page 3 >
6a) Metabolism and Energy Production Dysfunction
A Molecular Neurobiological Approach to Understanding the Aetiology of Chronic Fatigue Syndrome Myalgic Encephalomyelitis or Systemic Exertion Intolerance Disease with Treatment Implications | SpringerLink https://link.springer.com/article/10.1007/s12035-018-0928-9#Sec9 There is now clear evidence of metabolic dysfunction in CFS/ME/SEID. As mentioned above, CFS/ME/SEID is associated with the presence of chronic O&NS, low-grade inflammation and impairment of the production of heat shock proteins 67 https://link.springer.com/article/10.1007/s12035-018-0928-9#CR67 "View reference". Naviaux and colleagues studied 45 patients and 39 age\- and sex-matched controls using targeted, broad-spectrum metabolomics and found evidence that, in this disorder, 20 examined metabolic pathways were abnormal, including those involved in mitochondrial and peroxisomal metabolism and those involved in the metabolism of branched-chain amino acids, cholesterol, phospholipids, purines, pyrroline-5-carboxylate, riboflavin, sphingolipid, as well as microbiome metabolism 68 https://link.springer.com/article/10.1007/s12035-018-0928-9#CR68 "View reference". In a more recent metabolic profiling study, abnormalities in purine, pyrimidine and amino acid metabolic pathways were found including adenosine diphosphate and ATP as well as in fatty acid and lipid metabolism 69 https://link.springer.com/article/10.1007/s12035-018-0928-9#CR69 "View reference". There is also evidence of impaired pyruvate dehydrogenase function 70 https://link.springer.com/article/10.1007/s12035-018-0928-9#CR70 "View reference", which is consistent with a shift from oxidative phosphorylation to the production of lactic acid in this disease. In their comprehensive metabolomic analyses of plasma samples from 46 CFS patients and 47 age\- and sex-matched controls, Yamano and fellow co-workers reported group differences in both the Kreb’s tricarboxylic or citric acid cycle, with lower citrate, lower *cis-aconitate*, lower isocitrate and lower malate in the patient group illustrated in Fig. 2 https://link.springer.com/article/10.1007/s12035-018-0928-9#Fig2, and in the urea cycle, with the patient group showing higher ornithine, lower citrulline and lower urea levels see Fig. 3 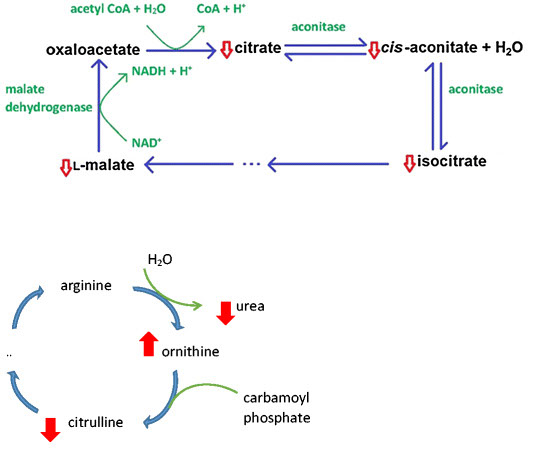 Fig. 2Metabolic changes in Kreb’s cycle reported in CFS/ME/SEID based on data in reference 71 https://link.springer.com/article/10.1007/s12035-018-0928-9#CR71 "View reference" Fig. 3Metabolic changes in the urea cycle reported in CFS/ME/SEID based on data in reference 71 https://link.springer.com/article/10.1007/s12035-018-0928-9#CR71 "View reference" From: Metabolic switch may bring on chronic fatigue syndrome | New Scientis thttps://www.newscientist.com/article/2121162-metabolic-switch-may-bring-on-chronic-fatigue-syndrome/ the condition could in many cases be due to people losing their ability to burn carbohydrate sugars in the normal way to generate cellular energy. Instead, the cells of people with CFS stop making as much energy from sugar as usual, and start relying more on lower-yielding fuels, such as amino acids and fats. This kind of metabolic switch produces lactate, which can cause pain when it accumulates in muscles. Together, this would explain both the shortness of energy, and why even mild exercise can be exhausting and painful. The levels of some amino acids in the blood of women with CFS was abnormally low – specifically for the types of amino acid that can be used by the body as an alternative fuel source. These shortfalls were not seen in men with CFS, but that could be because men tend to extract amino acids for energy from their muscles, instead of their blood. And the team saw higher levels of an amino acid that’s a sign of such a process. “It seems that both male and female CFS patients may have the same obstruction in carbohydrate metabolism to energy, but they may try to compensate differently,” says Fluge. Both sexes had high levels of several enzymes known to suppress pyruvate dehydrogenase PDH, an enzyme vital for moving carbohydrates and sugars into a cell’s mitochondria – a key step for fully exploiting sugar for energy. Fluge thinks PDH is prevented from working in people with CFS, but that it can spontaneously recover. Starvation effectSeveral studies have now hinted that defects in sugar burning can cause CFS, but there is still uncertainty over how