proc 2015).
Isolated cases of hypercalcemia have been reported from the use
of supplements. A 54-year-old man developed kidney failure due to untreated
hypercalcemia caused by excessive vitamin D supplementation. For 2.5 years he
been taking 8 to 12 drops daily of vitamin D that contained 1,000 IU per drop
(i.e., 8,000 to 12,000 IU per day) which he mistakenly thought contained 500 IU
per drop. In addition to discontinuing vitamin D, hydroxychloroquine was used
reduce his calcium level, but he was left with stage 3B chronic kidney disease
(Auguste, CMAJ 2019). A 50-year-old woman in England developed hypercalcemia
and acute kidney injury, with symptoms including lethargy, nausea, vomiting,
headache and high blood pressure after taking 8,000 to 16,000 IU of vitamin D
daily from a supplement for four months. Her blood levels of vitamin D had
reached 1,800 ng/mL at the time of her admission to the hospital. She reported
that she first began feeling lethargic about two months after starting
supplementation (Ferreira, Med Clin Res 2019). A famous
case, reported in 2010, involved Gary Null, a
nutrition promoter, who was apparently sickened by his own product, Gary
Null's Ultimate Power Meal, due to a manufacturing error that resulted in
2,000,000 IU of vitamin D per serving instead of 2,000 IU. A 22-year-old male
was sickened in Australia after three months use of a protein supplement for
bodybuilding. He complained of lethargy, nausea, vomiting, and had excessive
thirst and urination. His blood serum level of vitamin D blood was 145 ng/mL
(several times normal) and calcium was 13.2 mg/dL (about 40% above normal). The
powder claimed to provide 400 IU of vitamin D and 1,200 mg of calcium per
serving — although it is not known if he used more than suggested or if the
product contained higher levels than claimed. Corticosteroids were used to
lower calcium levels (Van, Am J Sci 2017). A 64-year-old woman in Brazil complained of stabbing
abdominal pain and vomiting after meals — symptoms she had suffered for several
months along with the onset of lower limb pain, headaches, fatigue, reduced
appetite, large weight loss, and frequent, foamy nighttime urination. Blood
tests showed hypercalcemia and she was hospitalized. It was found that she had
an extremely high vitamin D blood level of 374 ng/dL, which had caused
hypercalcemia and, apparently, kidney injury. She noted that she had been
taking daily vitamin complexes containing vitamin D3 (product not identified)
from a relative for about 6 months. After 7 weeks of hospitalization, during
which supplementation was stopped and hypercalcemia treated, she was discharged
with chronic kidney disease (de Paula, BMC Geriatrics 2020 with correspondence
with ConsumerLab).
Women taking a daily calcium (1,000 mg) and vitamin D (400
IU) supplement showed a 17% greater incidence of kidney stones compared
to women who did not receive the supplement.22 The increased risk, however, is small, as only 0.35% of
the women taking the calcium and vitamin D supplement reported kidney stones,
compared to 0.30% of the women in the control group. A similar (17% to 20%)
increase in kidney stones has been reported in studies with calcium
supplementation alone, suggesting that calcium, rather than vitamin D, is the
causative factor (Wallace, Am J Clin Nutr 2011). However, there is
evidence that very high-dose vitamin D can markedly increase
levels of calcium in the urine (hypercalciuria) from calcium supplementation,
which, in turn, can increase the risk of kidney stones. A study of
postmenopausal women who took either 600 IU or 10,000 IU of vitamin D3 daily along with a calcium supplement (1,200 mg of calcium
carbonate per day) for one year found that those who took the higher dose of
vitamin D drove their vitamin D levels to an abnormally high average of 86
ng/mL and had 3.6 times the risk of developing hypercalciuria
(Aloia, Clin Endocrinol (Oxf) 2018).
Giving high-dose vitamin D (96,000 to 120,000 IU) every two months has been
shown to increase the risk of upper respiratory infections,
compared to taking a low dose (400 IU) daily (Martineau, Thorax 2015)
High-dose vitamin D may decrease the natural production
of melatonin (a mediator of sleep). A small, but
well-controlled study in people with multiple sclerosis being treated with
interferon found that, after 3 months, those also given high dose vitamin D3
(800 IU daily plus 75,000 IU every 3 weeks — averaging 4,370 IU per day) had a significant
decrease in nighttime melatonin production, while those given a low dose (800
IU daily) did not. The study continued for full year during which vitamin D
levels in the both groups fell (possibly due to shorter days of winter), and,
melatonin product began to increase toward original levels (Golan, Brain, Behav, Immun 2013). Consistent with this, a
study found that among overweight, postmenopausal women given 2,000 IU of vitamin
D daily for 12 months, those whose vitamin D blood levels rose to over 32 ng/mL
showed a modest deterioration of sleep quality (6.2%
reduction) compared to those with blood levels that remained below 32 ng/mL
(5.7% improvement). The deterioration in sleep quality -- as well an increased
need for sleep medication -- was also associated with larger increases in
vitamin D blood levels. Most women started study with vitamin D levels ranging
from about 16 to 27 ng/mL and all participated in a weight loss/exercise
program as part of the study (Mason, Preventive Medicine, 2016).