exactly this is disrupted. However, a picture is emerging. Something makes the body switch from burning sugar to a far less efficient way of making energy. “We don’t think it’s just PDH,” says Chris Armstrong at the University of Melbourne in Australia, whose research has also uncovered anomalies in amino acid levels in patients. “Broadly, we think it’s an issue with sugar metabolism in general.” The result is not unlike starvation, says Armstrong. “When people are facing starvation, the body uses amino acids and fatty acids to fuel energy for most cells in the body, to keep glucose levels vital for the brain and muscles as high as possible.” “We think that no single enzyme in metabolism will be the answer to CFS, just as no single enzyme is the ‘cause’ of something like hibernation,” says Robert Naviaux of the University of California at San Diego, who has found depletion of fatty acids in patients suggesting they were diverted as fuel. Not psychosomaticSo what could flick the switch to a different method of metabolism? Fluge’s team thinks that a person’s own immune system may stop PDH from working, possibly triggered by a mild infection. His team has previously shown that wiping out a type of white blood cell called B-cells in CFS patients seems to relieve the condition. These white blood cells make antibodies, and Fluge suspects that some antibodies made to combat infections may also recognise something in PDH and disable it. The team is now conducting a large trial in Norway of the cancer drug rituximab, which destroys the cells that make antibodies, in people with CFS. Results are expected next year. Together, these metabolic approaches are suggesting that CFS has a chemical cause. “It’s definitely a physiological effect that we’re observing, and not psychosomatic, and I’ll put my head on the block on that,” says Armstrong. However, he adds that psychological and brain chemistry factors might be involved in some cases. Journal reference: Journal of Clinical Investigation, DOI: 10.1172/jci.insight.89376 From: Blood biomarkers may help diagnose chronic fatigue syndrome | New Scientist https://www.newscientist.com/article/2142350-blood-biomarkers-may-help-diagnose-chronic-fatigue-syndrome/ Armstrong’s own team have found that the fatigue of CFS may be caused by disrupted metabolism and energy production in the body https://www.newscientist.com/article/2121162-metabolic-switch-may-bring-on-chronic-fatigue-syndrome/. “The metabolic changes we found suggest a physiological stressor in the body is affecting the cells,” he says. “The cause of that stress is unknown, but is likely to be immune-based given the mounting evidence in that direction – this new study included.” A team in Norway has had some early success in treating CFS by targeting the immune system and reducing inflammation https://www.newscientist.com/article/dn27813-antibody-wipeout-found-to-relieve-chronic-fatigue-syndrome/. They have been using a drug called rituximab to wipe out the white blood cells that may make inflammatory antibodies. Montoya says it’s unclear what causes the increase in cytokines they have seen in CFS, but he thinks something is triggering inflammation in the body – possibly an infection like the herpes virus. From: ME/CFS, a mathematical model – paolo maccallini https://paolomaccallini.wordpress.com/2018/07/10/me-cfs-a-mathematical-model/
Fig. 2Metabolic changes in Kreb’s cycle reported in CFS/ME/SEID based on data in reference 71 https://link.springer.com/article/10.1007/s12035-018-0928-9#CR71 "View reference" Fig. 3Metabolic changes in the urea cycle reported in CFS/ME/SEID based on data in reference 71 https://link.springer.com/article/10.1007/s12035-018-0928-9#CR71 "View reference" From: Metabolic switch may bring on chronic fatigue syndrome | New Scientis thttps://www.newscientist.com/article/2121162-metabolic-switch-may-bring-on-chronic-fatigue-syndrome/ the condition could in many cases be due to people losing their ability to burn carbohydrate sugars in the normal way to generate cellular energy. Instead, the cells of people with CFS stop making as much energy from sugar as usual, and start relying more on lower-yielding fuels, such as amino acids and fats. This kind of metabolic switch produces lactate, which can cause pain when it accumulates in muscles. Together, this would explain both the shortness of energy, and why even mild exercise can be exhausting and painful. The levels of some