The FDA has cautioned that some liquid vitamin D supplements are sold with
droppers that could allow for excessive dosing of vitamin D to infants.
It recommends that droppers hold no more than 400 IU of vitamin D to avoid this
problem.
It is particularly important to avoid excessive vitamin D during pregnancy,
as hypercalcemia in a mother can lead to seizures, mental and/or physical
retardation, and other problems in an infant.
Giving high-dose vitamin D to people who are not vitamin D
deficient may slightly increase cholesterol levels. A
placebo-controlled study in Austria among older, generally overweight adults
with hypertension but with vitamin D blood levels averaging 23.5 ng/mL found
that giving 2,800 IU of vitamin D daily for 8 weeks resulted in slight but
statistically significant increases in total cholesterol (+3.6
mg/dL) and triglycerides (+13 mg/dL) levels. (The average vitamin D level among
those receiving vitamin D rose to 30.6 ng/mL.) The researchers speculated that
high-dose vitamin D may cause increased calcium absorption from the gut,
leaving less calcium to bind to (and remove) fats passing through the gut (Schwetz, J Clin Lipidol 2018). Similarly,
increased triglyceride levels (+ 11 mg/dL) occurred in another study when
participants with low blood levels of vitamin D (average 15 ng/mL) took 4,000
IU of vitamin D3 daily for six months, while those who took a lower dose (400
IU) actually had a slight decrease in triglycerides (- 6.2 mg/dL). There were
no significant changes in total or LDL cholesterol with either dose. After six
months, blood levels of vitamin D 25(OH)D among those taking the higher and
lower dose had increased to an average of 30 ng/mL and 20 ng/mL, respectively (Miao, J Am Heart Assoc 2021).
Taking elexacaftor/tezacaftor/ivacaftor
(Trikafta), a prescription medication for cystic fibrosis, along
with vitamin D may modestly increase the absorption of vitamin D, necessitating
downward adjustment of vitamin D dosage. An analysis of data among 67 cystic
fibrosis patients with pancreatic insufficiency (which impairs absorption of
fat-soluble vitamins such as vitamin D) who were supplemented with very large
doses of vitamin D (about 1,570 mcg or 63,000 IU per week, which is
approximately 224 mcg or 9,000 IU per day) showed that, at 12 months after
being prescribed treatment with elexacaftor/tezacaftor/ivacafter (Trikafta),
vitamin D blood levels increased by about 5 ng/mL, requiring 28% of the
patients to lower their maintenance dose of vitamin. This effect was attributed
to the ability of Trikafta to improve pancreatic function,
resulting in improved absorption of vitamin D (Wright, Pediatr Pulmonol 2021).
High-dose estrogen-containing oral contraceptives (e.g.,
30 mcg ethinyl estradiol plus 150 mcg levonorgestrel) may cause an increase in
vitamin D binding protein, which regulates circulating levels of vitamin D.
However, this does not seem to significantly affect total (bound and unbound)
amounts of vitamin D in the blood, which is what most labs measure, and it is
not clear if this effect has any clinical significance. Low-dose
estrogen-containing oral contraceptives do not seem to have this effect (Stanczyk, J Steroid Biochem Mol
Biol 2021).
For more information see the government report on vitamin D at http://ods.od.nih.gov/factsheets/vitamind.asp.
References:
1 Fiscella, et al,
Vitamin D, Race, and Cardiovascular Mortality: Findings From a National US
Sample, Annals of Family Medicine, 2010;
8:11-18.
2 Armas, et al,
Vitamin D2 is Much Less
Effective than Vitamin D3 in Humans, The Journal of Clinical
Endocrinology & Metabolism, 2004; 89(1):5387-5391.
3 Trang, et al,
Evidence that vitamin D3 increases serum
25-hydroxyvitamin-D more efficiently than does vitamin D2, American Journal of Clinical Nutrition,
1998; 68:854-8.
4 Kumar, et al,
Prevalence and Associations of 25-Hydroxyvitamin D Deficiency in US Children:
NHANES 2001-2004, Pediatrics, 2009; 124(3):362-370.
5 Holick, et al,
Vitamin D2 is as Effective as Vitamin D3 in Maintaining Circulating
Concentrations of 25-Hydroxyvitamin D, J Clin Endocrinol Metab, March 2008, 93(3):677-681.