amino acids in the blood of women with CFS was abnormally low – specifically for the types of amino acid that can be used by the body as an alternative fuel source. These shortfalls were not seen in men with CFS, but that could be because men tend to extract amino acids for energy from their muscles, instead of their blood. And the team saw higher levels of an amino acid that’s a sign of such a process. “It seems that both male and female CFS patients may have the same obstruction in carbohydrate metabolism to energy, but they may try to compensate differently,” says Fluge. Both sexes had high levels of several enzymes known to suppress pyruvate dehydrogenase PDH, an enzyme vital for moving carbohydrates and sugars into a cell’s mitochondria – a key step for fully exploiting sugar for energy. Fluge thinks PDH is prevented from working in people with CFS, but that it can spontaneously recover. Starvation effectSeveral studies have now hinted that defects in sugar burning can cause CFS, but there is still uncertainty over how exactly this is disrupted. However, a picture is emerging. Something makes the body switch from burning sugar to a far less efficient way of making energy. “We don’t think it’s just PDH,” says Chris Armstrong at the University of Melbourne in Australia, whose research has also uncovered anomalies in amino acid levels in patients. “Broadly, we think it’s an issue with sugar metabolism in general.” The result is not unlike starvation, says Armstrong. “When people are facing starvation, the body uses amino acids and fatty acids to fuel energy for most cells in the body, to keep glucose levels vital for the brain and muscles as high as possible.” “We think that no single enzyme in metabolism will be the answer to CFS, just as no single enzyme is the ‘cause’ of something like hibernation,” says Robert Naviaux of the University of California at San Diego, who has found depletion of fatty acids in patients suggesting they were diverted as fuel. Not psychosomaticSo what could flick the switch to a different method of metabolism? Fluge’s team thinks that a person’s own immune system may stop PDH from working, possibly triggered by a mild infection. His team has previously shown that wiping out a type of white blood cell called B-cells in CFS patients seems to relieve the condition. These white blood cells make antibodies, and Fluge suspects that some antibodies made to combat infections may also recognise something in PDH and disable it. The team is now conducting a large trial in Norway of the cancer drug rituximab, which destroys the cells that make antibodies, in people with CFS. Results are expected next year. Together, these metabolic approaches are suggesting that CFS has a chemical cause. “It’s definitely a physiological effect that we’re observing, and not psychosomatic, and I’ll put my head on the block on that,” says Armstrong. However, he adds that psychological and brain chemistry factors might be involved in some cases. Journal reference: Journal of Clinical Investigation, DOI: 10.1172/jci.insight.89376 From: Blood biomarkers may help diagnose chronic fatigue syndrome | New Scientist https://www.newscientist.com/article/2142350-blood-biomarkers-may-help-diagnose-chronic-fatigue-syndrome/ Armstrong’s own team have found that the fatigue of CFS may be caused by disrupted metabolism and energy production in the body https://www.newscientist.com/article/2121162-metabolic-switch-may-bring-on-chronic-fatigue-syndrome/. “The metabolic changes we found suggest a physiological stressor in the body is affecting the cells,” he says. “The cause of that stress is unknown, but is likely to be immune-based given the mounting evidence in that direction – this new study included.” A team in Norway has had some early success in treating CFS by targeting the immune system and reducing inflammation https://www.newscientist.com/article/dn27813-antibody-wipeout-found-to-relieve-chronic-fatigue-syndrome/. They have been using a drug called rituximab to wipe out the white blood cells that may make inflammatory antibodies. Montoya says it’s unclear what causes the increase in cytokines they have seen in CFS, but he thinks something is triggering inflammation in the body – possibly an infection like the herpes virus. From: ME/CFS, a mathematical model – paolo maccallini https://paolomaccallini.wordpress.com/2018/07/10/me-cfs-a-mathematical-model/
Close window by clicking in grey area >