6 Hollis, B. W.,
Circulating 25-Hydroxyvitamin D Levels Indicative of Vitamin D Sufficiency:
Implications for Establishing a New Effective Dietary Intake Recommendation for
Vitamin D, J. Nutri. 135:317-322, February 2005.
7 Biancuzzo, et al,
Fortification of orange juice with vitamin D2 or vitamin D3 is as effective as
an oral supplement in maintaining vitamin D status in adults, Am J Clin Nutr, April 28, 2010 (Epub
ahead of print].
8 Vitamin D Consumer
Fact Sheet, Office of Dietary Supplements, National Institutes of
Health, Updated: 3/5/2010.
9 Milaneschi, et al,
Serum 25-Hydroxyvitamin D and Depressive Symptoms in Older Women and Men, J. Clin Endocrinol Metab, May, 5 2010 [Epub
ahead of print].
10 Sanders, et al,
Annual High-Dose Oral Vitamin D and Falls and Fractures in Older Women, JAMA. 2010;303(18):1815-1822.
11 Dawson-Hughes, et
al, High-Dose Vitamin D Supplementation: Too Much of a Good Thing? JAMA. 2010;303(18):1861-1862.
12 Terushkin, et al,
Estimated equivalency of vitamin D production from natural sun exposure versus
oral vitamin D supplementation across seasons at two US latitudes, J. Am Acad Dermatol 2010; 62(10), 929.e1-929.e9.
13 Llewellyn, et al,
Vitamin D and Risk of Cognitive Decline in Elderly Persons, Arch Intern Med, July 12, 2010;
170(13):1135-1141.
14 Knekt, et al, Serum
Vitamin D and the Risk of Parkinson Disease, Arch Neurol, July 2010; 67(7): 808-811.
15 Urashima, et al,
Randomized Trial of Vitamin D Supplementation to Prevent Seasonal Influenza A
in Schoolchildren, Am J Clin Nutr 2010; 91(5):1255-60.
16 Sandu, et al, The
Role of Vitamin D in Asthma, Ann Allergy Asthma Immunol 2010; 105(3):191-199.
17 Dietary Reference
Intakes for Calcium and Vitamin D (2010), Food and Nutrition Board, National
Acadamies Press.
18 Ensrud, et al,
Circulating 25-Hydroxyvitamin D Levels and Frailty Status in Older Women, J. Clin Endocrinol Metab, 2010 95: 5266-5273.
19 Sharief, at al,
Vitamin D levels and food and environmental allergies in the United States:
Results from the National Health and Nutrition Examination Survey 2005 -
2006, J. Allergy Clin Immunol, 2011
Published online February 17, 2011.
20 Green, et al,
Calcium and vitamin-D supplementation on bone structural properties in
peripubertal female identical twins: a randomised controlled trial, Osteoporosis Int 2011; 22(2):489-981.
21 Sun et al, Vitamin
D intake and risk of cardiovascular disease in US men and women, Am J Clin Nutr. 2011 June 8 [Epub ahead of print].
22 Wallace, et al,
Urinary tract stone occurrence in the Women's Health Initiative (WHI)
randomized clinical trial of calcium and vitamin D supplements, Am J Clin Nutr 2011; 94: 5-6.
23 Mitri, et al,
Vitamin D and type 2 diabetes: a systematic review, Eur J Clin Nutr, 2011, 1-11.
24 Bertone-Johnson, et
al, Vitamin D intake from foods and supplements and depressive symptoms in a
diverse population of older women, Am J Clin Nutr 2011 August 24 [Epub
ahead of print].
25 Mulligan, Taking
vitamin D with the largest meal improves absorption and results in higher serum
levels of 25-hydroxyvitamin D, J Bone and Min Res 2010; 25(4):
928-930.
26 Belenchia, et al,
Safety and efficacy of using high-dose (4,000 IU) vitamin D supplementation to
improve the vitamin D status of obese adolescents, The FASEB Journal. 2011;
25:343.4., The FASEB Journal. 2011; 25:343.4
27 Wolpin, et al,
Plasma 25-Hydroxyvitamin D and Risk of Pancreatic Cancer, Cancer Epidemiol Biomarkers Prev. 2011 Dec.7 [Epub ahead
of print]
28 Amer, et al,
Relation between serum 25-vitamin D and C-reactive protein in asymptomatic
adults (from the continuous national health and nutrition examination survey
2001 to 2006), Am J Cardiol 2012 Jan.15 [Epub ahead of print], Am J Cardiol 2012 Jan.15[Epub ahead of print]
29 Lasco, et al
(2012). Improvement of Primary Dysmenorrhea Caused by a Single Oral Dose of
Vitamin D: Results of a Randomized, Double-blind, Placebo-Controlled
Study. Arch Intern Med. 172(4):366-7.
30 Muir, et al (2011).
Effect of vitamin D supplementation on muscle strength, gait and balance in
older adults: a systematic review and meta-analysis, J Am Geriatr Soc. 59(12):2291-300.
31 Salehpour A, et al
(2012). Vitamin D3 and the risk of CVD in overweight and obese women: a
randomised controlled trial. Br J Nutr. Feb 9 2012 [Epub ahead
of print]
32 Vacek, et al,
Vitamin D Deficiency and Supplementation and Relation to Cardiovascular
Health, Prev Cardio 2012; 109(3): 359—363.
33 Albanes, et al,
Serum 25-Hydroxy Vitamin D and Prostate Cancer Risk in a Large Nested
Case-Control Study, Canc Epidemiol Biomarkers Prev
2011; 20(9): 1850-1860.
34 Schwartz, G,
Circulating Vitamin D and Risk of Prostate Cancer — Letter, Canc Epidemiol Biomarkers Prev 2012; 21(1): 246.
35 Durup, et al, A
Reverse J-Shaped Association of All-Cause Mortality with Serum
25-Hydroxyvitamin D in General Practice, the CopD Study, J Clin Endocrinol Metab, August
2012 [Epub ahead of print]
36 Rejnmark, et al,
Vitamin D with Calcium Reduces Mortality: Patient Level Pooled Analysis of
70,528 Patients from Eight Major Vitamin D Trials, J Clin Endocrinol Metab, August 2012 [Epub ahead of print]
37 LeBlanc, et al,
Associations Between 25-Hydroxyvitamin D and Weight Gain in Elderly
Women, Journal of Women's Health, June
2012 [Epub ahead of print]
38 Holmes, et al,
Analytical Performance Characteristics of Two New Automated Immunoassays for 25
Hydroxy Vitamin D, Endocrine Soc. 2012 Meeting,
(Poster presentation)
39 Bischoff-Ferrari,
et al, A Pooled Analysis of Vitamin D Dose Requirements for Fracture
Prevention, N Engl J Med; 367:40-9.
40 Logan, et al,
Long-term vitamin D3 supplementation is more effective than vitamin D2 in
maintaining serum 25-hydroxyvitamin D status over the winter months, Br J Nutr, July 2012 [Epub ahead of
print]
41 Kabadi et
al. Joint Effects of Obesity and Vitamin D Insufficiency on Insulin
Resistance and Type 2 Diabetes: Results from the NHANES 2001-2006. Diabetes Care, 2012 [Epub ahead of print] 42 Coussens, et al, Vitamin D accelerates
resolution of inflammatory responses during tuberculosis treatment, PNAS, September 4, 2012 [Epub ahead
of print]
43 Annweiler, et al,
Higher Vitamin D Dietary Intake Is Associated With Lower Risk of Alzheimer's
Disease: A 7-Year Follow-up, J Gerontol A Biol Sci Med, April
2012 [Epub ahead of print]
Information on this site
is provided for informational purposes only. It is not an endorsement of any
product nor is it meant to substitute for the advice provided by physicians or
other healthcare professionals. The information contained herein should not be
used for diagnosing or treating a health problem or disease. Consumers should
inform their healthcare providers of the dietary supplements they take.
Latest Clinical Research Updates for Vitamin D Supplements
Vitamin D Affected by Medication
12/07/2021
A specific medication for
cystic fibrosis seems to increase the absorption of vitamin D, requiring the
adjustment to supplementation, according to a recent study. Get the details in
the Concerns and Cautions section of our
Vitamin D Supplements Review.
Sun Protection and Bone Health
11/02/2021
Does staying out of the
sun or using sunscreen increase the risk of osteoporosis or bone fracture? Find
out what a recent study suggests in the Getting vitamin D from sunlight section
of our Vitamin D Supplements Review.
10/27/2021
Does vitamin D
supplementation improve sleep or reduce insomnia in people with low blood
levels of vitamin D? See what a new study found in the What It Does section of our Vitamin D
Supplements Review.
Vitamin D Supplements: Same Dose, Different Results?
9/25/2021
Taking the same dose of
vitamin D may lead to greater increases in vitamin D status in some people than
in others, according to recent research. Find out why in the How Much Do You Need section of our
Vitamin D Supplements Review. Also see our Top Picks among vitamin D supplements.
8/10/2021
A recent study showed
that high-dose vitamin D may increase the risk of falls for certain people. Get
the details in the Muscle, Balance, and Falls section of our
Vitamin D Supplements Review.
Related CL Answers (58)